Poorani Pazhanivel , Ganapathy Sankar Umaiorubagam*
, Ganapathy Sankar Umaiorubagam* and Monisha Ravikumar
and Monisha Ravikumar
SRM College of Occupational Therapy, SRM Institute of Science and Technology, SRM Nagar, Kattankulathur, Chengalpattu district, Tamil Nadu- India
Corresponding Author E-mail:ganapatu@srmist.edu.in
DOI : https://dx.doi.org/10.13005/bpj/3140
Abstract
Aim: To compare the Vestibular Rehabilitation therapy on balance with and without conventional occupational therapy for adult with hearing impairment. Method: Quasi-experimental pre-post test study design was used, 8 young adults between 18 to 24 years of age were recruited, assigned to vestibular rehabilitation therapy group (n=4) and conventional therapy group (n=4) respectively. Participants from the vestibular rehabilitation therapy group underwent vestibular rehabilitation therapy exercise for balance focusing on gaze stability and postural stability, along with conventional therapy for balance for a duration of 4 weeks, whereas conventional therapy group received conventional occupational therapy on balance for the same period. Outcome measures to assess balance were Berg balance scale (BBS), Timed Up and Go test (TUG) and Functional Reach Test (FRT) was used. Results: there was a statistically significant difference between the post-test scores of BBS -static, Dynamic, total, TUG, and FRT between the control and experimental group. The results depicted that vestibular rehabilitation therapy with conventional occupational therapy had an more effect on balance for persons with hearing impairment than conventional occupational therapy for balance. Conclusion: The study concludes that vestibular rehabilitation therapy with conventional occupational therapy had shown to be effective on balance for young adults with hearing impairment. This study recommends continuous follow-up of participants to identify the effects of vestibular rehabilitation therapy on balance in other functional activities of individuals.
Keywords
Balance; Hearing impairment; Vestibular rehabilitation therapy; Young adult
Download this article as:| Copy the following to cite this article: Pazhanivel P, Umaiorubagam G. S, Ravikumar M. Vestibular Rehabilitation Therapy with and Without Conventional Regimen on Balance for Adult with Hearing Impairment: Pilot Study. Biomed Pharmacol J 2025;18(1). |
| Copy the following to cite this URL: Pazhanivel P, Umaiorubagam G. S, Ravikumar M. Vestibular Rehabilitation Therapy with and Without Conventional Regimen on Balance for Adult with Hearing Impairment: Pilot Study. Biomed Pharmacol J 2025;18(1). Available from: https://bit.ly/3EijtZA |
Introduction
The vestibular system is essential to maintain human body balance. The auditory organ consists of a vestibulocochlear system which has a dual function. The cochlea part of the vestibular organ is responsible for the auditory or hearing function, and the vestibular system of the vestibular organ is responsible for maintaining the body in balance. When the vestibular part of the auditory organ is affected or presented with any disorder such as hearing loss the individual’s balance is affected1. While walking individual should have good postural stability which requires the combined use of two of the three sensory cues (visual, vestibular,somatosensory). The person with hearing impairment has deficits in vestibular function and the other two cues are also decreased which results in poor balance. This results in fall, balance disturbance while walking in the dark or low light area and on uneven surfaces, and also shows decreased ability to see clearly during head movements2. Studies reported that children and adolescents with hearing loss have presented with poor balance abilities when compared with hearing peers or individuals with normal hearing ability.
Vestibular rehabilitation therapy (VRT) is an exercise-based intervention program that includes different components that aim to improve a person’s balance, gait, and gaze stability and also helps in facilitating somatosensory integration 3. Vestibular rehabilitation therapy focuses on above three important components but different approaches consisting of exercises focusing on habituation, gaze stabilization, and postural stabilization to improve balance in vestibular dysfunction patients. Vestibular rehabilitation therapy is used for patients with balance disorders due to a vestibular origin. It used exercises that are aimed to optimize both static and dynamic postural stability under sensory conflicting conditions 4. It has been proven to be an effective therapy for improving balance in children diagnosed with vestibular disorders.
Vestibular rehabilitation therapy (VRT) has been reported to improve visual acuity, postural stability, and reduced disequilibrium during movement for people with hearing loss through different exercises. The exercises used for hearing loss in VRT aim to substitute for alternative strategies that compensate for the vestibular functional loss, also focus on improving vestibular functioning 5. Vestibular rehabilitation focuses on enhancing gaze stability, postural stability, and compensation strategies for people with hearing impairment. It uses combined intervention of gaze stabilization exercises and exercise for increasing somatosensory and visual information which results in improvement for postural stability and also focuses on compensatory strategies which are used during situations where balance is stressed to the maximum 6.
Vestibular rehabilitation therapy (VRT) found to be effective for balance in different populations such as stroke, traumatic brain injury, BPPV, sensorineural hearing loss.The vestibular and visual system plays a major role in improving postural stability which is then based on the maintenance of balance7. The functional maturation of the visual system and vestibular system for postural stability and control of the system continues through fifteen years of age.
The effectiveness of postural control is less mature during the seven years of age but for vestibular system’s effectiveness in the control of posture that results in improving the balance of individual continues to develop beyond fifteen years of age 8. Considering this age, and as brain neural plasticity is at the peak during early development and reduces after 7 years of age, as well as the scarcity of VRT studies in the Indian context 8, the present study was designed to examine the effectiveness of ibular rehabilitation therapy on balance in young adults with hearing impairment.
Material and Methods
This study obtained approval from the institutional Ethical committee of SRM Medical College Hospital and Research Centre. Ethical Clearance No: 2080/IEC/2020. It was a Quasi-experimental study design. The inclusion criteria were: Younger adults with severe to profound hearing impairment; Age between 18 and 24 years; Both male and female; Berg Balance Scale (BBS) score ≤45 . Younger adults with any physical difficulties were excluded from the study.
Procedure
The purpose of the study was explained to all the subjects and a written consent form was obtained. Eight younger adults (n=8) with hearing impairment between the ages of 18 to 24 years were recruited through the convenience sampling method. The subjects were randomly grouped into a vestibular rehabilitation therapy group (n =4), and conventional occupational therapy group (n =4). The procedure was explained and communicated with the help of a teacher who knows sign language.Berg balance scale, functional reach test, timed up and go test was used to measure at baseline (pre-test). Both the groups received intervention for a period of 4 weeks. At the end of 4 weeks, post-test was done by administering Berg balance scale, timed up and go test, and functional reach test. The intervention was carried out for a period of 4 weeks consists of 5 sessions, 5 times a week. Each session was held for 45 min. Post-test was done after the 18th session. Experimental group received vestibular rehabilitation therapy focusing on gaze stabilization and postural control, along with conventional occupational therapy on balance the exercises for the conventional therapy were first demonstrated by the therapist then it was performed by the client. For the first 2 weeks phase, one balance exercise was given as an intervention. From the 3rd and 4th week phase two balance exercises were performed by the participants.
Berg balance scale
The Berg Balance Scale (BBS) is an objective measure of dynamic and static balance. It was developed 1989 and it consists of 14 daily living balance tasks of which six and eight measures the static and dynamic balance components of an individual. The following are the 14 tasks performed by the individual through the therapist instruction: sit to stand, stand to sit, various standing positions, sitting unsupported, standing unsupported, forward reach, feet together, retrieving an object from the floor, standing on one foot, and placing the fool on a step or stool. The task performances are evaluated by the therapist and scoring is done 9 . The scoring is done by a five-point scale (graded 0–4) 4 indicated that the patient was able to perform independently, able to meet time and distance criteria and a score of 0 indicated that the patient was unable to perform. The total score on this scale is 56.A score of < 45 indicates a greater risk of falling.The content validity of this scale concerning geriatrics patients and health professionals is good. The concurrent validity with Tinetti balance subtest is 0 .91, Barthel mobility is 0 .67and TUG is 0.76. The reliability (ICC), Inter-rater reliability is 0.98 and intra-rater reliability is 0.99. Item of Individual ranged from .71 to .99. The Internal consistency of the scale, Cronbach’s alpha is 0 .96. This scale is used before and after the intervention to check the effect of the intervention10.
Functional reach test (FRT)
Functional reach test (FRT) is a single task test developed in 1990 and it measures the static balance ability of the individual. The scale examines forward upper extremity reach with the shoulder at 90° flexion, feet still. This test focuses on the following: Postural responses related to voluntary upper extremity movement and Limits of Stability (LOS). Scoring is based on distance reached in inches. It uses 1 practice and 3 trials. The scoring is based on the average of the 3 trials. Norm value for Functional reach test between the age 20 -40 years male is 16.7(±1.9) and for a female is 14.6 (±2.2) .The content validity: expert consensus, concurrent validity, duke mobility is 0.65, and gait speed is 0.71. The reliability (ICC) of this scale, interrater is 0.98, and interrater reliability is 0.92 11.
Timed up and go test (TUG)
The Timed up and go test is a single task test developed in 1986 and it measures the dynamic balance and mobility of an individual. It evaluates a person’s balance by therapist instructing them to complete the following tasks: Stand up, walk for 3 meters (10 feet), turn around, and return to the chair. The TUG test evaluates the time taken by the individual to complete the task in seconds .The test uses 1 practice and scoring is done by measuring the average of 3 trials. Healthy adults can complete the test in less than 10 seconds. Scores of 11 to 20 seconds are considered typical for frail individuals with a disability. Scores over 30 seconds are indicative of impaired functional mobility and high fall risk.The content validity of this test has achieved expert consensus, concurrent validity with BBS is 0.81, Barthel is 0.78. The reliability of this scale, inter-rater is 0.99, intra-rater is 0.9812.
Intervention – Vestibular rehabilitation therapy
Vestibular rehabilitation therapy focuses on improving postural stability and decreasing disequilibrium for people with hearing impairment. It aims to provide alternative strategies for vestibular function loss and also improve the remaining function. The vestibular rehabilitation protocols involve a combined use of gaze stabilization exercises and exercises to improve postural stability which results in enhancement of balance control among the hearing-impaired population 13.
Gaze stability exercises are used for gaining compensatory eye movements during active and passive head movements which are diminished in patients with hearing loss. This is done through different mechanisms such as the central pre-programming mechanism and saccadic and pursuit eye movement which act as a substitution for vestibular loss during activities such as perturbation while walking 14. The purpose of postural stability exercises was to develop strategies for performing daily activities when there is a loss or reduced vestibular input. Patients with hearing impairment showed less stability when they were asked to turn their head while walking, this is because they rely more on visual cues to maintain postural stability and when the head moves, the visual cue is degraded which results in disturbed balance 15. The experimental group was given vestibular rehabilitation therapy along with conventional balance training.
Intervention – Conventional occupational therapy for balance
The intervention for the conventional occupational therapy group on balance focuses on two sets of exercises with a gradual increase in the number of repetitions and the compliance for the improvement of balance. This protocol is from a study which focused on the effectiveness of occupational therapy intervention for balance.
Results
The data analysis was computed using the software version SPSS 24.0. (SPSS, Inc, Chicago, IL). The significance level was set at 0.005 for the analysis.
Table 1: Comparison of pre-test scores of BBS-Static, Dynamic,Total, TUG, and FRT between control and experimental group
|
Outcome measures |
Group |
Mean |
Std. Deviation |
µ -Value |
p-Value |
|
|
BBS |
Static |
Control |
26.00 |
1.826 |
-0.899 |
0.369 NS |
|
Experimental |
27.00 |
1.414 |
||||
|
Dynamic |
Control |
15.75 |
.500 |
-1.423 |
0.155 NS |
|
|
Experimental |
15.00 |
.816 |
||||
|
Total |
Control |
41.75 |
1.500 |
-0.155 |
0.877 NS |
|
|
Experimental |
42.00 |
1.414 |
||||
|
TUG |
Control |
11.9500 |
.26458 |
-1.461 |
0.144 NS |
|
|
Experimental |
11.4750 |
.50580 |
||||
|
FRT |
Control |
12.7750 |
.97767 |
-0.577 |
0.564 NS |
|
|
Experimental |
12.9750 |
1.29968 |
||||
p≤0.05
Mann Whitney µ ‘ test was used to compare the pre-test scores of the experimental and control groups. The results showed that there was no statistically significance difference between the pre- test scores of the experimental and control groups in BBS – static, Dynamic, Total, TUG and FRT (u = -0.899, p = 0.369; u = -1.423, p = 0.155; u = -0.155, p = 0.877; u = -1.461, p = 0.144; u = -0.577, p = 0.564 respectively).
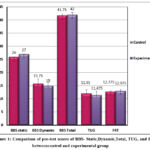 |
Figure 1: Comparison of pre-test scores of BBS- Static,Dynamic,Total, TUG, and FRT betweencontrol and experimental group
|
Table 2: Comparison of the post-test score of BBS- Static, Dynamic, Total, TUG, and FRT between control and experimental group
|
Outcome measures |
Group |
Mean |
Std. Deviation |
µ -Value |
p-Value |
|
|
BBS |
Static |
Control |
27.75 |
2.872 |
-2.678 |
0.007 S |
|
Experimental |
30.25 |
1.500 |
||||
|
Dynamic |
Control |
18.00 |
.816 |
0.000 |
1.000 NS |
|
|
Experimental |
18.00 |
.816 |
||||
|
Total |
Control |
45.75 |
2.217 |
-2.759 |
0.006 S |
|
|
Experimental |
48.25 |
1.708 |
||||
|
TUG |
Control |
10.2250 |
.78049 |
-2.021 |
0.043 S |
|
|
Experimental |
8.8000 |
.37417 |
||||
|
FRT |
Control |
13.6250 |
.96738 |
-2.871 |
0.004 S |
|
|
Experimental |
14.1250 |
1.08743 |
||||
p≤0.05
Mann Whitney µ ‘ test was used to compare the post-test scores of the experimental and control groups. The results showed that there was statistically significance difference between the post-test scores of the experimental and control groups in BBS – Static, Dynamic, Total, TUG and FRT (u = -2.768, p = 0.007; u = 0.000, p = 1.000; u = -2.759, p = 0.006; u = -2.021, p = 0.043; u = -2.871, p = 0.004 respectively).
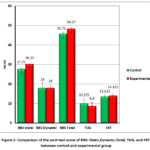 |
Figure 2: Comparison of the post-test score of BBS- Static,Dynamic,Total, TUG, and FRT between control and experimental group
|
Discussion
Table No. 1 and Figure No.1 show that there was no statistically significant difference between the pre-test score of BBS-Static, Dynamic, Total, TUG, and FRT between the control and experimental group. The results depict that there was no difference in the baseline performance between the control and experimental groups. Table No.2 and Figure No.2 show that there was a statistically significant difference between the post-test scores of BBS -static, Dynamic, total, TUG, and FRT between the control and experimental group. The results depicted that vestibular rehabilitation therapy with conventional occupational therapy had an effect on balance for persons with hearing impairment than conventional occupational therapy for balance. The results were similar to a previous study 1conducted in 2020 stated that when people with severe to profound hearing impairment with cochlear implantation were given a 4-week vestibular rehabilitation therapy intervention consists of habituation and adaptation exercise for balance and gait stability showed a significant effect on balance, postural stability and reported to improve participant’s functional recovery. A study9 stated that vestibular rehabilitation therapy focusing on compensatory training, visual enhancement, somatosensory function and balance training for children with bilateral vestibular dysfunction given for a duration of 8 weeks showed significant improvement in the vestibular function, postural stability, and balance abilities.
Two sets of balance training exercise protocol were given for the control group (conventional occupational therapy group). This balance training exercise is reported to stimulate the neuromuscular system, vestibular system, and proprioceptive system that sends signals to the vestibular nuclei and cerebellum. This causes the activation of the vestibular system which results in enhancing the balance ability, postural, and improving the overall quality of movement of individuals 16. Whereas vestibular rehabilitation therapy focuses on improving the vestibulo-ocular (VOR) and vestibular spinal reflex (VSR) which are responsible for visual and body stability during movement. VOR is responsible for the activation of ocular motor nuclei which results in stimulation of extraocular muscle of the eye during eye movement to maintain visual stability. VSR is responsible for the activation of anterior horn cells of the spinal cord results in the stimulation of skeletal muscle through the lateral vestibulospinal tract, medial vestibulospinal tract, and reticulospinal tract which results in maintenance of balance. As vestibular rehabilitation therapy focuses on vestibular reflex to maintain balance it is more effective than conventional balance therapy. The results of the study show that vestibular rehabilitation therapy improves both static and dynamic balance among young adults with hearing impairment while conventional occupational therapy had an effect on static balance in young adults with hearing impairment 17.
There were some study limitations that have been described. Firstly, the sample size was small, and a convenience sampling technique was used, hence generalization of the effectiveness of vestibular rehabilitation therapy was poor. Secondly, Due to the pandemic, the study duration was reduced, the setting of the study was changed from institutional setting to home visits and follow-up was not possible. Accessibility was difficult to participants’ places due to restrictions in transportations. This study is in accordance with other literature findings was able to determine and nurtures the knowledge on the effect of vestibular rehabilitation therapy on balance in young adults with hearing impairment. Vestibular rehabilitation therapy aids to improve balance and postural defects in hearing-impaired individuals. One of the clinically relevant findings of this study was that the use of vestibular rehabilitation therapy for the age group between 18 to 24 years showed improvement in static and dynamic balance for individuals with hearing impairment. This shows that vestibular rehabilitation therapy can be used for improving balance in young adults with hearing impairment.
Conclusion
This research attempts to explore the effect of vestibular rehabilitation therapy on balance for young adults with hearing impairment. Young adults with hearing impairment are reported to have reduced balance ability due to defects in the vestibular system. The vestibular system consists of two components cochlear and vestibular systems, in which the vestibular system is responsible for maintaining balance. Individuals with hearing impairment were reported due have defects in the vestibular system which results in reduced balance ability. Vestibular rehabilitation therapy is a exercises programs that focus on improving the vestibulo-ocular reflex and vestibulospinal reflex which results in improvement of balance and postural stability among individuals with hearing impairment. The study concludes that vestibular rehabilitation therapy with conventional occupational therapy had shown to be effective on balance for young adults with hearing impairment.
This study recommends continuous follow-up of participants to identify the effects of vestibular rehabilitation therapy on balance in other functional activities of individuals. Further researches can be conducted with a larger sample size to generalize the results. Study can be conducted for a longer duration.
Acknowledgement
We would like to thank all participants in this research and Authorities of SRM College of Occupational Therapy, SRMIST to grant permission to conduct this research.
Funding Sources –
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Conflict of Interest
The author(s) do not have any conflict of interest.
Data Availability Statement
This statement does not apply to this article.
Ethics Statement
This study obtained approval from the institutional Ethical committee of SRM Medical College Hospital and Research Centre. Ethical Clearance No: 2080/IEC/2020
Informed Consent Statement-
This study did not involve human participants, and therefore, informed consent was not required.
Clinical Trial Registration-
This research does not involve any clinical trials
Author Contributions
Poorani Pazhanivel : Conceptualization, Methodology and data collection
Ganapathy Sankar Umaiorubagam: Methodology, Supervision, Writing-Review & Editing
Monisha Ravikumar: Original manuscript writing & proof reading, Editing
References
- Romita Fernandes, Shalini Hariprasad, Vijaya K Kumar.Physical therapy management for balance deficits in children with hearing impairments: A systematic review: Balance rehabilitation in deafness. Journal of Paediatrics and Child Health. 51(8).,753-758.
CrossRef - Berg, K., Wood-Dauphine, S., Williams, J. I., & Gayton, D. Measuring balance in the elderly: preliminary development of an instrument. Physiotherapy Canada, 1989.41(6), 304-311.
CrossRef - Byng In Han. Vestibular Rehabilitation Therapy: Review of Indications, Mechanisms and Key exercises. Journal of Clinical Neurology, 2011.Dec 29,189-196
- Duncan, P. W., Weiner, D. K., Chandler, J., & Studenski, S. Functional reach: a new clinical measure of balance. Journal of gerontology, 1990.45(6), M192-M197.
CrossRef - Dunsky A. The Effect of Balance and Coordination Exercises on Quality of Life in Older Adults: A Mini-Review. Front Aging Neurosci. 2019;11:318.
CrossRef - Melo RS, Marinho SEDS, Freire MEA, Souza RA, Damasceno HAM, Raposo MCF. Static and dynamic balance of children and adolescents with sensorineural hearing loss. Einstein (Sao Paulo). 2017,15(3):262-268.
CrossRef - Cardon G, Campbell J, Sharma A. Plasticity in the developing auditory cortex: evidence from children with sensorineural hearing loss and auditory neuropathy spectrum disorder. J Am Acad Audiol. 2012,23(6):396-411.
CrossRef - Mathias S, Nayak US, Isaacs B. Balance in elderly patients: the “Get-Up and Go” Test. Arch Phys Med Rehabil, 1986.67, 387–389.
- Saki N, Abshirini H, Karkhaneh S, Bayat A. Investigating the Effects of Vestibular Rehabilitation on Balance Function in Cochlear Implant Recipients. Int Tinnitus J. 2020, 24(1):36-39.
- Podsiadlo, D., & Richardson, S. The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. Journal of the American Geriatrics Society, 1991.39(2), 142-148.
CrossRef - Melo RS, Lemos A, Paiva GS, Ithamar L, Lima MC, Eickmann SH, Ferraz KM, Belian RB. Vestibular rehabilitation exercises programs to improve the postural control, balance and gait of children with sensorineural hearing loss: A systematic review. Int J Pediatr Otorhinolaryngol. 2019 ;127:109650
CrossRef - Rine RM, Cornwall G, Gan K, LoCascio C, O’Hare T, Robinson E. Evidence of progressive delay of motor development in children with sensorineural hearing loss and concurrent vestibular dysfunction. Percept motor skills,2000, 90: 1101-12.
CrossRef - Susan J. Herdman. Vestibular Rehabilitation 3rd edition, 2007, Published by: A. Davis Company.
CrossRef - Garg S, Chadha S, Malhotra S, Agarwal AK. Deafness: burden, prevention and control in India. Natl Med J India. 2009 , 22(2):79-81.
- Tucci D, Merson MH, Wilson BS. A summary of the literature on global hearing impairment: current status and priorities for action. Otol Neurotol. 2010;31(1):31-41.
CrossRef - Rajendran V, Roy FG. An overview of motor skill performance and balance in hearing impaired children. Ital J Pediatr. 2011;37:33.
CrossRef - Wiegersma PH, Van der Velde A. Motor development of deaf children. J Child Psychol Psychiatry. 1983;24(1):103-111.
CrossRef








