Mozafar Sarafraz1, Nader Saki1*,Soheila Nikakhlagh1, Mahyar Maleki2, Reza Shikhpour Jonaky3
1Associated professor of otolaryngology, Head and neck surgery, Hearing and Speech Research Center, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran 2Resident of otolaryngology, Head and neck surgery, Hearing and Speech Research Centre, Ahvaz 3General Physcian, Cancer Research Center, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran
Abstract
The aim of the present study was to determine the audiometric pattern of patients suffering from presbycusis. Moreover, we tried to give an overview of affected patients in regard to age, gender, and concomitant diseases. In this prospective descriptive study we investigate the audiometric patterns of presbycusis patients older than 60 years attending the otolarygology clinic of Imam Khomeini Hospital, Ahvaz, Iran. Moreover, a questionnaire about past medical history of all participants in regard to ear and hearing disorders and risk factors were obtained. A screening tympanogram and otoscopic evaluation were performed by an otolaryglogist before the enrolling the subject to the study. Our findings showed that the sensory pattern is the most frequent kind of presbycusis (64.29%), followed by neural, conductive, metabolic and sensory-neural with a frequency of 16.25%, 9.54%, 2.68% and 7.16% respectively. Tinnitus was detected is over 60 percent of participants. Presbycusis did not have significantly higher rates in smokers or patients with positive history of hypertension ( P=0.245, P=0.249). In this study the most frequent audiometric pattern was sensory and there was no significant difference between presbycusis and smoking or hyprtention.
Keywords
Audiometry; Presbycusis; Age-Related Hearing Loss; Elderly
Download this article as:| Copy the following to cite this article: Sarafraz M, Saki N, Nikakhlagh S, Maleki M, Jonaky R. S. Distribution of Audiometric Findings in Patients with Presbycusis. Biomed Pharmacol J 2015;8(March Spl Edition) |
| Copy the following to cite this URL: Sarafraz M, Saki N, Nikakhlagh S, Maleki M, Jonaky R. S. Distribution of Audiometric Findings in Patients with Presbycusis. Biomed Pharmacol J 2015;8(March Spl Edition). Available from: http://biomedpharmajournal.org/?p=2271> |
Introduction
Presbycusis, age-related hearing loss (ARHL), is an inevitable deterioration in hearing ability which gradually occurs in most individuals as they grow up [1]. After hypertension and arthritis, ARHL is the third most common chronic disease among people aged over 65 years, [2].
Presbycusis by definition is a progressive bilateral symmetrical age-related hearing loss [3]. Although its etiology is not well known, previous studies suggested various types of physiological degeneration, environmental factors (i.e. noise exposure and ototoxic agents), and genetic susceptibility as the affecting causes. ARHL should be considered as a major public health problem, since it has diverse adverse effects on quality of life, cognitive, emotional and social functions of the older adults [4, 5]. The prevalence of hearing loss seems to be growing by age, from 40-60% in the 60s to over 80% in people older than 85 [6]. It could be detected in both men and women but the hearing loss showed different patterns among either genders previously [1, 7].
The association between ARHL and tinnitus, smoking and several chronic diseases have been evaluated before [2, 8, 9]. Besides, concomitant factors including; dyslipidemia, hypertension would aggregate the progression of presbycusis [2].
In spite of high prevalence and potential adverse effects of presbycusis, unfortunately it is still a diagnose dilemma. Schuknecht, et al. categorised presbycusis based on pathology and audiometric findings into sensory, neural, conductive, and metabolic(strial) types. Sensory presbycusis is defined as epithelial atrophy and loss of sensory hair cells and supporting cells of the organ of Corti, which is begun from the base and progress towards the apex. In this type slope of the audiogram occurs in the high frequencies therefore the speech discrimination is preserved. Neural presbycusis is result from nerve cells atrophy in the cochlea and central neural pathway. Atrophy occurs throughout the cochlea with no precipitous drop in high-frequency threshold in the audiogram. The speech discrimination severely decreases even before hearing loss is noted. Conductive or mechanical type stems from thickening and secondary stiffening of the basilar membrane of the cochlea with a gradual sloping high-frequency sensorineural hearing loss. Speech discrimination is preserved in this type. Atrophy of stria vascularis result in metabolic or strial presbycusis which affect the entire cochlea and show a flat curve in the audiogram.
The aim of the present study was to determine the audiogram pattern of patients suffering from presbycusis. Moreover, we tried to give an overview of affected patients in regard to age, gender, and concomitant diseases.
Materials and Methods
This descriptive prospective study was conducted during March 2010 to March 2012 in Imam Khomeini Hospital, Ahvaz, Iran. Eligible subjects were all patients older than 60 years old with hearing disorders attending to the otolarygology clinic of Imam Khomeini Hospital. All participants first were evaluated by an otolaryngologist . Patients with any abnormal findings i.e tympan tearing, otosclerosis, and otitis serous were excluded. Then a questionnaire was completed for each participant. The hearing examination included an otoscopic evaluation, a screening tympanogram and pure-tone air- and bone-conduction assessments.
A questionnaire about the ear and hearing-related medical and surgical history, noise exposure, acoustic trauma, congenital disorders, previous history of using ototoxic agent, smoking, and hypertension was administered as an interview for all subjects.
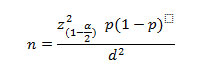
The sample size was calculated using the following equation:
where Prevalence (p) and difference (d) based on Gate, et al was 0.37 and 0.05, respectively [1]. The frequency of different type of presbycusis was calculated. The Chi-squard test was used for analysis of qualitative variables. All reported P-values less than 0.05 were considered as statistically significant.
Results
Five hundred and sixty patients over the age of 60 (315 male and 245 female) were evaluated in four different age groups (Table 1).
The sensory pattern was the most frequent one, which was detected in 360 (64.29%) of patients. It followed by neural, conductive and metabolic patterns in 91 (16.25%), 54 (9.54%), and 15 (2.68%) patients respectively. Forty patients (7.14%) showed a combination of sensory and neural pattern in audiometry. Recent group had normal hearing ability in low and medium frequencies, but showed a severe hearing loss in high frequencies. Besides, the speech discrimination was impaired in this group.
The majority of patients, 339 (60.5%), complained of tinnitus. This compliant was associated with sensory-neural hearing loss the most (72.5%) (Table.2)
A sensory-neural pattern was more frequent among females (55%), while four other patterns showed a higher frequency in men ( Table 3).
Smoking and hypertension were more accompanied by conductive pattern, 87 (15.5%) and 255 (45.5%) respectively. Metabolic presbycusis patients had no smoking history. There were no significant differences between smoking and presbycusis (P=0.245). The least frequent audiometric pattern in hypertensive patients was sensory presbycusis. The association between hypertension and presbycusis was not statistically significant (P=0.249) (Figure 1,2).
Table 1: The age distribution of presbycusis audiometric patterns
| Audiometric pattern | Age* | ||||
| 60-69 | 70-79 | 80-89 | 90-99 | Total | |
| Sensory | 263(73.1%)** | 78(21.7%) | 19(5.3%) | 0(0%) | 360(100%) |
| Neural | 46(50.5%) | 23(25.3%) | 18(19.8%) | 4(4.4%) | 91(100%) |
| Conductive | 18(33.3%) | 25(46.3%) | 11(20.4%) | 0(0%) | 54(100%) |
| Metabolic | 11(73.3%) | 4(26.7%) | 0(0%) | 0(0%) | 15(100%) |
| Sensory-Neural | 23(57.5%) | 17(42.5%) | 0(0%) | 0(0%) | 40(100%) |
| Total | 361(64.5%) | 147(26.3%) | 48(8.6%) | 4(0.7%) | 560(100%) |
* Years
** Number(percent)
Table 2: The association between tinnitus and audiometric patterns
| Audiometric pattern | Tinnitus* | ||
| Present | Abscent | Total | |
| Sensory | 220(61.1%)** | 140(38.9%) | 360(100%) |
| Neural | 45(49.5%) | 46(50.5%) | 91(100%) |
| Conductive | 38(70.4%) | 16(29.6%) | 54(100%) |
| Metabolic | 7(46.7%) | 8(53.3%) | 15(100%) |
| Sensory-Neural | 29(72.5%) | 11(27.5%) | 40(100%) |
| Total | 339(60.5%) | 221(39.5%) | 560(100%) |
*Number(percent)
Table 3: The gender distribution of different audiometric patterns
| Audiometric pattern | Gender | ||
| Male | Female | Total | |
| Sensory | 209(58.1%)* | 151(41.9%) | 360(100%) |
| Neural | 48(52.7%) | 43(47.3%) | 91(100%) |
| Conductive | 29(53.7%) | 25(46.3%) | 54(100%) |
| Metabolic | 11(73.3%) | 4(26.7%) | 15(100%) |
| Sensory-Neural | 18(45.0%) | 22(55.0%) | 40(100%) |
| Total | 315(56.3%) | 245(43.8%) | 560(100%) |
*Number(percent)
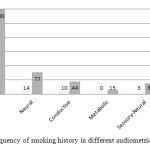 |
Figure 1: Frequency of smoking history in different audiometric patterns |
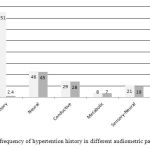 |
Figure 2: frequency of hypertention history in different audiometric patterns |
Discussion
The population older than 60 years is going to increase at a fast rate during coming decades. Both peripheral and central auditory systems affect by advancing age. ARHL gradually progress and leads to social isolation of the elderly population. There are supporting data about the association between presbycusis and the cognitive decline [10-12].
The findings of the present study suggest that the most frequent presbycusis pattern in our studied population was sensory (64.29%), which is defined as the hearing loss in low and medium frequencies. Baradli, et al. (2005) studied 211 elderly patients and revealed that the major decrease in low frequency hearing loss occurs in the 90s and older, but high-frequencies hearing loss occur before mentioned age [13].
Presbycusis is a common cause of tinnitus and 60.5% of our participants present this symptom. This result is in a line with Do Carmo et al. (2008) survey in Brazil which reported 72.5% and 64.4% tinnitus in male and female population respectively [7].
Cruickshank et al. (1998) in an epidemiological study of hearing loss reported that current smokers had 1.69 times more hearing loss than nonsmokers. Besides, nonsmoking participants who lived with a smoker were more likely to have a hearing loss than those who were not exposed to a household member who smoked. But our results showed no statistically significant relationship between smoking and presbycusis.
Gate GA et al. investigated the relationship between cardiovascular disease and hearing status in the elderly and they revealed that there is a statistically significant relationship between these two factors [14]. In the present study the relationship between hypertension and presbycusis was investigated, which was not statistically significant (P =0.249).
In conclusion in this study the most frequent audiometric pattern was sensory and there was no significant difference between presbycusis and smoking or hypertension.
Acknowledgement
This study was DR.Reza.Sheikhpour Joneki postgraduate thesis and was supported by a grant from Ahvaz Jundishapour University of medical sciences.
Conflict of interest
There is no conflict of interest to be declared
Refrences
- Gates, G.A. and J.H. Mills, Presbycusis. The Lancet. 366(9491): p. 1111-1120.
- Cruickshanks, K.J., et al., Prevalence of hearing loss in older adults in Beaver Dam, Wisconsin The Epidemiology of Hearing Loss Study. American Journal of Epidemiology, 1998. 148(9): p. 879-886.
- Schuknecht, H.F. and M.R. Gacek, Cochlear pathology in presbycusis. The Annals of otology, rhinology, and laryngology, 1993. 102(1 Pt 2): p. 1-16.
- Mulrow, C.D., et al., Association between hearing impairment and the quality of life of elderly individuals. Journal of the American Geriatrics Society, 1990.
- Huang, Q. and J. Tang, Age-related hearing loss or presbycusis. European Archives of Oto-Rhino-Laryngology, 2010. 267(8): p. 1179-1191.
- Frisina, S.T., et al., Characterization of hearing loss in aged type II diabetics. Hearing research, 2006. 211(1): p. 103-113.
- do Carmo, L.C., et al., Audiological study of an elderly Brazilian population. Brazilian journal of otorhinolaryngology, 2008. 74(3): p. 342.
- Rosenhall, U. and A.-K. Karlsson, Tinnitus in old age. Scandinavian Audiology, 1991. 20(3): p. 165-171.
- Cruickshanks, K.J., et al., Cigarette smoking and hearing loss. JAMA: the journal of the American Medical Association, 1998. 279(21): p. 1715-1719.
- Parham, K., et al., Challenges and opportunities in presbycusis. Otolaryngology–Head and Neck Surgery, 2011. 144(4): p. 491-495.
- Parham, K., et al., Comprehensive Management of Presbycusis Central and Peripheral. Otolaryngology–Head and Neck Surgery, 2013. 148(4): p. 537-539.
- Arlinger, S., Audiometric profile in presbycusis. Acta Oto-Laryngologica, 1991. 111(S476): p. 85-90.
- Baraldi, G.d.S., L.C.d. Almeida, and A.C.d.C. Borges, Hearing loss in aging. Revista Brasileira de Otorrinolaringologia, 2007. 73(1): p. 64-70.
- Gates, G.A., et al., The relation of hearing in the elderly to the presence of cardiovascular disease and cardiovascular risk factors. Archives of Otolaryngology—Head and Neck Surgery, 1993. 119(2): p. 156.