Nader Saki1, Soheila Nikakhlagh1*, Lila Mashali2, Soad Fazeli3
1Associated professor of otolaryngology, Head and neck surgery, Hearing and Speech Research Center, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran 2Assistant Prof. of otolaryngology, Head and neck surgery, Hearing and Speech Research Center, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran 3Medical Student, Hearing and Speech Research Center, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran *Corresponding author Email: nikakhlagh.s@gmail.com
Abstract
Generally in any parotid surgery it is necessary to identify the trunk and branches of the facial nerve. For damage to this nerve or its branches may have irreparable consequences. The purpose of this study was to evaluate the frequency of anatomical variation of facial nerve branching in patients undergoing parotid surgery. 94 patients undergone parotid surgery in Imam Khomeini Hospital of Jondishapur University of Ahvaz from September 2011 to September 2014 were studied. All patients had benign unilateral parotid surgery. During surgery and dissection, the parotid glands of the patients were photographed and the anatomy of the facial nerve and its branches in the parotid glands of patients were interpreted. The schematic picture of the anatomy of the facial nerve within the parotid gland was drawn. The images were divided into three groups: type A, B and C. The number of patients with a variety of nerve type A was 25, type B, 47 and type C, 22. The comparison between the nerve and sex using the Chi-square test showed that there is no significant relationship between gender and type of nerve (P value = 0.6). The range of the patients’ age was 25-65 years. In this study no new landmark was found and of the 94 patients, 25 (26%) were type A, 47 (50%) type B and 22 (24%) type C. In the parotid surgery, if the anatomical variation of facialnerve is kept in the mind, theadverse effectsand damage tothe facial nerveand its branches can beavoided. More accurateand completestudyof theanatomicalnervebranching can benefitalltypes of surgeryinvolvedin thearea.
Keywords
Parotid Gland Tumor; Facial Nerve; Anatomical Variation of Branches
Download this article as:| Copy the following to cite this article: Saki N, Nikakhlagh S, Mashali L, Fazeli S. Pattern of Distribution in Facial Nerve in the Benign Parotid Gland Tumors. Biomed Pharmacol J 2015;8(March Spl Edition) |
| Copy the following to cite this URL: Saki N, Nikakhlagh S, Mashali L, Fazeli S. Pattern of Distribution in Facial Nerve in the Benign Parotid Gland Tumors. Biomed Pharmacol J 2015;8(March Spl Edition). Available from: http://biomedpharmajournal.org/?p=2298> |
Introduction
The facial motor nerve is a very important anatomical and surgical element in the head and neck surgery. Its anatomical knowledge is very important for various reasons. This nerve usually has five branches and a complicated anatomy. In addition, its anatomical variety and branches are great. In the parotid gland surgery, it is necessary to describe the ear and the traumatic lesions of the parotid fully or partially to avoid its damage (1-3). The most common causes of paralysis of this nerve are the iatrogenic injury during surgery of the mandibular and parotid regions (4-6). Damage to the facial nerve is usually irreversible and irreparable. Except in a limited way, and with some techniques, the nerve function improves. The terminal branches of the facial nerve are associated with parotid gland and pass through the center of the gland, so the anatomy of facial nerve and its relationship with the parotid gland is very important. For example parotid cancer with more than 4cm is situated exactly on the facial nerve main trunk. So because of the little space between the mastoid process and the cancerous parotid gland, working on this area is extremely difficult (7). Another example of the importance of a full identification of facial nerve is in parotid gland surgery, in which the parotid gland is close to the extra-cranial region of the facial nerve (8). generally in any parotid surgery, the identification of the facial nerve trunk is a need. Damage to this nerve or pulling it may result in irreparable consequences (9). The full anatomical knowledge of this nerve is essential for preventing its damage and facial muscle paralysis. The purpose of this study was to recognize the frequency of anatomical variations of facial nerve and its branches in patients undergoing parotid surgery.
Materials and Methods
94 patients undergoing parotid surgery in Ahwaz Imam Khomeini Hospital from September 2011 to September 2014 were studied. This study was approved by the ethics committee of the University. Information on age and sex of the patients were recorded. All patients had unilateral benign parotidectomy. The number of male patients was 51 and female patients, 43. The average of patients’ age 25-65 years old was calculated. During surgery photographs were taken from the parotid gland dissection and facial nerve anatomy in patients with parotid gland was interpreted. Information about pattern of the facial nerve branching and other anatomical findings in the parotid gland associated with facial nerve that can be a new landmark for identifying the nerve was extracted. Schematic illustrations of the anatomical variation of facial nerve and its branches within the parotid gland were drawn. The images were divided into three groups: type B, A and C. Results in the presence or absence of new landmarks, the frequency and percentage of relative frequency of each of the images, display of the pattern of facial nerve were reported. The relationship between the frequency of nerve branches and gender categories were analyzed by Chi-square test.
Results
Totally 94 patients underwent unilateral parotid surgery. The patients were examined in terms of the anatomical variation of the facial nerve branching. Patients with variation nerve type A were 25. Type B, 47 and type C, 22. The comparison between the nerve and sex using the Chi-square test showed that there is no significant relationship between gender and the type of nerve (P value = 0.6). Age range of the patients was 25 to 65 years old. In this study, a new landmark was not found. Of 94 patients, 25 (26%) were type A, 47 (50%) type B and 22 (24%) type C was observed. Figure 1 shows the frequency of facial nerve branching anatomical variation observed in 94 patients.
Table 1:The frequency of facial nerve branches variation in terms of gender
| Frequency (%) | Facial nerve | Sex |
| 13 (25%) | A | Male (n= 51) |
| 25 (49%) | B | |
| 13 (25%) | C | |
| 12(27.9%) | A | Female (n= 43) |
| 22 (51.2%) | B | |
| 9 (20.9%) | C |
Table 2: The frequency of two and three branches of the facial nerve in different studies
| Trifurcation (%) | Bifurcation (%) | Sample size (N) | Author |
| – | 100 | 350 | Davis et al., 1956 (10) |
| 4.4 | 95.6 | 111 | Park and Lee, 1977 (11) |
| – | 100 | 100 | Katz and Catalano, 1987 (12) |
| 18 | 82 | 50 | Kopuz et al., 1994 (13) |
| 18.6 | 81.4 | 27 | Ekinci, 1999 (14) |
| 2.2 | 97.8 | 46 | Salame et al., 2002 (15) |
| – | 100 | 108 | Tsai and Hsu, 2002 (16) |
| 13.3 | 86.7 | 30 | Kwak et al., 2004 (17) |
| 18.7 | 81.3 | Kalycioglu et al., 2014 (18) | |
| 24 | 76 | 94 | Present Study |
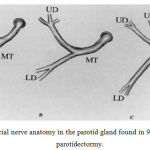 |
Figure 1: The facial nerve anatomy in the parotid gland found in 94 patients underwent parotidectormy. |
MT, Main trunk; UD, upper division; LD, lower division
- A) Where the upper and lower trunks of the facial nerve divide, closely followed by the bifurcation of the marginal and cervical branches.
- B) Where the upper and lower trunks divide and then branch into their respective divisions.
- C) Branching of the upper division immediately after the bifurcation of the upper and lower divisions
Discussion
The parotid surgery success depends on identifying and preserving the facial nerve (2), so perfect knowledge of the nerve and its variable branches is necessary. In the study of Farooq Ahmed and his colleagues, 57 parotid glands were dissected, from which 5/89% of the facial nerve are divided into five types and 5/10% are not included in any of these types. In All these types, the trunk of the facial nerve in parotid gland is divided into the upper and the lower branches. Higher types have greater complexity in terms of the number of the branches of the facial nerve and the relationships between them (19). The types of the present study are not similar to the types described in the study carried out by Farooq et al. Among 94 patients with parotid surgery, three types of nerve were identified (Fig 1). The highest frequency is related to nerve type B (50%). Nerve type C in the present study, has not been reported in any of the previous studies. In nerve type C after the nerve trunk, the facial nerve is divided into three branches (Fig 1-C). In most of the previous studies, the schematic drawing of the facial nerve was divided into 5 types. In different studies the frequency of each of the identified schematic drawings found in the studied samples were reported. In addition, no relationship was found between gender and anatomic nerve (P value= 0.6). This finding is consistent with study carried out by Kalycioglu et al. concerning bifurcation and trifurcation of facial nerve, in our study, bifurcation was of a higher frequency. In other studies, bifurcation was also the most frequent (Table 2). However in some of the facial nerve studies, trifurcation was not found (10-19).
Conclusion
If we get familiar with the different facial nerve branching during the surgery of the parotid gland, the adverse effects of damage to this nerve and its branches can be avoided. More accurate and more complete studies of the anatomy and the branching of this nerve will be beneficial to all types of surgery involved in its area.
Acknowledgment
The present study is result of the General partitioning Thesis Number D/1747. Thus I would like to thank the Deputy of Research and Technology, Ahvaz Jundishapur University of Medical Sciences for their great support.
References
- Gupta S, Mends F, Hagiwara M, Fatterpekar G, Roehm PC. Imaging the facial nerve: a contemporary review. Radiology research and practice. 2013;2013:248039. Epub 2013/06/15.
- Harris TJ. Localization of the facial nerve in parotid surgery. ANZ journal of surgery. 2001;71(12):701-2. Epub 2002/03/22.
- Wong DS. Surface landmarks of the facial nerve trunk: a prospective measurement study. ANZ journal of surgery. 2001;71(12):753-6. Epub 2002/03/22.
- Batra AP, Mahajan A, Gupta K. Marginal mandibular branch of the facial nerve: An anatomical study. Indian journal of plastic surgery : official publication of the Association of Plastic Surgeons of India. 2010;43(1):60-4. Epub 2010/10/07.
- O’Brien CJ. Facial nerve localization in parotid surgery. ANZ journal of surgery. 2002;72(5):370. Epub 2002/05/25.
- Toure S, Vacher C, Bertrand JC. [Anatomy of the marginal mandibular branch of the facial nerve]. Revue de stomatologie et de chirurgie maxillo-faciale. 2004;105(3):149-52. Epub 2004/06/24. Etude anatomique du rameau marginal de la mandibule du nerf facial.
- Yokoyama J, Ooba S, Fujimaki M, Anzai T, Kojima M, Ikeda K. Impact of removing mastoid process for advanced parotid cancer on facial nerve identification, preservation and reconstruction. Head and face medicine. 2014;10:6. Epub 2014/03/05.
- Sharma R, Sirohi D. Proximal and distal Facial nerve exploration during superficial parotidectomy. Journal of maxillofacial and oral surgery. 2010;9(2):150-4. Epub 2010/06/01.
- Saha S, Pal S, Sengupta M, Chowdhury K, Saha VP, Mondal L. Identification of facial nerve during parotidectomy: a combined anatomical and surgical study. Indian journal of otolaryngology and head and neck surgery : official publication of the Association of Otolaryngologists of India. 2014;66(1):63-8. Epub 2014/03/08.
- Davis RA, Anson BJ, Budinger JM, Kurth LR. Surgical anatomy of the facial nerve and parotid gland based upon a study of 350 cervicofacial halves. Surgery, gynecology and obstetrics. 1956;102(4):385-412. Epub 1956/04/01.
- Park IY, Lee ME. A morphological study of the parotid gland and the peripheral branches of the facial nerve in Koreans. Yonsei medical journal. 1977;18(1):45-51. Epub 1977/01/01.
- Katz AD, Catalano P. The clinical significance of the various anastomotic branches of the facial nerve. Report of 100 patients. Archives of otolaryngology–head and neck surgery. 1987;113(9):959-62. Epub 1987/09/01.
- Kopuz C, Turgut S, Yavuz S, Ilgi S. Distribution of facial nerve in parotid gland: analysis of 50 cases. Okajimas folia anatomica Japonica. 1994;70(6):295-9. Epub 1994/03/01.
- Ekinci N. A study on the branching pattern of the facial nerve of children. Kaibogaku zasshi Journal of anatomy. 1999;74(4):447-50. Epub 1999/09/25.
- Salame K, Ouaknine GER, Arensburg B, Rochkind S. Microsurgical anatomy of the facial nerve trunk. Clinical Anatomy. 2002;15(2):93-9.
- Tsai SC-S, Hsu H-T. Parotid neoplasms: diagnosis, treatment, and intraparotid facial nerve anatomy. The Journal of Laryngology and Otology. 2002;116(05):359-62.
- Kwak HH, Park HD, Youn KH, Hu KS, Koh KS, Han SH, et al. Branching patterns of the facial nerve and its communication with the auriculotemporal nerve. Surg Radiol Anat. 2004;26(6):494-500.
- Kalaycioglu A, Yeginoglui G, Ertemoglu Oksuz C, Uzun O, Kalkisim SN. An anatomical study on the facial nerve trunk in fetus cadavers. Turkish journal of medical sciences. 2014;44(3):484-9. Epub 2015/01/07.
- Farooq Ahmed FA, Muhammed Ehsanul Haque, Riaz Ahmad, Imran Ahmed, Nabila Kaukab. Facial nerve; pattern of distribution in the parotid gland. Professional Med J. 2005;12(1):85-90.







