K. V. R. N. S. Ramesh¹ and K. Ravi Shankar²
¹Aditya Institute of Pharmaceutical Sciences, Surampalem India.
²Sri Sai Aditya Institute of Pharmaceutical Sciences, Surampalem India.
Keywords
Oncolytic viruses; Cancer
Download this article as:| Copy the following to cite this article: Ramesh K. V. N. S. Shankar K. R. Oncolytic Viruses for the Treatment of Cancer (A review). Biomed Pharmacol J 2009;2(2). |
| Copy the following to cite this URL: Ramesh K. V. N. S. Shankar K. R. Oncolytic Viruses for the Treatment of Cancer (A review). Biomed Pharmacol J 2009;2(2).Available from: http://biomedpharmajournal.org/?p=746 |
Introduction
The limited efficacy and toxicity of current cancer therapies have been the impetus for the search for novel approaches to the treatment of cancer [1]. The goal in developing new therapies for the treatment of cancer is to design agents that have large index (high potency against malignant cells) but limited pathogenicity to normal tissue cells [2].
One such approach is gene therapy, which seeks treat cancer by the introduction of genes that will result in destruction of the tumor from within or will enhance an immune response against it. Viruses are frequently chosen as vehicles for such genes because they have evolved a very efficient mechanism of gene transfer (transduction) and expression. As many viruses lyse cells, the cells in which they replicate, the suggestion that viruses might potentially be used to destroy specific cell populations is not altogether surprising. It does however seem a little ironic that viruses which are otherwise one of the causes of cancer might be used to combat cancer [1].
During the last century, many attempts are made to explore the cytolytic effects of several wild type viruses as oncolytic agents. Until recently attenuated and replication defective viruses are used as vectors for cancer gene therapy for safety purposes [3]. The use of replication defective viruses is particularly important where diseases other than cancer are being treated in which the survival of the transduced cell is a necessity. If however one is attempting to transducer tumor cells and destroy them then one may take advantage of any cytotoxic effects a virus may exhibit.
Naturally occurring lytic viruses have evolved to infect, replicate and lyse human cells. It is evident that the replication cycle of many viruses exploits the same cellular pathways that are altered in cancer cells [[2]. In general there are two aspects of oncolytic viral therapy-direct and indirect. First some cytopathic viruses preferentially replicate in proliferating cells. These are investigated as specific oncolyitc viruses (OVs) that reduce the tumor cell load in conjunction with conventional therapies. The second, viruses act as foreign antigens and may aid in the recognition of cancer cells by the host’s humoral and cellular immune systems. This could potentially enhance virus induced tumor regression [4].
Recent advances in the understanding of the molecular biology of cancer as well as the availability of technologies to genetically engineer viruses have led to the concept of oncolytic viruses. These biological agents are thought to hold the toxic and discriminating power that is expected from an efficacious therapy against human cancer and they have several appealing approaches. Whereas conventional chemotherapeutic agents distribute relatively uniformly throughout the human body and follow the typical log kinetics of cell killing, the local replication of administered oncolytic viruses amplifies the input dose and creates a high concentration of the agent at the target site. The accumulation helps to spread the agent to adjacent tumor cells and limits the potentially toxic side effects within the normal tissue cells [2].
An Overview of Cancer
Cancer is a group of over 100 different diseases characterized by uncontrolled cellular growth, local tissue invasion and distant metastasis. [5]. Cancer also is a genetic disease in that it arises because of alteration in DNA that result in unrestrained cellular proliferation. Most of these alterations involve actual sequence changes in DNA. They may arise as a consequence of random replication errors, exposure to carcinogens or a faulty DNA repair process [6]. Chemical carcinogens such as those in tobacco smoke, azo dyes, aflotoxins and benzene are clearly implicated in cancer induction in humans and animals [7].
One abnormal cell that begins to replicate without the controls that normally keep growth in check will grow into a mass of abnormal cells called a tumor or a neoplasm. Some of the tumors simply grow in place without causing any damage except for devouring more than their share of nutrients and perhaps creating a mechanical blockage in the body as they enlarge. Such tumors are benign. More serious tumors are those whose cells are able to invade other tissues – these are cancers or malignant tumors [8]. Cells that leave the tumor and spread throughout the body forming new tumors at distant sites are called metastases.
Cancer have 3 major characteristics: hyperplasia, anaplasia and metstasis. Hyperplasia is the uncontrolled proliferation of cells. Anaplasia is structural abnormality of cells (these cells also have a loss of or reduction in their function). Metastasis is the ability of a malignant cell to detach itself from a tumor and establish a new tumor at another site within the host.
Viruses and Cancer
Viruses indicated in human cancer are called oncogenic viruses. Persistent viral infection is suspected to be the root cause of as many as 20% of hum an malignancies. For the most part, cancer is an accidental and highly unusual or long term effect of infection with oncogenic human viruses [6]. Viruses can be isolated tumors and these viruses cause virus-containing tumors to develop in other individuals [9].
There are 2 classes of tumor viruses – DNA tumor virus and RNA tumor virus the latter also being referred to as Retrovirus. These 2 viruses have the ability to integrate their genome with that of the host cell genome. A number of viruses have the potential to change a cell from a normal cell to a cancer cell. This process called transformation, can be induced by infections of animal ell with certain kinds of viruses [10]. The DNA viruses are incorporated into the genes of the host and are then transmitted to subsequent generations. The genes are then expressed without the usual symptoms that accompany infection [11]. The transformation often results in loss of growth control. The region of viral genome that causes tumor is called oncogene. This foreign gene can be incorporated into a host cell and causes it to gain new properties such as immortalization anchorage independent growth. The oncogenes may not be unique to the viruses and homologous genes are found in normal host tissue cells as well. Indeed it is likely that a virus picked up a cellular gene during its evolution and this gene has subsequently got altered. Normally the cellular oncogenes are not expressed as or they are expressed in low levels. However they become aberrant when the tumor virus that does not in itself carry the oncogene infects the cell.
DNA tumor viruses are most commonly involved in human malignancy. Etiological studies have clearly established human papilloma virus (HPV) infection as the central cause of invasive cervical caner [12]. Approximately 40 different types of HPV types are known to infect the genital tract and epidemiological studies to date suggest that at least 14 of these are high risk type. Other DNA viruses of tumor causing potential include Human Polyoma viruses, Adeno viruses, and Herpes viruses. RNA viruses that cause tumor include – HTLV – 1 and HTLV – 2, Lentiviruses and Spuma viruses.
Overview of Oncolytic Viruses
Oncolytic (“onco” meaning cancer, “lytic” meaning “killing”) viruses represent an innovative potential cancer therapy known as “virotherapy” – a therapy that seeks to harness the natural properties of viruses to aid in the fight against cancer.
In short, oncolytic viruses are human viruses that infect and replicate in cancer cells, destroying these harmful cells and leaving normal cells largely unaffected. Like all viruses, oncolytic viruses seek to penetrate a host cell and “trick it into replicating more of the virus until ultimately, it bursts. However, unlike other viruses, oncolytic viruses seek only to replicate in cancer cells. In general oncolytic viruses derive their specificity by exploiting cell surface or intracellular aberrations in gene expression that arise during tumor evolution [13]. The treatment of human tumors with a replication selective virus is a natural extension of virus mediated gene delivery that in theory offers several advantages. The oncolytic virus itself is capable of lysing the infected tumor cell to eradicate or reduce the tumor mass. Importantly, replication leads to amplification of the input dose of the virus and these progeny viruses are released by virus-mediated lysis of the infected cell to spread and infect surrounding cells. This self-perpetuating treatment continues until the host immune response and / or susceptible cell become limiting.
The concept of using replicating viruses as anticancer agents is not new. For nearly a century the idea of using replication competent viruses to treat human cancer has been revisited with various viruses. Observations made in the early 1920s indicated that viruses replicated in and lysed murine and other experimental tumors. In 1940s and 1950s, studies were conducted to evaluate the usefulness of the viruses in the treatment of tumors.
Mechanism of antitumor efficacy of oncolytic viruses
Oncolytic viruses mediate the destruction of tumor cells by several potential mechanisms (Table-1). These include – cell lysis, cell apoptosis, antiangiogenesis and cell necrosis. In cell lysis once the virus infects the tumor cell, it compromises the cell’s natural defense mechanisms giving the virus the extra time to thrive. The virus then begins to replicate and continues until finally the tumor cell can no longer accommodate the increasing number of viruses and bursts. The liberated viruses then spread to the neighbouring cancer cells to continue the cycle. It is important to remember that all oncolytic viruses are intended to replicate only in cancer cells (strategies to generate tumor selectivity are reviewed latter) and to bypass through the normal tissue without causing harm. Hence once all the tumor cells are eradicated, the oncolytic viruses no longer has the ability to replicate and the immune system clears it from the body [15].
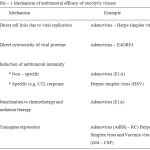 |
Table 1: Mechanism of antitumoral efficacy of oncolytic viruses.
|
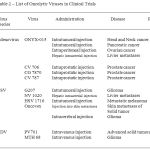 |
Table 2: List of Oncolytic Viruses in Clinical Trials.
|
Another mechanism by which the oncolytic viruses act is to generate proteins during their replicative cycle that are directly cytotoxic to the tumor cells. Adenoviruses for example express the E311.6Kd death protein and the E4ORF4 protein late in the lytic cycle and both of these proteins are cytotoxic to cells [16]. Many of the adenoviral vectors used for oncolytic therapy have deletions in viral genes that have impaired the cytolytic activity. It was demonstrated by Bell, J.V. et al [13] that by reinserting the viral ADP (adeno virus death protein) gene the virus become more cytolytic and has an increased ability to spread between cells.
A different mechanism by which oncolytic viruses mediate tumor cell destruction is via induction of non-specific antitumor immunity. Tumor cell are inherently weakly immunogenic, in part because they exhibit decreased expression of the major histocompatibility complex (MHC) antigens and stimulatory signals including cytokines that activate local immune responses. But infection of the tumor cells by the replicating adenoviruses with expression of the E1A protein leads to increased sensitivity to tumor necrosis factor (TNF) mediated killing [16].
More importantly, induction of specific antitumor immunity confers the possibility of long-term protection against tumor recurrence. After viral infection of a tumor cell, there is infiltration of lymphocytes and antigen presenting cells as well as induction of cytokine release. Viral antigens are presented on the cell surface in conjunction with MHC class I protein, a complex that is then recognized by cytotoxic T lymphocytes (CTLs) that are attracted the virally transduced tumor. By an unknown mechanism as yet identified these CTLs acquire specificity for tumor specific antigens in the process of viral antigen recognition and cell killing. A system specific antitumor immune response is thereby established as demonstrated with herpes simplex virus type I (HSV – I) mutant [16].
Oncolytic viruses not only kill cells but also carry genes that make the cells more susceptible to radiation or chemotherapy, thereby delivering a double blow to the tumor [17]. For example, the adenovirus E1A gene product is potent chemosensitizer particularly in cells with functional p53. The E1A gene product can induce high levels of p53 in these cells and render them susceptible to DNA damage from chemotherapy and radiation. Normal, non-transformed cells appear to be unaffected by E1A. Interestingly the adenovirus E1A gene product can sensitize tumor cells to chemotherapeutic agents even in the absence of functional 53 by an unknown mechanism.
Another mechanism by which the oncolytic viruses mediate antineoplastic activity is by the expression of therapeutic transgenes inserted into the viral genome. These armed therapeutic viruses offer a distinct advantage over the replication incompetent viruses that have been employed in the vast majority of gene therapy applications to date. As the virus amplifies itself through several rounds of replication of neighboring cells, there is a concomitant amplification in transgene expression, which produces amplified antitumor effect [16].
Possible Benefits of Oncolytic Virus Therapy
Clinical data suggest that oncolytic viruses may offer therapeutic advantages over existing cancer therapies such as chemotherapy and radiation and may even act synergistically with these conventional approaches [18]. The primary benefits identified to date include the following:
High therapeutic index: Compared with traditional therapies, oncolytic viruses thave been shown to have a high therapeutic index. In some instances, the therapeutic index of oncolytic viruses is found to be as high as 100,000 to one. In other words, for every 100,000-tumor cells that are killed only one normal cell is killed. This is significantly higher than the Ti of commonly used chemotherapeutic agents and will result in greater efficacy with fewer side effects. Chemotherapy and radiation are the mainstay in the treatment of advanced cancers but are limited by tumor cell resistance to these agents and a relatively narrow TI. Thus dose escalation or combination of therapies designed to overcome resistance or increase tumor cell kill are limited by toxicity to normal tissues. Oncolytic viral therapy, on the other hand is capable of increasing the TI between tumor cells and normal cells when viral replication proceeds preferentially in tumor cells.
Better antitumor efficacy due to viral replication: Unlike some traditional therapies that are cleared form the body within a specific amount of time (e.g. chemotherapy), oncolytic viruses are engineered to proliferate and remain in the body until all of the cancer cells are destroyed. This self-proliferation could potentially mitigate the need for extensive re-treatment and result in greater efficacy and patient convenience.
Synergistic antitumor activity with other cancer therapies: some oncolytic viruses have been shown to have significant synergy with conventional cancer treatments such as radiation and chemotherapy. This type of combination therapy could potentially lead to greater therapeutic efficacy.
Virus mediated oncolysis may also enhance antitumor immune response: These immune responses may include reactions not only to the viral component but also to specific tumor antigens that are released following oncolysis. Several observations [19], suggest that these additional immune enhancements may enable eradication of metastases following local tumor treatment. Additional effects on the immune response also can be achieved by engineering the viral vector to direct expression of viral cytokines.
Oncolytic viruses are multimodality therapeutics that can be engineered to have the tumor specificity. In particular viral genomes are highly versatile and can be modified to direct their cytotoxicity toward cancer cells. Perhaps the greatest advantage that the oncolytic virus platform offers over chemical agents is its ability to be tailored by in vitro genetic manipulation in response to preclinical findings.
Strategies to Develop Tumor Selective Viruses
Research is currently being carried out by many institutions around the world using both non – engineered viruses to evaluate their use in the fight against multiple types of cancer. Thee are several strategies that achieve tumor selectivity of replication competent viruses some of which are mentioned here.
Naturally occurring Oncotropic Viruses
One approach to achieve viral tumor selectivity is to use viruses that possess inherent tumor selectivity. Over the last decade, a new understanding has emerged of the signaling pathways that mammalian cells use to resist virus infection. It is now apparent that pathways controlling the first line of cellular defense against viral invasions often control aspects of cell growth and apoptosis. It follows that during tumor cell evolution, aberrations in cell growth control and apoptosis occur concomitantly with defects in cellular antiviral response.
Several RNA virus species are tumor tropic which is party the result of their ability to grow exclusively in cells with defective antiviral system [ e.g. Newcastle Disease Virus (NDV) and Vesicular Stomatitis Virus (VSV) ]. Vesicular stomatitis virus is a RNA virus sensitive to the antiviral actions of alpha / beta interferon can be completely protected from infection by this virus but tumor cells lacking an interferon response are rapidly killed by VSV. It is found that VSV variants that robustly induce interferon production as a byproduct of infection are self-attenuating in normal tissues but grow unabated in tumor cells.
The precise mechanism of tumor selectivity with other viruses is poorly understood and is likely to differ with each virus. For example the autonomous parvoviruses are unable to force resting cells into S phase and are therefore incapable of undergoing genome replication in quiescent cells [21]. Therefore the efficiency with which parvoviruses replicate in transformed cell lines relative to normal cells is probably due to the aberrant cell cycle control exhibited by transformed cells. Some naturally occurring viruses of veterinary importance have been adapted by serial passage in tumor ells to increase their oncolytic efficacy [22]. NDV strains adapted to Ehrlich ascites carcinoma cells or human melanoma cells are two examples. NDV was first reported [23] as having oncolytic activity in the mid 1950s and lysates prepared from NDV infected tumor explants (known as viral oncolysates) have been administered to cancer patients since the mid 1960s in attempts to augment the antitumor immune response
As with any anti cancer therapy, the ctytotoxic effects of the oncolytic viral thrapy upon the normal tissue surrounding the tumor must be minimized. A number of viruses naturally replicate preferentially in transformed cells but it is unlikely that these viruses will demonstrate the degree of tumor selectivity required by the regulatory authorities for the routine treatment of cancer patients. Since naturally occurring viruses are unlikely to be considered safe enough, the virus must be the one that is amenable to genetic manipulation. The virus should ideally be the one, which is well characterized in terms of its replication in different cell types and its pathogenesis. The virus must be able to replicate efficiently in the context of a developing or even a pre-existing antiviral immune response. This may require expression of viral proteins that are involved in suppression of the antiviral immune response. The virus must be able to disseminate throughout the tumor mass destroying cells directly or sensitizing them to the action of other therapeutic agents while sparing the surrounding normal tissue. Furthermore infection with the virus should stimulate an effective antitumor immune response that would lead to destruction of metastases. In this regard, active research is going on in developing tumor specific engineered viruses.
Engineered Viruses
The use recombinant (engineered) and replication – competent viruses for cancer therapy became possible with the identification of specific genes or gene regions that are necessary for replication or toxicity in normal cells but are expendable in tumor cells. For example transformed cells exhibit different patterns of gene expression and often display different proteins on their surfaces. Currently attempts are being made to exploit these differences with a view to generating tumor specific viruses. In general virus replication can be subdivided into the attachment of the virion, internalization, uncoating and transcription and finally to assembly and release. Each of these processes could represent opportunities for achieving tumor specificity. For example tumor specificity may be achieved by modifying viral attachment proteins such that the resulting viruses bind selectivity to a tumor specific cell surface molecule [24]. Furthermore tumor selectivity can be achieved by linking viral protein coding regions to the promoters or enhancers of cellular genes that are upregulated in or expressed solely in tumor cells [25].
Some of the developments that took place with regard to the engineered viruses will be briefly reviewed here. Tumor selective viruses can be engineered by altering viral surface proteins that recognize specific cellular receptors, allowing the virus to specifically enter cancer cells. Replicative selectivity can be engendered by modifying the viral genes that are required for efficient replication so that the virus can only replicate in cells that have disruptions in normal homeostatic pathways such as tumor suppressor defects or activation of oncogenic pathways.
Tumor selective infection
This approach is carried out mainly with adenovirus based oncolytic viruses. Structurally, the DNA of these viruses is enclosed by a protein capsid that is composed of several elements including a penton base and a fibre. The fibre binds to the coxsackie and adenovirus receptor (CAR)[26], a homophilic adhesion molecule that is expressed on various cells. Additional low affinity interactions exist between cellular integrins and the adenoviral penton base [27]. Because CAR expression is inversely correlated to malignancy and in some tumors there is minimal if any CAR expression – untargeted adenoviruses might infect normal cells more than neoplastic ones. The fibre can however be modified to overcome this obstacle. Bispecific antibodies have been developed to link the fibre to a cellular receptor that is highly expressed in malignant cells [such as the epidermanl growth factor receptor (EGFR). These antibodies have been shown to prevent the virus from infecting non-malignant CAR expressing cells.
Tumor selective replication
There are other strategies to develop oncolytic viruses that replicate only in tumor cells. Those viruses are designed to target cells that have alterations in signal transduction pathways that promote tumorigenesis.
The p53 tumor suppressor pathway
The tumor suppressor protein p53 induces cell growth arrest or apoptosis in response to DNA damage. The p53 induction of apoptosis is also a cellular stress response to viral infection that eliminates propagation of the virus to neighbouring tissues. The adenoviral protein E1B55Kd is thought to block p53 activity, which prevents apoptosis and allows adenoviral replication to occur. This mechanism has been exploited to impart tumor selectivity. A mutant strain of adenovirus that lacks E1B55Kd was initially shown by some laboratories to selectively replicate in and lyse cancer cells that carry TP53 (which encodes p53) mutations or have other defects in p53 function [28] such as CDKN2A (which encodes INK4A/.ARF) mutations. This virus known as ONZY – 015 is the subject of several reviews [29,30].
The RAS/PKR or IFN/PKR pathway
The double stranded RNA dependent protein kinase (PKR) and its associated signaling pathways regulate the tumor specific replicative ability of different oncolytic viruses. Viral infection of cells activates not only p53 response but also another stress response – PKR activity. PKR activity. PKR is a cytosolic enzyme that phosphorylates the translation factor eiF2 – inhibiting its function and shutting off protein synthesis in cells. Unusual nucleic acid structures such as dsRNA activate various cellular stress responses. Human PKR possesses a dsRNA – binding domain at its amino terminus. Although dsRNA binding to these domains is thought to activate PKR function induction of PKR activity might also occur through cytokine, interferon (IFN) and stress signaling pathways that are thought to operate independently of dsRNA. PKR mediated activation of a transcription factor called NF – B leads to the transcription of proinflammatory genes, enhancing the clearance of virally infected cell. Inhibition of PKR is therefore crucial to the successful progression of the viral life cycle.
What is the link between PKR, tumors and oncolytic viral replication? Although little, if any evidence links genetic mutations in PKR or its downstream targets to tumorigenesis, oncogenic pathways that regulate PKR activity have been described. For example, activated RAS mutants have been shown to inhibit PKR [31] although the identify of this inhibitor remains elusive. So viruses with mutations in the PKR inhibitory protein such as ICP34.5 in HSV 1, NS1 in influenza would be able to replicate in tumor cells with overactive RAS whereas in normal cells PKR activity would limit the replication of such mutant virus. In such instances even some wild type virus such as reovirus or Newcastle disease virus can selectively replicate in ells with overactive RAS.
Tumor Selective Promoters
A slightly different approach to achieving tumor selective replication involves linking genes to promoters that are only functional in tumor cells. This strategy has been used primarily with adenoviruses and HSV1. One tumor specific promoter is derived form the gene that encodes alpha – fetoprotein (AFP). AFP is expressed in several tissues during development in adult tissues its expression is limited to tumors of hepatic and intestinal origin. In an adenoviral vector, this promoter can be used to regulate the expression of both E1A and E1B55Kd. There is a 10,000-fold increase in the replication of this virus in AFP – expressing cells, compared with AFP sensitive tumors such as hepatocellular carcinomas with minimal toxicity to normal cells. Other tumor promoters include surfactant protein B gene promoter for lung cancer [33] and the MCU1 protein for breast carcinoma [34], the carcinoembryonic antigen promoter in colorectal and lung cancer cells and the tyrosinase gene promoter in melanomas.
Other Tumor Targeting Strategies
Several oncolytic viruses target tumor cells through different avenues. A vaccinia virus with a deletion in the vaccinia growth factor (vgf) displays oncolytic properties. Vaccinia oncolysis can be increased by also deleting the gene that encodes thymidine kinase. Vgf acts as mitogen that primes neighbouring ells for subsequent rounds of viral infection. Viruses with mutations in both genes have been shown to have oncolytic specificity [35].
Poliovirus is a neuropathogenic virus that infects and propagates in spinal cord motor neurons and causes paralytic effects in humans. The nueropathogenic function of the wild type virus resides with an internal ribosome entry site (IRES) element. When this element is included in viral vectors it confers neuron specific translation genes that are needed for viral propagation. When this IRES element is substituted with IRES from human rhinovirus type 2, the neuron specificity is lost and the virus cannot propagate in neuronal cells and infection of glial tumor cells in facilitated [36]. Measles virus is also shown to have oncolytic effects [37]. In fact in anecdotal reports [38], measles infection was found to be associated with regression of Burkitt’s lymphoma. However the oncolytic targeting mechanism for the virus remains undetermined. Oncolytic effects of mumps, Sendai, Semliki and Sindbis viruses are also reported but like is known about targeting mechanisms of these viruses or their oncolytic or cytotoxic properties [39].
Preclinical Trials with Oncolytic Viruses
The process of determining the anticancer effects and toxic side effects of the oncolytic viruses has relied on a variety of in vitro assays as well as on the use of animal models. Generally, the definition of oncolytic selectivity is that a virus infects, replicates in and lyses more tumor than normal cells. Defining the therapeutic index of a replicating virus can however be problematic. Oncolytic viral replication in tumor cells versus normal cells can show differences of upto 110,000 fold in viral titres [40]. In fact, gien enough time to allow for viral propagation, dose – effect curves can reveal cytopathic effects for some oncolytic viruses at a viral multiplicity of infection (MOI) of 0.01 – 0.001 in tumor cells, whereas a MOI of 100 – 1,000 is required for small effects to occur in normal cells. Multiplicity of infection is defined as the ratio of number of infections units of oncolytic virus to number of cells. These therapeutic indices compare favorably with those exhibited in vitro by anticancer drugs. In fact drug and oncolytic virus development requires the fulfillment of the same principles of specificity for tumor cells and lack of toxicity against normal cells, yet differences exist with respect to how this is achieved. The biological efficacy of oncolytic viruses is tested in several animal models of human cancer. These include immunocompetent mice or rats that carry syngeneic tumors and immunocompromised mice or rats that carry human xenograft tumors. Each model is known to have limitations that impaat on the ability to accurately predict responses in humans [41]. In terms of prediction of toxicity, subhuman primates (Aotus species) are thought to be fairly reliable in studying toxicity to HSV1 based oncolytic viruses. For adenoviruses, preclinical toxicity studies have used cotton rats and primates. Preclinical evaluation of anticancer efficacy and toxic effects for a particular oncolytic virus probably requires a combination of all these models.
Clinical Trials with Oncolytic Viruses
While most oncolytic viral products are still in the early phases of clinical development, data from a handful of trials are providing important leads about the best way to deliver therapeutic viruses. Both systemic and intratumoral routes of administration are explored. Intratumoral injections of agents like Onyx – 15 (an oncolytic adenovirus) provided some early encouraging results. Initial studies with the oncolytic viruses revealed that toxicity is generally restricted to pain at the injection site, transient fever. Responses with early crude materials were usually short in duration, however recent trials with gene – attenuated viruses suggest a more prolonged duration of responses [42].
As replication of human viruses is typically restricted to human cells, issues of tumor specificity and viral distribution cannot be fully addressed in animal models of cancer. Therefore, several research groups and companies have rapidly moved into clinical testing. Initial testing began with intratumoral injection and proceeded to intracavitary (such as intraperitoneal) and intravascular administration (such as hepatic artery fusion). More recently systemic (intravenous) applications are studies. Some of the important developments that are taking place in clinical trials will be briefly reviewed here. And Table-2 gives the summary of the clinical trials that are underway with various oncolytic viruses.
Oncolytic adenoviral trials
ONYX – 015 is extensively being explored for antitumor properties. Phase I trials for head and neck, ovarian, brain and prostate cancer are conducted and revealed minimal if any toxicity. Phase II trials for head and neck tumors have also been encouraging in terms of efficacy. Furthermore when ONYX – 015 is injected intratumorally and the chemotherapeutic agents 5 – fluorocytosine or cisplatin were co –administered systemically, more than half of the treated patients showed a partial or complete response for more than six months. These clinical findings in spite of the relatively attenuated oncolytic potency displayed by the oncolytic virus provide reassurance that additional refinements in OV technology will result in a therapeutically useful agent.
Oncolytic HSV1 trials
G207 is a herpes simplex virus (HSV) mutant with defects in both Ul39 and ICP34.5 expression. G207 is tested in a Phase I clinical trial in patients with recurrent malignant gliomas. Administration was carried out by direct stereotactic injection into the tumor. Doses of upto 3 x 100 infectious units were well tolerated. This trial showed that inoculation of an OV, the wild type counterpart’s main pathogenic effect of which is encephalitis remained relatively safe in human brain.
1716 is an HSV1 mutant with a disruption in the γ34.5 gene, which encodes PKR inhibitor ICP 34.5. This oncolytic virus was also well tolerated at doses upto 105 infectious units after stereotactic injection into recurrent malignant gliomas. Analysis of tumor explants revealed viral replication at 4-9 days after injection and the amount of recovered virus exceeded the input dose in at least some patient samples [43].
Oncolytic Newcastle Disease Virus
The Newcastle disease virus strain PV706 was recently evaluated with systemic intravenous administration as part of a Phase I, dose escalation trial in 79 patients that had various advanced solid malignancies [44]. Several different schedules were used including single and repeat dose regimens given over a period of 2 to 4 weeks. Dose limiting toxicities included diarrhea, dyspoenea, hypotension and tremors. Interestingly it is found that the administration of an initial dose of 12×109 infectious units/m2 – known as desensitizing dose – allowed for increase of subsequent doses upto 120×10 units/m2, even when the second dose was given only 2 days latter. This phenomenon of desensitization was thought to be due to development of human tolerance to toxicity caused by the cytokine/acute phase responses. Tumor progression did not occur in 14 out of 62 patients for 4-30 months after treatment. This trial established important toxicity profiles that might be encountered during, systemic administration of OVs and illustrates how desensitizing doses of OVs might allow for increases in overall dosage.
Oncolytic human reovirus – Reolysin (Trade name) – represents another virus that is being engineered for oncolytic activity. Reolysin is now in phase I/II development and has been demonstrated to replicate specifically in tumor cells bearing an activated Ras pathway. Treatment with reovirus has demonstrated an extremely positive safety profile. Testing on both animals and humans has indicated that reovirus is effective in the treatment of cancer [45].
Advances in OV technology
Multimode therapy is generally more effective than single agent treatment for cancer. Even if replication competent viruses are deemed sufficiently safe and efficacious in human clinical trials, it is unlikely that they will be used alone for the treatment of cancer. Indeed, evidence from both preclinical and clinical studies suggests that combining replication competent viruses with standard anti cancer treatments such as chemotherapy and radiotherapy will result in greater therapeutic benefit. Some of the developments in this regard will be mentioned here.
Combining Ovs with standard chemo or radiotherapy
Clinical trials with ONYX – 015 seem to reaffirm this concept of combination therapy. Various preclinical studies have shown that combining chemotherapy with OV administration results in augmented anticancer effects. In a few cases the rationale for such effects is known. For example, the anticancer and immunosuppressive agent cyclophosphamide facilitates infection of glioma xenografts by oncolytic HSV1 by partially inhibiting complement activation against the virus [46]. In another example, treatment with fluorodeoxyuridine (FUDR) – an inhibitor of cellular thymidylate synthase that is responsible for conversion of deoxyuracil monophosphate (dUMP) and cytosine diphosphate (CDP) to dTTP – stimulates mammalian ribonucleotide reductase activity due to loss of feedback inhibition by dTTP [47]. Increased ribonucleotide reductase activity therefore enhances replication of an u139 mutant HSV1.
Radiation was also shown to be effective in combination with OV therapy. Several HSV1 mutants act synergistically with radiation therapy although in some studies the effect of radiation was primarily additive. The anticancer effects of a combination an oncolytic adenovirus and radiation were also shown to be more potent than either treatment alone.
Improving OV efficacy with Cytotoxic Genes
Ov efficacy can be improved by adding cytotoxic genes to the viral genome to couple gene based therapy with viral oncolysis. In this respect OV technology might solve on the problems in gene therapy – the inefficiency of gene delivery. Replication defective, viral based gene therapy vectors distribute poorly within tumor mass and therefore fail to deliver such cytotoxic genes efficiently [48]. Experimentally it was found that transgene delivery by an OV reached an anatomically larger area of tumor compared with that reached by replication defective viral vector.
Ganciclovir is a guanosine analogue that is used as a prodrug to induce suicide of cells transfected with HSV1 thymidine kinase gene. Including this gene in HSV1 – based OV and combining viral infection of tumor cells with ganciclovir treatment enhanced its anticancer action in a rat 9L solid brain tumor model as well as in other models when compared with OV therapy alone [49]. Similarly combining a replicating adenovirus that expresses thymidine kinase with ganciclovir treatment enhanced anticancer activity; however combining oncolytic viruses that express thymidine kinase with ganciclovir treatment was not effective in all models [50].
The ability to include anticancer cDNA in OVs represents the potential for achieving multimode cancer treatment. OVs that contained two anticancer cDNA that activated two different anticancer prodrugs were more effective in killing tumor cells than when only one prodrug was added[51]. Even tumor cells that were not infected with the OV were killed by the bystander effects of the anticancer gene products. Levels of therapeutic metabolites that were generated within the tumor by the action of the OV were increased compared with levels in the systemic circulation – even when the prodrug was delivered locally. Attempts at discovering combinations of prodrugs that act synergistically might also facilitate such efforts.
Oncolytic Viral Delivery with Carrier Cells
Carrier cells are being developed that can be loaded with OVs and used to deliver specifically to tumor cells. The carrier cell strategy offered a number of advantages. The loaded cells will sustain the expression of the virus for longer period of time than what is possible with the administration of the oncolytic virus as such. Also the spread of the virus from the injection site to the peripheral organs will be minimized. Compared to direct virus injection, the carrier cell protocol leads to an improved therapeutic effect (metastases suppression) and a lesser generation of virus neutralizing antibodies.
Some of the carrier cells that are explored include – mesenchymal progenitor cells (MPC) and teratocarcinoma cells. These cells after they are loaded can be inactivated by gamma irradiation and this treatment was found not to affect the production and release of the virus. These cell-based systems are investigated to deliver oncolytic paroviruses that were capable of lysing neoplasm in Morris Hepatoma lung metastases [52]. Also MPCs loaded with Adenovirus – Ad5/3 caused total cell killing of ovarian cancer cells. These MPCs were also found to be undergoing preferential homing to the tumor cells thereby reducing the overall load to be administered of the oncolytic virus.
What are the effects of the Immune system on OVs
A relatively controversial topic relates to the effect of the immune system response to viral oncolysis. The reports of the effects of immune system are slightly contradictory. In some studies [53] immunesuprression has been shown to improve vitl oncolysis probably enabling the OVs to escape the immune system and survive and then exert its effects on the tumor cells. Whereas in other report [54], a robust immune response produced antitumor vaccination effect. The actions of the multiple effector arms of the antiviral immune response might provide an explanation for these discordant findings. The initial infection and propagation phases of the virus within the tumor are met with hyperacute and acute immune response that probably limit oncolysis. In rats, transient complement and antibody depletion enhance oncolytic effects in the initial phases of the virus – tumor interactions. The innate immune response against the viral infection might also increase toxicity to the host because of toxic inflammatory effects of complement activation products and elevated cytokine levels such as IL-6 and TNF-α as is shown in a recent clinical trial study [44].
As tumors regress and tumor antigens are released into the circulaltlion – these antigens can be presented to and activate CD4 and CD8 T cells and this leads to the immune destruction of any residual or subsequent tumors [54]. Pharmacological modulation or genetic alteration of OVs can be used to activate or inhibit different immune phases of viral infection and propagation within tumors and to elicit along lasting immune responses against residual and recurrent tumors.
Challenges of Oncolytic Virotherapy
One of the greatest challenges of oncolytic therapy and of gene therapy in general is the efficient delivery of the viral vector to the tumor. There are several factors that could hamper the efficient spread of the OVs within the solid tumor mass. Physical barriers such as the necrotic areas within the infected tumor, normal stroma cells and extra cellular matrix or the presence of basal membrane could limit the distribution and infection by the virus. Also the physical size of the administered virus particle and their interactions with the receptors that are present on the normal cells could be crucial. New delivery techniques such as convention – enhanced delivery (CED) of drugs to the brain will need to be explored for oncolytic viral therapy to tumors (specifically brain tumor) to achieve a uniform virus distribution. Convection enhanced delivery enables potent therapeutic agents which would otherwise be too toxic to the body to be slowly and continuously infused into particular brain tumors through small plastic catheters. After surgery the drug is administered via catheters using an infusion pump over a period of several days and the catheters are removed. Tools need to be developed that facilitate enhanced virus administration within the tumor using several simultaneous needle injections.
Another major factor that can potentially lead to the rapid clearance of viruses from the blood stream could be the uptake into Kupffer cells which are extremely active phagocytic cells that line the walls of sinusoids in the liver. Also the injected oncolytic virus can be quickly inactivated by complement. But there are suggestions that the complement can be transiently neutralized by administration of cobra venom factor. In addition the use of virus mutants that incorporate complement resistance factors into the outer membrane, which therefore offers resistance to the complement is also suggested.
In addition sufficient expression of viral receptors on malignant cells is required for therapeutic efficacy – a factor that is identified as a potential limitation for oncolytic adenovirus i.e. the inability of the vector to infect the cells, which do not express the receptor. The coxsackie and adenovirus receptor (CAR) is down regulated in certain malignant glioma cells. This suggests that strategies to redirect adenoviruses to achieve CAR independent infection will be necessary to realize the full potential of adenoviral vectors for OV therapy.
Another important constraint is that genetically enhanced vectors may or may not adhere to their replication restriction in long-term applications. So the genomic stability of OV in culture or in vivo is also an important issue. There are reports [55] that viruses that carry deletions in the Hsyγ34.5 gene undergo mutations. Although such resulting mutants still retained the oncolytic activity [56], their emergence is a reminder that DNA rearrangements, mutations and recombinations can occur with OVs. This serves as a note of caution to researchers in this field that possible undesirable mutants can be generated.
Summary
Several oncolytic viruses (OVs) – viruses that selectively infect or replicate in cancer cells, but spare normal cells – have been identified. Replication competent viruses either naturally occurring or genetically engineered offer great promise for cancer treatment because of their ability to amplify themselves and spread within the tumor mass.
Over the past 15 years, new insights into the molecular mechanisms of viral cytotoxicity have provided the scientific rationale to design more effective Ovs. Recent trials using genetically engineered viral strains, such as adenovirus (ONYX-015and CV706) and herpes simplex virus (G207 and 1716), as well as wild-type Newcastle disease virus (PV701) have been encouraging, showing these viruses to be relatively non-toxic and tumor specific.
Combination of oncolytic virotherapy with traditional chemotherapy significantly enhances the efficacy of virotherapy on a synergistic basis. In parallel additional antitumor mechanisms are applied to oncolytic viruses to arm them with therapeutic transgenes (e.g. prodrug – converting enzymes and antiangiogenic or immunomodulatory proteins) that induce bystander effects that are capable of eliminating tumor cells that are not directly killed through viral oncolysis alone.
The main goals of oncolytic viral research are to increase tumor selectivity by modifying the viral genome, to combine oncolytic viral therapy with standard radiation and chemotherapy, and to ‘arm’ the viruses with suicide cDNAs and/or cytokine cDNAs for multimode treatment.
A better understanding of mechanisms that viruses use to overcome cellular defenses in order to achieve robust replication within the cell will lead to the development of oncolytic viruses with better tumor specificity and reduced toxicity. Significant progress is made in targeting viruses to certain cell types but a truly tumor specific virus with a good strain stability is yet to be constructed.
The availability of systemic therapy in conjunction with oncolytic viruses will enhance the potential of oncolytic viruses to become a viable new therapeutic approach for the treatment of cancer. It is likely that in the future a range of viruses that target different cells will become available in the fight against cancer.
Refrencess
- Ring C.J.A.Cytolytic viruses as potential anticancer agents. J.General Virol. 83: 491 – 502 (2002).
- Ries S.J. and Brandts C.H. Oncolytic viruses for the treatment of cancer: current strategies and clinical trials. Drug Disc. Today 9,759 – 768 (2004).
- Wilder O.Comparison of replication selective, oncolytic viruses for the treatment of human cancers. Curr Opin Mol Ther. 5,351 – 361 (2003)
- Weises R.Aral Carcinogenesis: Aetiologic leads in The Text book of Oncology, 1st ed.Batch Press, New York, pp.147 – 151 (1995).
- Balmer C and Valley A.W.Basic principles of cancer treatment and cancer chemotherapy in Pharmacology – A Pathophysiologic approach, 2nd ed. Appleton and Lange, Connecticut, pp 1879-1881 (1993)
- Collins F.S. and Trent J.M.Medical Virology in Harrison’s Principles of Internal medicine, 15th ed., McGraw Hill Companies Inc. USA, pp 503, (2001)
- Salmon S and Sarterelli A.C. Cancer Chemotherapy in Basic and Clinical Pharmacology, 8th ed., Lange Medical Books/McGrawHill companies, Inc. USA pp 923-924
- Guttam B.s. in Biology 1st ed., McGraw Hill Companies Inc. USA pp 412-415
- Raven P.H. and Johnson G.B.in Biology 5th ed., McGraw Hill Companies Inc., USA, 99 339-343
- Brock T.D.and Madigan M.T.in Biology of Microorganisms, 6th ed., Prentice Hall Englewood Cliffs, New Jersey, pp 216-217
- Bullock B.L. an Rosendahl P.P.pathophysiology : Adaptations and Alterations in Functions 2nd ed., Scott Foreman & Company, USA, pp 196-197
- Clifford G.M., Smith J.S. and Franceschi S.Human papilloma virus types in invasive cervical cancer worldwide Br.J.Cancer 88,63 – 73 (2003)
- Bell J.C.and Stojdl D. Getting oncolytic viruses off the ground. Cancer 4,7-11 (2003)
- Bergland E.K. and Venook A.P shedding old paradigms – developing viruses to treat canacer J.Clin. Oncology 20,2230-2222 (2002)
- http://www.37c.comcn/topicoo4/spotlight trace/11.htm, Oncology: Training viruses to attack cancers
- Mullen J.T. and Tanabe K.K. Viral Oncolysis. The Oncologisit 7,106-109 (2002)
- http://www.37c.comcn/topic004/spotlight trace/11.htm, Oncology: Training viruses to attack cancers.
- http://www. pharmiweb.com/Features.asp row ID541 Developments in oncolytic viruses – an emerging approach to cancer therapeutics
- Rogers C.S., Sullengar B.A. and George A.L.Gene therapy in Goodman & Gilman The Pharmacological basis of therapeutics 10th ed. McGraw Hill, USA pp 87-89 (2001)
- Obuchi M., Fernadenz M. and Barber G. Development of recombinant vesicular stomatitis viruses that exploit defects in host defense to augment specific oncolytic acitivity.J.Virol.77, 8843-8856 (2003).
- Rommelaere, J. & Tattershall, P. Oncosuppression by parvoviruses, pp.. In Handbook of Parvaviruses,. Edited b P. Tijssen. Boca Raton, FL: CRC Press. 41-57 (1990).
- Hammon, W.Mc.D., Yohn, D.S., Casto, B.C. and Aitchison, R.W.Oncolytic potentials of nonhuman viruses for human cancer: effects of twenty-four viruses on human cancer cell lines. Journal of the National Cancer Institute 31,329-3453 (1963).
- Flanagan, A.D., Love, R. and Tesar, W. Propagation of Newcastle disease virus in Ehrlich ascites cells in vitro and in vivo. Proceedings of the Soceity for Experimental Biology and Medicine 90, 82-86 (1955).
- Lindblom, A. and Liljegren, A.Tumour markets in malignancies. British medical Journal 320, 424-427 (2000)
- Nettelbeck, D.M., Jerome, V.&Muller, R.Gene therapy: designer promoters for tumour targeting. Trends in Genetics 16,174-181. (2000)
- Bergelson, J.M. Isolation of a common receptor for coxsackie B viruses and adenoviruses 2 and 5. Science 275, 1320-1323 (1997)
- Wickham, T.J., Mathias, P., Cheresh, D.A. and Nemerow, G.R.Integrins romote adenovirus internalization but not virus attachment. Cell 73, 309-319 (1993).
- Yang, C.T.p14 (arf) modulates the cytolytic effect of onlyx-015 in mesothelioma cells with wild-type p53. Cancer Res. 61,59959-5963 (2001).
- Mc Cormick, F.ONXY-015 selectivity and the p14ARF pathway. Oncogene 19, 6670-6672(2000).
- McCormick, F.Cancer therapy based on p53. Cancer J.Sci. Am.5, 139-144 (1999).
- Mundschau, L.J. and Faller, D.V. Platelet-derived growth fator signal transduction through the interferon-inducible kinase PKR.Imediate early gene induction.J.Biol.Chem.270, 3100-3106 (1995).
- Li, Y.A hepatoellular carcinoma-specific adenovirus variant, CV890, eliminates distant human liver tumors in combination with doxorubicin. Cancer Res.61, 6428-6436 (2001).
- Doronin, K.et al. Tissue-specific, tumor-selective, replication-competent adenovirus vector for cancer gene therapy. J. Virol. 75,3314-3324 (2001).
- Kurihara, T., Brough, D.E., Kovesdi, I.andKufe, D.W. Selectivity of MUC1 antigen. Journal of Clinical Investigation 106,763-771. (2000).
- McCart, J.A.. Systemic cancer therapy with a tumorselective vaccinia virus mutant lacking thymidine kinase and vaccinia growth factor genes. Caner Res.61,8751-8757 (2001).
- Gromeier, M., Lachmann, S., Rosenfeld, M.R., Gutin, P.H.& Wimmer, E.Intergeneric poliovirus recombinants for the treatment of malignant glioma. Proc. Natl Acad.Sci USA 97, 6803-3808 (2000)
- Frote, D.et al. Lice attenuated measles virus induces regression of human lymphoma xenografts in immunodeficient mice. Blood 97,3746-3754 (2001).
- Bluming, A.Z. and Ziegler, J.L.Regression of Burkitt’s lymphoma in association with measles infection. Lancet 105-107 (1971).
- Asada, T.Treatment of human cancer with mumps virus. Cancer 34, 1907-1928 (1974).
- Andreansky, S.. Evaluation of genetically engineered herpes simplex viruses as oncolytic agents for human malignant brain tumors. Cancer Res. 67,1502-1509 (1997).
- Barth, R.F.Rat brain tumor models in experimental neurooncology: the 9L, C6, T9, F98, RG2 (D74), RT-2 and CNS -1 gliomas . J.Neurooncol. 36,91-102 (1998)
- Newmanaitis J.J.Cancer tareatment involving oncolytic viruses Clin Lung Cancer 1,50-55 (1999)
- Papanastassiou, V.. The potential for efficacy of the modified (ICP 34.5)- herpes simplex virus HSV11716 following intratumoural injection into human malignant glioma: a proof of principle study. Gene Ther. 9,398-406 (2002).
- Pecora, A.L.et al. Phase I trial of intravenous administration of PV 701, an oncolytic virus, in patients with advanced solid cancers. J.Clin Oncol.20,2251-2266 (2002).
- http://www.cancercompass.com/message-board/message/all,1326.0htm New treatment
- Ikeda, K. Complement depletion facilitates the infection of multiple brain tumors by an intravascular, replication conditional herpes simplex virus mutant.J Virol. 74,4765-4775 (2000).
- Petrowsky, H. Functional interaction between fluorodeoxyuridine-induced cellular alterations and replication of a ribonucleotide reductase-negative herpes simplex virus.J.Virol 75,7050-7058 (2001).
- Harsh, G.R. et al. Thymidine kinase activation of ganciclovir in recurrent malignant gliomas: a gene-marking and neuropathological study.J. Neurosurg. 92,804-811 (2000).
- Kasuya, H Intraperitoneal delivery of hrR3 and gancicloviir prolongs survival in mice with disseminated pancreatic cancer.J.Surg.Oncl 72,136-141 (1999).
- Carroll, N.M., Chase M., Chicca, E.A. and Tanabe, K.K. the effect of ganciclovir on herpes simplex virus-mediated oncolysis J.Surg. Res. 69,413-417 (1997).
- Aghi, M., Chou, T.C., Suling, K., Breakefieldl, X.O. and Chiocca, E.A. Multimodal cancer treatment mediated by a replicating oncolytic virus that delivers the oxazaphosphorine/rat cytochrome P450 2B1 and ganciclovir/herpes simplex virus thymidine kinase gene therapies. Cancer Res. 59,3861-3865 (1999).
- Komarova S. and Kawakami Y. Mesenchymal progenitor cells as cellular vehicles for delivery of oncolytic adenoviruses Mol. Cancer Ther. 5(3), 7750766 (2006).
- Ikeda, K.Oncolytic virus therapy of multiple tumors in the brain requires suppression of innate and elicited antiviral responses. Nature Med. 5,881-887 (1999).
- Todo, T. Systemic antitumor immunity in experimental brain tumor therapy using a multimutated, replicationcompetent herpes simplex virus. Hum Gene Ther. 10,2741-2755 (1999).
- He, B..Suppression of the phenotype of (1)34.5-herpes simplex virus 1: failure of activated RNA-dependent protein kinase to shut off protein synthesis is associated with a deletion in the domain of the 47 gene. J.Virol.71,6049-6054 (1997).
- Mohr, I.A herpes simplex virus type 1 34.5 secondsite suppressor mutant that exhibits enhanced growth in cultured glioblastoma cells is severely attenuated in animals J. Virol 75,5189-5196 (2001).







