Ndubuisi N. Nwobodo1* and Paul O. Okonkwo2
1Department of Pharmacology and Therapeutics, Ebonyi State University, Abakaliki, Nigeria. 2Department of Pharmacology and Therapeutics, University of Nigeria.
DOI : https://dx.doi.org/10.13005/bpj/516
Abstract
The efficacy of amodiaquine in the malaria endemic region of sub-Saharan Africa has declined. The use of serum lipid lowering agents as part of management protocol for treatment of malaria infection has been advocated. The aim of present study was to evaluate the clinical response of amodiaquine plus simvastatin combination in relation to amodiaquine alone in the treatment of malaria infection. Subjects with frank malaria (n=60) diagnosed by thick blood film and immunological tests were nominated for the study. Informed written content was obtained and subjects randomized into amodiaquine plus simvastatin (test) and amodiaquine alone (control) groups. The ethical clearance certificate was obtained from the University of Nigeria Teaching Hospital Research Ethics Committee (NHREC/05/01/2008B). The assessment of clinical response was done in line with WHO criteria and patients followed up on days D3, D7, D14 and D28 post-treatment. The GraphPad Prism 4.0 was employed in the analysis of data which was presented as tables and graphs. Statistically significant decrease in the mean early treatment failure given as 2.5±0.11% in the test group relative to 12.5±0.11% reported in the control; similarly the mean late treatment failure given as 7.2±0.34% in the test group was decreased relative to 20.3±0.17% in the control. A statistically significant increase was reported in adequate clinical and parasitological response given as 90.3±0.55% in the test group relative to 67.2±0.45% in the control. There was statistically significant reduction in the mean parasite clearance time in the test group given as 2.8±0.19 days relative to 6.3±0.27days in the control. Similarly, the fever clearance time given as 24.3±1.13 hours was significantly reduced relative to 66 ±2.1 hours rported in the control. A statistically significant increase in the clinical clearance rate given as 96.3±0.5% was recorded in the test group as compared to the 71.6±2.1% recorded in the control. A statistically significant decrease in the recrudescence rate given as 6.4±0.0.1% in the test group relative to 13.6±0.16% in the control was also reported. Evidently, the enhanced clinical response obtained in the test subjects relative to control in present study, can only be attributed to the modulating influence of the HMG-CoA reductase inhibitor, simvastatin.
Keywords
Amodiaquine; Clinical response; Falciparum malaria; Statin; Treatment failure
Download this article as:| Copy the following to cite this article: Nwobodo N. N, Okonkwo P. O. Statin Treatment Modulates Clinical Response to Amodiaquine in Acute Uncomplicated Falciparum Malaria. Biomed Pharmacol J 2014;7(2) |
| Copy the following to cite this URL: Nwobodo N. N, Okonkwo P. O. Statin Treatment Modulates Clinical Response to Amodiaquine in Acute Uncomplicated Falciparum Malaria. Biomed Pharmacol J 2014;7(2). Available from: http://biomedpharmajournal.org/?p=3066 |
Introduction
Amodiaquine is a 4-aminoquinoline compound (4-[(7-chloroquinoline-4-oyl) amino]-2-(diethyl aminomethylphenol) similar in structure and activity to chloroquine and exhibiting clinical efficacy against the parasite despite high parasitological resistance1,2. Studies have revealed decreasing efficacy of amodiaquine in the malaria endemic region of sub-Saharan Africa3,4. It has been shown that chlorpheniramine in combination with amodiaquine was significantly more effective than amodiaquine alone in the treatment of acute uncomplicated malaria5. The lipogenesis-inducing activity in the lipid fractions of boiled supernatant of Plasmodium falciparum cultures with subsets of T-lymhocytes being affected at an early stage during paroxysms of non-endemic malaria infection has been demonstrated6,7. It has been shown that Plasmodium falciparum glycosylphosphatidylinositols (GPIs) stimulate the production of tumor necrosis factor alpha (TNF-α) in macrophages through mainly toll-like receptor2 (TLR-2) activation and to a lesser extent through TLR-4 activation8,9. Simvastatin has been reported to reduce levels of TNF- α and interleukin-1β10,11 . Consequently, it is hypothesized that simvastatin in combination with amodiaquine significantly improves clinical response compared to amodiaquine alone in the treatment of malaria infection.
Materials and Methods
Subjects: Subjects with acute malaria (n=60) in attendance at eight primary health facilities were selected for this study. Malaria infection was diagnosed using thick blood films and confirmed by immunological test (Paracheck PI®) . Paracheck PI®, a rapid qualitative two site sandwich immunochromatographic dipstick assay, was employed for the determination of Plasmodium falciparum specific histidine rich protein-2 (PfHRP-2) in whole blood samples. This was considering the fact that classical method of diagnosis by microscopy involving examination of thin and thick blood smears was prone to false negative readings and time consuming.
Study Design: Informed consent was obtained after adequate explanation of the purpose of study, formal written documentation , type of treatment to be administered and clarification of any likely adverse effects or complication that may arise in the course of treatment. Patients enrolled for this study were within the age range 16 to 65 years inclusive, in attendance at eight primary health facilities within Asu Nkanu Local Health Authority in Nkanu East Local Government Area of Enugu State, Nigeria. Routine clinical clerkship and examination including body weight measurement and axillary temperature were carried out to confirm the enrollee’s physical condition and ascertain presence of any confounding ailment. Subjects were randomised into test and control groups using a table of random numbers statistically generated. No member of the research team including the principal investigator, microscopist, field supervisor, field assistants, medical officer and nurses involved in the study had any prior knowledge of the patients’ medical records nor the treatment group to which any enrollee was assigned. The ethical clearance certification was given by the Institutional Research Ethics Review Committee of the University of Nigeria Teaching Hospital, Ituku-Ozalla, Nigeria (Ref: NHREC/05/01/2008B) in line with principles guiding human experimentation as enumerated in the Declaration of Helsinki by the World Medical Association General Assembly as last amended (Seoul 2008); while approval for the study was obtained from Enugu State Ministry of Health, Enugu-Nigeria. Amodiaquine (Camoquin® from Pfizer West-Africa, Dakar-Nigeria) was given as 15mg/kg at initial presentation D0, then 10mg/kg daily for D1 and D2. Simvastatin (Simvor® from Ranbaxy Laboratories, Dewas-India) was given orally in the dosage 0.6mg/kg/d only in the evening for 3 consecutive days. The control group received Amodiaquine only in same dose as test group. Artemether-Lumefantrine (Coartem®from Novartis Pharma AG, Basel-Switzerland) was used to salvage subjects who presented with recrudescence or treatment failure and eventually withdrawn from the study. The Artemether component was given as 3.2mg/kg/d while the Lumefantrine as 19.2 mg/kg/d respectively in two divided doses for 3 days. Baseline monitoring of liver function tests was done before commencement and in the course of therapy. The discontinuation of simvastatin would be indicated following elevation of serum transaminase activity up to three times normal level.
Assessment of Response: The patients were followed up on days D0, D3, D7, D14 and D28. The categorization of therapeutic response was done as follows in line the World Health Organisation (WHO) criteria as follows:
Early Treatment Failure (ETF): Development of danger signs of severe malaria on D1-D3 in the presence of parasitemia. Parasitemia on D2 higher than D0 count irrespective of axillary temperature. Parasitemia on D3 with axillary temperature ³5oC.
Late Treatment Failure (LTF): Development of danger signs of severe malaria after D3 in the presence of parasitemia, without previously meeting any of the criteria of early treatment failure. Presence of parasitemia and axillary temperature ³5oC on any day from D4 to D14, without previously meeting any of the criteria of early treatment failure.
Late Parasitological Failure (LPF): Presence of parasitemia on D28 and axillary temperature <5oC without previously meeting any of the criteria of early treatment failure or late treatment failure.
Adequate Clinical and Parasitological Response (ACPR): Absence of parasitemia on D14 irrespective of axillary temperature without previously meeting any of the criteria of early treatment failure or late treatment failure
Fever Clearance Time (FCT): The time taken from anti-malarial drug administration until axillary temperature falls below 37.4oC and remains at that value for 72 hours.
Parasite Clearance Time (PCT)
The time taken from anti-malarial drug administration until no patent parasitemia is detected.
Clinical Clearance Rate (CCR)
The proportion of subjects with full resolution of signs and symptoms of malaria on D14.
Recrudescence Rate (RR)
The proportion of subjects in which there is incomplete clearance of parasitemia on D14 and D28 of follow-up.
Statistical Analysis: Graphpad Prism version 4.0 (GraphPad Software, Inc., La Jolla, CA, USA) statistical software was employed and data presented in the form of tables and graph. Test of significance statistically determined using two-tailed Student t-test, at 95% confidence interval, p<0.05 considered significant.
Results
The baseline characteristics of test and control groups at presentation are as shown in Table 1.
Table 1: Baseline Characteristics of Test and Control Groups
| Characteristics | Test | Control | p-Value |
| Number of Patients | 30 | 30 | – |
| Male: Female Ratio | 2:3 | 2:3 | – |
| Mean Age (Range: 16-65 years) | 38.7±2.6 | 39.4±3.2 | p>0.05 |
| Mean Weight (Range: 43–92 kg) | 62.5±4.8 | 61.8±3.6 | p>0.05 |
| Mean Temperature (Range: 37.8–39.2oC) | 38.8±1.4 | 37.9±1.1 | p>0.05 |
| Mean Parasite Density (Range: 1260-21500/µL) | 9168±932 | 10723±821 | p>0.05 |
| Mean Hemogram (Range: 4.2 – 11.5g/dL) | 9.1±1.2 | 8.8±1.4 | p>0.05 |
| Mean WBC Total (Range: 3000 – 11700 x 109/L) | 6720±457 | 7700±453 | p>0.05 |
| Mean Alanine Transaminase
(Range: 7.8-31.2U/L) |
13.4±3.1 | 15.7 ±4.1 | p>0.05 |
| Mean Aspartate Transaminase
(Range: 13.7-28.4U/L) |
16.7±5.1 | 17.3±5.4 | p>0.05 |
| Mean Alkaline Phosphatase (Range: 45.2-110.7U/L) | 88.7±8.4 | 92.4±8.1 | p>0.05 |
| Mean Total Bilirubin (Range 4.3-13.8µmol/L) | 6.4±1.2 | 7.2±1.2 | p>0.05 |
The mean values of treatment failure in patients treated with amodiaquine and simvastatin (test) and those treated with amodiaquine alone (control) are shown in Table 2. The mean values of Parasite Clearance Time (PCT), Fever Clearance Time (FCT), Clinical Clearance Rate (CCR), Recrudescence Rate (RR) and Cure Rate (CR) in both test and control groups are depicted in Table 3.. Figure 1 depicted the mean geometric parasite densities of test and control groups on follow-up days D0, D3, D7, D14 and D28.
Discussion
A study reported initial mean geometric parasite density of 13167/µL in patients treated with amodiaquine alone12. However, in the said study initial parasite density was not normally distributed, and there was no statistically significant difference between the sensitive and resistant subjects based on the initial mean geometric parasite density. The study confirmed that 64% of patients treated with amodiaquine showed an initial parasite density under 10000/µL. A statistically significant difference (p<0.05) was found in the post-treatment mean geometric parasite density between the test and control groups as shown in Figure 1.
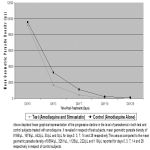 |
Figure 1 |
Mean values of treatment failure as reported in both test and control are as as shown in Table 2. Previous studies have reported in vitro therapeutic failure to amodiaquine13.
The total treatment failure of 32.8% reported in the control subjects was above the 25% recommended limit. This contrasts sharply with the value of 9.7% reported in the test subjects which was considered far below the 25% limit recommended for centres in the high endemicity of malaria transmission. The early treatment failure rate of 2.5% in the test group was considered far below the 10% margin as compared to 12.5% in the control which was above the 10% margin recommended for change in first line anti-malarial treatment. The above findings indicate that there was significantly less therapeutic failure in the test relative to the control group. This was further corroborated by a relatively better clinical response in the test compared to control as shown by mean values of adequate clinical and parasitological response (ACPR) depicted in Table 2.
Table 2: Mean Treatment Failure in the Test and Control Groups
| Treatment Parameters
|
Test | Control | P-Value |
| ETF (%) | 2.5±0.11 | 12.5±0.11 | P<0.05 |
| LTF (%) | 7.2±0.34 | 20.3±0.17 | P<0.05 |
| ACPR (%) | 90.3±0.55 | 67.2±0.45 | P<0.05 |
ETF: Early Treatment failure
LTF: Late Treatment failure
ACPR: Adequate Clinical and Parasitological Response
Amodiaquine, a 4-aminoquinoline is rapidly metabolized by the hepatic cytochrome CYP2C8 to N-desethylamodiaquine14, which exerts the main anti-malarial therapeutic effect15-16. The methodology to assess therapeutic efficacy of most anti-malarials has been standardized. This is in contrast to the wide variations in methodology used for in vitro testing, particularly for amodiaquine. A study highlighted the need to clinically differentiate between re-infections and recrudescence after 14 days. Hence, treatment failure is confirmed by msp-2-genotyping of infections at enrolment and recurrence of parasitemia17. The above procedure is not employed in the present study, notwithstanding that the study site is an area of intense malaria transmission.
The mean fever clearance time (FCT) reported for both test and control groups are as shown in Table 3. A study in Enugu, Nigeria reported fever clearance time of 41.2 hours in subjects treated with amodiaquine alone18. The present study revealed that mean fever clearance time in the test group treated with amodiaquine and simvastatin differed significantly (p<0.05) from the control treated with amodiaquine alone. The mean parasite clearance time (PCT) reported in the present study in respect of test and control groups are as presented in Table 3. A study in Enugu, Nigeria reported parasite clearance time of 6.1 days in respect of subjects treated with amodiaquine alone. This compares closely with the value obtained in the control in respect of the present study; though, the mean difference is not statistically significant (P>0.05). However, the parasite clearance time in respect of the control subjects treated with amodiaquine alone in the present study and that reported in the earlier study both differed significantly (p<0.05) from the test group treated with amodiaquine and simvastatin. Another study reported that parasite clearance time is lower during re-treatment with amodiaquine plus chlorpheniramine than during initial treatment with amodiaquine alone, although group mean difference is not significant19. The above study evaluated the use of chlorpheniramine, a histamine (H1) receptor antagonist in the enhancement of anti-malarial efficacy of amodiaquine; in amodiaquine resistant parasites harboring mutant PfcrtT76 and Pfmdr1Y86 alleles in which the treatment outcome is favourable. Nevertheless, the precise mechanisms of the enhancement of amodiaquine efficacy by chlorpheniramine or the clearance of drug resistant parasites remain unclear and the findings interpreted with caution because of the small number of subjects involved. The present study, however, evaluated the enhancement of amodiaquine efficacy by simvastatin, a HMG-CoA reductase inhibitor.
Table 3: Mean Clinical Response in the Test and Control Groups
| Clinical Parameters
|
Test | Control
|
p-Value
|
| PCT (Days) | 2.8±0.19 | 6.3±0.27 | P<0.05 |
| FCT (hours) | 24.3±1.13 | 66±2.1 | P<0.05 |
| CCR (%) | 96.3±0.5 | 71.6±2.1 | P<0.05 |
| RR (%) | 5.4±0.09 | 13.6±0.16 | P<0.05 |
PCT: Parasite Clearance Time
FCT: Fever Clearance Time
CCR: Clinical Clearance Time
RR: Recrudescence Rate
The present study reports recrudescence rates of 5.4% in the test compared to 13.6% in the control subjects treated with amodiaquine. These values are inversely related to the the clinical clearance rates of 96.3% and 71.6% in respect of test and control subjects respectively. Amodiaquine recrudescence results due to failure to eradicate the infecting population before drug concentration declines below the level of a minimum inhibitory concentration, necessary to maintain a parasite multiplication rate less than 1. There are generally, between 108 and 1013 parasites in the body in symptomatic malaria. The parasite population might be exposed to very high concentration of anti-malarial drug and up to 99.99% of the population killed during the first asexual cycle; although large numbers of viable malaria parasites still remain and must be killed in subsequent cycles. The short acting anti-malarial drugs such as amodiaquine which cause <1000-fold reductions in parasite number per cycle must be given for longer than four asexual cycles, that is 7 days, as the total parasite biomass in an adult with malaria may exceed 1012 parasites. The above may explain the relatively high recrudescence and lower cure rate reported in the control treated with amodiaquine alone in the present study compared to the test subjects treated with amodiaquine and simvastatin. This simple numbers game explains most of the in vivo and in vitro result following anti-malarial treatment20.
Studies have shown that malaria parasites are unable to synthesize fatty acid and cholesterol de novo for biogenesis of cell membranes, rather depending on their import from host plasma21-23. A new pathway to malaria infection has been uncovered linking it with cholesterol involved in the assembly of CD81 “cluster of differentiation 81” tetraspamin micro-domains on the cell surface necessary for sporozoite infection24. Malaria parasites are known to hide themselves in the dead liver cells to enable them travel from liver to blood stream without being noticed or detected by the immune system. The sporozoite traverse kupffer cell, then through a number of hepatocytes before finally taking up residence in the liver. Traversal damage and subsequent necrotic hepatocyte death have been confirmed in liver sections, revealing clusters of necrotic hepatocytes adjacent to structurally intact , sporozoite-infected hepatocytes25. Sporozoite traversal through hepatocytes, induces secretion of the host hepatocyte growth factor (HGF) which is known to render hepatocytes susceptible to infection26 . The successful liver stage replication is enhanced by hepatocyte growth factor/tyrosine kinase receptor signalling, which in addition to preventing the apoptosis of parasite-infected cells, induces actin re-organisation reported to be necessary for early liver stage development. Simvastatin, is known to concentrate in the liver, blocking the transformation of sporozoites to hepatocytic schizonts. Evidently, the enhanced clinical and parasitological responses already highlighted, as obtained in the test subjects relative to control in present study, can only be attributed to the modulating influence of the HMG-CoA reductase inhibitor, simvastatin.
Acknowledgments
I wish to acknowledge the sacrificial and tremendous assistance of the former executive secretary, Mr. M.O. Offu and entire staff of the 8 primary health facilities in the study site at Asu-Nkanu Local Health Authority, Enugu State, Nigeria. The selfless contribution of Mr. E.A. Ahaotu and Mr. B.C. Ezeagwoma, both of whom are chief medical laboratory scientists at University of Nigeria Teaching Hospital, is highly appreciated. My immense gratitude also goes toDr. Nick C. Obitte, Lecturer, Department of Pharmaceutical Technology, University of Nigeria, Nsukka for his assistance and useful advice. I sincerely acknowledge the contribution of Dr. G.P.I. Oluka, formerly Health Administrator, Enugu State Health Board and Pharm. P.O. Otegbulu, Director Pharmaceutical Services, Enugu State Ministry of Health.
Declarations
Authors’ contributions: The conception and design of this study was carried out by both NNN and POO. Data acquisition and conduct of the study was by NNN. Analysis and interpretation of data were carried out by both NNN and POO. The manuscript was drafted by NNN and meticulously reviewed by POO for intellectual content. NNN and POO read, scrutinized and approved the final draft of the manuscript prior to submission.
Conflict of Interest
None disclosed.
Funding
None
Ethical Clearance
Obtained from University of Nigeria Teaching Hospital, Health Research Ethics Committee (Ref: NHREC/05/01/2008B)
References
- Sowunmi A, AjedeAI, Falade AG, Ndikum VN, Sowunmi CO, Adedeji AA, Falade CO, Happi TO, Oduola AM. Randomized comparison of chloroquine and amodiaquine in acute uncomplicated malaria. Ann Trop Med Parasitol 2001; 96: 409-418.
- Grauper J, Gobels K, Groubusch MP, Lund A, Richter J, Haussinger D. Efficacy of amodiaquine in uncomplicated malaria. Ann Trop Med Parasitol 2001; 96: 409-418.
- Wang I, Oliaro P, Barenness H, Bonnet M, Brasseur P, Bukirwa H, Cohuet S, D’Alessandro U, Djimde A, Karema C, Guthmann JP, Hamour S, Ndiaye JL, Martensson A, Rwagacondo C, Sagara J, Same-Ekobo A, Sirima SB, van den Broek I, Yeka A, Taylor WR, Dorsey G, Randrianoriveloyosia M. Efficacy of artesunate-amodiaquine for treating uncomplicated falciparum malaria in sub-Saharan Africa: a multicentre analysis. Malar J 2009; 8: 203.
- Sinclair D, Zani B, Donegam S, Oliaro P, Garner P. Artemisinin-based combination therapy for treating uncomplicated malaria. Cochrane Database Syst Rev 2009; 8: CD007483.
- Falade CO, Michael SO, OduolaAMJ. Chlorpheniramine combination over amodiaquine alone in the treatment of acute uncomplicated Plasmodium falciparum malaria in children. Med Princ Pract 2008; 17: 197-201.
- Boutlis CS, Gowda DC, Naik RS, Maguire GP, Mgone CS, Bockerie MJ, Ibam ML, Lorry EK, Anstey NM. Antibodies to Plasmodium falciparum glycosylphosphatidylinositols: inverse association with tolerance of parasitemia in Papua New Guinean chilren and adults. Infect Immun 2002; 70: 5052-5057.
- Boutlis CS, Fagan PK, Gowda DC, Legog M, Mgone CS, Bockerie MJ, Anstey N.M. Immunoglobulin G (lgG) responses to Plasmodium falciparum glycosylphosphatidylinositols are short-lived and predominantly of the IgG-3 subclass. J Infect Dis 2003; 187: 862-865.
- Krishnegowda G, Hajjar AM, Zhu J, Douglass EJ, Uematsu S, Akira S, Woods AS, Gowda DC. Induction of pro-inflammatory responses in macrophages by the glycosylphosphatidylinositols of Plasmodium falciparum: cell signalling receptors, glycosylphosphatidylinositol (GPI) structural requirement and regulation of GPI activity. J Biol Chem 2005; 280: 8606-8616.
- Nebl T, MJ DEV, Schofield L. Stimulation of innate immune responses by malarial glycosylphosphatidylinositol via pattern recognition receptors. Parasitol 2005; 130(suppl. 1): 545-562.
- Solheim S, Seljeflot I, Arnesen H, Eritsland J, Eikvar L. Reduced levels of TNF alpha in hypercholesterolemic individuals after treatment with pravastatin for 8 weeks. Atherosclerosis 2001; 157: 411-415.
- Ferro D, Violi F. Simvastatin inhibits the monocyte expression of pro-inflammatory cytokines in patients with hypercholesterolemia. J Am Coll Cardiol 2000; 36: 427-431.
- Blair ST, Lacharme LL, Carmona FJ. Resistance of Plasmodium falciparum to anti-malarial drugs in Zaragoza (Antioquia Colombia). Mem Inst Oswaldo Cruz 2002; 97(3): 401-406.
- Olliaro P, Missano P. Amodiaquine for treating malaria. Cochrane Database SystRev 2003: CD000016.
- Li XD, Bjorkman A, Anderson TB, Ridderstrom M, Masimirembra CM. Amodiaquine clearance and its metabolism to N-desethylamodiaquine is mediated by CYP2C8: a new high affinity and turnover enzyme-specific probe substrate. JPharmacol Exp Ther 2002; 300: 399-407.
- Churchill FC, Patchen LC, Campbell CC, Schwartz IK, Nguyen-Dinh P, Dickinson CM. Amodiaquine as a pro-drug: importance of metabolite(s) in the anti-malarial effect of amodiaquine in humans. Life Sci 1985; 36: 53-62.
- Basco IK, Le Bras J. In vitro activity of monodesethylamodiaquine and amopyraquine against African isolates and clones of Plasmodium falciparum. Am JTrop Med Hyg 1993; 48: 120-125.
- Happi CT, Gbotosho GO, Folarin OA, Bolaji OM, Sowunmi A, Kyle DE, Millons WK, Wirth DF, Oduola AMJ. Association between mutations in Plasmodium falciparum chloroquine resistance transporter and Plasmodium falciparum multidrug resistance 1 genes and in vivo amodiaquine resistance in Plasmodium falciparum malaria infected children in Nigeria. Am J Trop Med Hyg 2006; 75: 155-161.
- Nwobodo N, Okonkwo PO. Comparative study on the efficacy of sulfadoxine-pyrimethamine, amodiaquine and amodiaquine plus sulfadoxine-pyrimethamine combination in the treatment of acute uncomplicated malaria in Enugu State, Nigeria. Biomedical and Pharmacology Journal 2008; 1(2): 301-304.
- Sowunmi A, Gbotosho GO, Happi CT, Adedeji AA, Bolaji OM., Fehintola FA, Fateye BA, Oduola AMJ. Enhancement of the anti-malarial efficacy of amodiaquine by chlorpheniramine in vivo. Mem Inst Oswaldo Cruz 2007; 102(3): 417-419.
- Nakazawa S, Kambara H, Aikawa M. Plasmodium falciparum: recrudescence of parasites in culture. Experimental Parasitology 1995; 81: 536-563.
- Holz GG. Lipids and the malaria parasite. Bull WHO 1977; 55(2-3):237-248.
- Valentin A, Rigomier D, Precigout E, Carcy B, Gorenflot A, Schrevel J. Lipid trafficking between high density lipoprotein and Babesia divergens infected human erythrocytes. Biol Cell 1991; 73:63-70.
- Vial HJ, Philippot JR, Wallach DFH. A re-evaluation of the status of cholesterol in erythrocyte infected by Plasmodiumknowlesi and Plasmodium falciparum. Mol Biochem Parasitol 1984;13:53-65.
- Schrie O, Charrin S, Billard M, Franetich JF, Clark KL, Van Gemert GJ , Saierwein RW, Dauty F, Boucheux C, Mazier D, Rubinstein E. Cholesterol contributes to the organization of tetraspanin-enriched microdomains and to CD81-dependent infection by malaria sporozoites. J Cell Sci 2006; 119: 1992-2002.
- Frevert U, Engelmann S, Zougbade S, Stange J, Ng B, Maluschewski K, Liebes L, Yee H. Intravital observation of Plasmodium berghei sporozoite infection of the liver. PloS Biol 2005; 3: c 192.
- Carrolo M. , Giordano S., Cabrita-Santos L., Corso S., Vigario A.M., Silva S., Leiriao P., Carapan D., Armas-Portelas R., Comoglio P.M. Hepatocyte growth factor and its receptor are required for malaria infection. Nat Med 2003; 9: 1363-1369.








