Muthu mani, Vijay Ebenezer and R. Balakrishnan
Department of Oral and Maxillofacial Surgery, Sree Balaji Dental College and Hospital, Bharath University, Chennai - 600 100, India
DOI : https://dx.doi.org/10.13005/bpj/475
Download this article as:| Copy the following to cite this article: Mani M, Ebenezer V, Balakrishnan R. Impact of Hemostatic Agents in Oral Surgery. Biomed Pharmacol J 2014;7(1) |
| Copy the following to cite this URL: Mani M, Ebenezer V, Balakrishnan R. Impact of Hemostatic Agents in Oral Surgery. Biomed Pharmacol J 2014;7(1). Available from: http://biomedpharmajournal.org/?p=2916 |
Introduction
Adequate bleeding control is very important in the success of all surgical procedures. Hemostatic agents may be beneficial in procedures like exodontia, tissue biopsies, placement of endosseous implants, and periodontal surgery. A perfect hemostatic agents does not exist. An ideal hemostatic agent should be lightweight, easy to store, and able to be rapidly applied to a hemorrhaging wound. It should be conformable to the wound, allowing the hemostatic agent to reach areas of injury which are difficult to access with direct pressure. The dressing should cause minimal local tissue destruction, be easily removable from the wound, and not contain particles which can spread systemically and the dressing must not be washed away by rapid bleeding from high-flow blood vessels.
The best management of perioperative hemorrhage is prevention. This includes a thorough preoperative patient history, necessary medical consults, familiarity with managing patients with possible bleeding diathesis, meticulous intraoperative technique, and appropriate postoperative instructions, care, and follow-up. Poor patient compliance with medication or postoperative instructions also are factors to be considered. During oral surgical procedures, persistent minor oozing of blood is common, although occasionally a bleeding episode prevents the continuation of the procedure and requires immediate attention. The usual sources for this intraoperative complication are incision into an area of granulomatous tissue, vessels in the periosteum or mucosa, or encountering nutrient arteries in the alveolar bone. Identification of the source of the bleeding requires good illumination, adequate retraction, and thorough suctioning. Once identified, the bleeding site should be packed, clamped, cauterized, burnished, debrided, and/or sutured for control. Topical hemostatic agents should be available, and if necessary, applied. The dentist should be familiar with the range of methods, techniques, materials, and their application during different types of bleeding episodes. Having a broad knowledge of the management approaches will allow the clinician to know when to apply a particular approach.
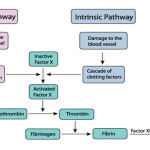
Clotting Mechanism
 |
Figure
|
Literature and Product Review
Hemostatic Collagen
These products (eg, CollaPlug, CollaTape, and Helistat) are soft, white, pliable, nonfriable, coherent, sponge-like structures. They are fabricated from bovine collagen (usually from deep flexor tendons) and are nontoxic and nonpyrogenic. The products are highly absorbent and able to hold many times their own weight of fluid. Their indications are for wound protection and for control of oozing or bleeding from clean oral wounds. It helps to control bleeding, stabilize blood clots, and protects the wound bed to facilitate the healing process. As for application, these products should be held in place for approximately 2 to 5 minutes to achieve hemostasis and then may be removed, replaced, or left in situ. All of these collagen materials are completely resorbed within 14 to 56 days1.
Hem Con
HemCon dressing (Hemorrhage Control Technologies, Portland, OR), is composed of chitosan, a substance derived from arthropod skeletons. Chitosan dressings are thought to function by mechanically sealing the wound and adhering to surrounding tissue. HemCon is a dual-sided 4 x 4 inch rectangular bandage: a chitosan-containing active side which must be placed directly on the wound and a nonstick side which the provider uses to apply pressure. The efficacy of HemCon depends entirely on the bandage adhering well to the wound, which is difficult in wounds which aren’t flat and easily accessible. The bandage isn’t flexible and can break when forced into a wound. It is best applied to flat, superficial wounds which are easily accessible. HemCon has been studied in both the military and civilian settings. The military demonstrated a 97% success rate in controlling bleeding with HemCon(9,10). The civilian experience has been less optimistic, controlling bleeding in 27 of 34 cases studied (79%). Of the seven failures, six were felt to be due to user error, possibly due to less training by civilian EMS providers in the proper use of the product (11). An additional study using a complex groin injury model in swine noted an increase in the rate of rebleeding and mortality between those treated with HemCon versus QuikClot. The authors noted that application of HemCon was more difficult than other agents and all failures of HemCon were due to the bandage not adhering to the injured tissue to which it was applied(12).
Gelatin
Gelatin-based hemostatic agents are abundant in modern operating rooms, and were first introduced in the 1940s as Gelfoam. Gelfoam is one of the more commonly employed agents for the control of minor bleeding. It is a porous, pliable sponge made from dried and sterilized porcine skin gelatin. Gelfoam’s mode of action is not completely understood, but unlike collagen, it is believed to be related to formation of a mechanical matrix that facilitates clotting(13,14,15,16) rather than affecting the blood-clotting mechanism. This agent can retain in its interstices 45 times its weight in blood (17). Gelfoam liquefies in one week and is completely resorbed in 4 to 6 weeks. Additionally, gelatin is hygroscopic, absorbing many times its weight in water. This action concentrates platelets and clotting factors and causes the gelatin to swell, which provides additional mechanical hemostatic action through compression (9,27,18). The addition of thrombin can enhance the hemostatic properties of gelatin sponge hemostatics, but plain Gelfoam or Surgifoam is affordable and readily accessible. A property of gelatin sponge hemostatics is the ability to absorb upwards of 40 times its weight in blood or fluids, and its capacity to expand up to 200% in vivo (19).
Another major advancement in the field of gelatin-based hemostatic agents came in the development of the product Floseal. Approved for commercial use in the US in 1999, Floseal combines human-derived thrombin with bovine-derived gelatin matrix granules which are mixed at the time of use (20) The major evolution of this product is the liquid nature of Floseal vs gelatin sponge, as well as a novel crosslinking of the gelatin matrix granules that minimizes in vivo expansion of the product [21]. With gelatin sponge agents, Floseal is absorbable and well-tolerated. Rare reports of abscess formation or granuloma formation have been reported with the use of gelatin-based agents.
Bone Wax
The British surgeon Sir Victor Horsley is often credited with the invention of the predecessor to modern bone wax with his publication of a formula for a soft, malleable, nonbrittle wax in 1886 from a mixture of beeswax, salicylic acid, and almond oil to achieve hemostasis in a canine model (9,22). Evidence shows that sealing wax was commonly used as early as 1850 for hemostasis in cranial bones(23). It is useful when bleeding is from a visualized local vascular channel within bone, commonly referred to as a “bone bleeder,” at the surgical site. This occurs commonly during the extraction of mandibular third molars, and if not adequately addressed during surgery can be a reason for postoperative bleeding.
Cellulose
Surgicel (Johnson & Johnson) is a resorbable oxidized cellulose material and is an expensive but useful option in oral surgery. It is prepared as a sterile fabric meshwork. Its mechanism of action is not completely understood, but appears to be physical rather than involve an alteration of the clotting mechanism. After it is fully absorbed with blood, it swells into a brownish/black gelatinous mass that aids in clotting. Excessive amounts of the material should be removed if possible to prevent delayed healing. Specific dental indications include use as an adjunct to control bleeding in exodontia and other oral surgical procedures (Somerville MJ 1998) This material may be more useful in soft-tissue procedures due to its shape, consistency, and interference with osteogenesis.
ActCel is a new topical hemostatic agent that is made from treated and sterilized cellulose and available in similar fabric meshwork as Surgicel, although it is slightly more friable. It is an FDA-approved material indicated for the control of bleeding from open wounds and body cavities (eg, mouth, ears, nose, throat, and vagina). The material does not contain chemical additives, thrombin, or collagen, and is hypoallergenic. In contact with blood, it expands to 3 to 4 times its original size and is almost immediately converted to a gel. Complete dissolution of the product takes place within 1 to 2 weeks (23). Because of its purity and the fact that it degrades rapidly into biocompatible end products (glucose, water), it does not adversely affect wound healing. ActCel’s mechanisms of action are multiple, enhancing the coagulation process biochemically by en-hancing platelet aggregation and physically by 3-D clot stabilization. Additionally, many of the previously mentioned enzyme-mediated reactions within the clotting cascade are calcium dependent. One study has demonstrated that ActCel adheres to calcium ions (23), making calcium more available for the clotting cascade. Further, since the material’s surface area increases as it dissolves, the area available for the coagulation process also increases.
Prevention of Dry Socket
Localized alveolar osteitis is the most common complication in extractions, with a prevalence of 1.9% to 31.2% following removal of mandibular third molar teeth (25, 26, 3). A variety of theories exist as to its etiology, although it certainly involves an interruption of the healing process. This condition is a significant problem for both the clinician and the patient, as 45% of patients who develop alveolar osteitis require at least 4 additional postoperative visits(8). Several methods have been found to reduce the incidence of alveolar osteitis, including the use of both topical (5, 6, 7) and systemic agents 2, 3, 4 ). Preliminary results examining the use of ActCel and tetracycline in mandibular impacted extraction sites have reduced alveolar osteitis (personal observation). Randomized controlled trials are needed to substantiate these observations. Indications for the use of ActCel are the control of bleeding or protection of a wound in the oral cavity. This includes minor oozing that may require additional hemostatic assistance, routine use in mandibular third molar extraction sites to decrease the occurrence of alveolar osteitis, or as an adjunct for control of arterial bleeding (first stopping the arterial bleed with other methods and then assisting in stabilizing the clot by placement of ActCel). ActCel, should not be placed in areas that are not in communication with the external environment or placed in infected sites.
Microfibrillar Collagen
Avitene, a topical microfibrillar collagen hemostatic, was introduced in the US in the early 1970s. Microfibrillar collagen products are made by purifying bovine collagen and processing it into microcrystals, which can then be manipulated into hemostatic agents in a wide variety of formats. The brand Avitene was first launched in a flour form, and it is still commonly used in the topical powder form. All manner of collagen-based hemostatics enjoyed widespread early use as they were felt to be more effective than gelatin-based hemostats. Collagen-based products activate the intrinsic pathway of the coagulation cascade, whereas gelatin hemostats are thought to induce hemostasis through physical properties alone27.
Conclusion
Hemostatic agents are used in dentistry for hemorrhage control and wound protection. This article has reviewed different hemostatic agents, their mechanisms of action, and their clinical indications and contraindications.
Reference
- Ogle OE. Perioperative hemorrhage. In: Dym H, Ogle OE.Atlas of Minor Oral Surgery. Philadelphia, Pa: WB Saunders; 2000:62-63.
- Rood JP, Murgatroyd J. Metronidazole in the prevention of ‘dry socket’.Br J Oral Surg. 1979;17:62-70.
- Krekmanov L, Nordenram A. Postoperative complications after surgical removal of mandibular third molars: effects of penicillin V and chlorhexidine.Int J Oral Maxillofac Surg. 1986;15:25-29.
- Mitchell DA. A controlled clinical trial of prophylactic tinidazole for chemoprophylaxis in third molar surgery.Br Dent J. 1986;160:284-286.
- Quinley JF, Royer RQ, Gores RJ. “Dry socket” after mandibular odontectomy and use of soluble tetracycline hydrochloride.Oral Surg Oral Med Oral Pathol. 1960;13:38-42.
- Goldman DR, Kilgore DS, Panzer JD, et al. Prevention of dry socket by local application of lincomycin in Gelfoam.Oral Surg Oral Med Oral Pathol. 1973;35:472-474.
- Julius LL, Hungerford RW, Nelson WJ, et al. Prevention of dry socket with local application of Terra-Cortril in gelfoam.J Oral Maxillofac Surg. 1982;40:285-286.
- Osborn TP, Frederickson G Jr, Small IA, et al. A prospective study of complications related to mandibular third molar surgery.J Oral Maxillofac Surg. 1985;43:767-769.
- Achneck HE, Sileshi B, Jamiolkowski RM, et al. A comprehensive review of topical hemostatic agents: Efficacy and recommendations for use. Annals of Surgery 2010; 251: 217-228.
- Mabry R and McManus JG. Prehospital advances in the management of severe penetrating trauma. Crit Care Med. 2008:36(7);S258-266.
- . Brown MA, Daya MR, Worley JA. Experience with chitosan dressings in a civilian EMS system. J Emerg Med. 2009;62:239-243.
- Kozen BG, Kircher SJ, Henao J, et al. An alternative hemostatic dressing: comparison of CELOX, HemCon, and QuikClot.Acad Emerg Med. 2008; 15:74-81.
- Guralnick W, Berg L. GELFOAM in oral surgery.Oral Surg. 1948;1:629-632.
- Jenkins HP, Janda R, Clarke J. Clinical and experimental observations on the use of gelatin sponge or foam.Surgery. 1946;20:124-132.
- Jenkins HP, Janda R. Studies on the use of gelatin sponge or foam as a hemostatic agent in experimental liver resections and injuries to large veins.Ann Surg. 1946;124:952-961.
- Correll JT, Prentice HR, Wise EC. Biologic investigations of a new absorbable sponge.Surg Gynecol Obstet. 1945;181:585-589.
- Council on Pharmacy and Chemistry. Absorbable gelatin sponge: new and nonofficial remedies.JAMA. 1947;135:921.
- Palm MD, Altman JS. Topical hemostatic agents: a review.Dermatol Surg. Apr 2008;34(4):431-45.[Medline].
- Pfizer GELFOAM package insert. Available from: http://media.pfizer.com/files/products/uspi_gelfoam_sponge.pdf[last cited on 2009]
- Baxter FLOSEAL [Hemostatic matrix] instructions for use. 2005
- Renkens KL, Jr, Payner TD, Leipzig TJ, Feuer H, Morone MA, Koers JM, et al. multicenter, prospective, randomized trial evaluating a new hemostatic agent for spinal surgery. Spine (Phila Pa 1976) 2001;26:1645–50. [PubMed]
- Tan TC, Black PM. Sir Victor Horsley (1857–1916): pioneer of neurological surgery.Neurosurgery. 2002;50:607–611; discussion 611–612.
- Gupta G, Prestigiacomo CJ. From sealing wax to bone wax: predecessors to Horsley’s development. Neurosurg Focus. 2007;23(1):E16.
- Zhang Qin-shang, Xu Qing-zhong. Application of S-99 soluble styptic gauze to wounds. Beijing Xuan Wu Hospital, Departments of Pathology and Stomatology. Beijing, China. December 31, 1982: personal communication.
- Barnes AC. The use of gelatin foam sponges in obstetrics and gynecology. Am J Obstet Gynecol. 1963;86:105-107.
- Swanson AE. Prevention of dry socket: an overview. Oral Surg Oral Med Oral Pathol. 1990;70:131-136.
- Sirlak M, Eryilmaz S, Yazicioglu L, Kiziltepe U, Eyileten Z, Durdu MS, Tasoz R, Eren NT, Aral A, Kaya B, Akalin H. Comparative study of microfibrillar collagen hemostat (Colgel) and oxidized cellulose (Surgicel) in high transfusion-risk cardiac surgery. J Thorac Cardiovasc Surg. 126(3):666-70, 2003 Sep.








