Adinarayana Andy1 , Ravindra Pukharaj Choudhary2
, Ravindra Pukharaj Choudhary2 , Divya Andy3
, Divya Andy3  and Srikanth Malavalli Siddalingegowda2*
and Srikanth Malavalli Siddalingegowda2*
1Pharmacy Manager, Weatherwax Family Pharmacies Inc, Spring Arbor, Michigan, USA.
2Department of Pharmacy Practice, JSS College of Pharmacy, Mysuru, Karnataka, India
3Independent Research consultant, Michigan, USA.
Corresponding Author E-mail: mssrikanth@jssuni.edu.in
DOI : https://dx.doi.org/10.13005/bpj/3104
Abstract
Obesity is a serious public health issue globally. Over the past three decades, many nations have experienced a substantial surge in obesity rates and obesity related non-communicable diseases (OR-NCDs), which has a considerable economic impact worldwide. It is estimated that more than 2.5 billion adults aged 18 and older were overweight, with over 890 million obese. Several anti-obesity medications came to market but were underutilized due to lack of safety evidence and concerns over adverse effects. Medication-induced weight gain is distressing for both patients and healthcare providers, and it can make it challenging to select and manage treatment regimens. Moreover, there has been a noticeable increase in preventable adverse drug events linked to medication-induced weight gain or obesity being reported to adverse drug reporting systems. Despite the availability of clinical care standards for obesity treatment and management, the outcomes have not been optimal. Hence, there is a need for a comprehensive and holistic approach that involves the proactive engagement of all the stakeholders involved in the care process. Clinical pharmacists are one among the key stakeholders in weight gain and obesity management, significantly contributing at various stages of patient care and in bariatric surgeries. Numerous studies have shown that clinical pharmacist-led weight management services and interventions have optimized treatment benefits. This paper emphasizes the need for and the role of clinical pharmacists in managing obesity.
Keywords
Anti-obesity medications; Clinical pharmacy; Drug-induced weight gain; Obesity; Weight-management
Download this article as:| Copy the following to cite this article: Andy A, Choudhary R. P, Andy D, Siddalingegowda S. M. Optimizing Weight Management: A Collaborative Strategy with Clinical Pharmacists. Biomed Pharmacol J 2025;18(1). |
| Copy the following to cite this URL: Andy A, Choudhary R. P, Andy D, Siddalingegowda S. M. Optimizing Weight Management: A Collaborative Strategy with Clinical Pharmacists. Biomed Pharmacol J 2025;18(1). Available from: https://bit.ly/4jyFW4L |
Introduction
Obesity is a major public health concern worldwide. Over the last three decades, many countries have seen a substantial surge in obesity rates, likely due to sedentary lifestyles, urbanization, and higher consumption of calorie-dense processed meals. This chronic and complex condition can have debilitating effects and far-reaching implications for individuals and society as a whole1. Evidence suggests that the abnormal distribution of fat in obesity has been linked to chronic inflammation, increased blood clotting, and narrowed blood vessels, increasing the risk of stroke, hypertension, diabetes mellitus, heart disease and other complications, while also exerting a substantial impact on psychosocial health. Furthermore, obesity is also linked to greater mortality rates2. According to the 2017 Global Burden of Disease (GBD) study, having a BMI of ≥25 kg/m2 has been linked to 2.4 million deaths in women and 2.3 million deaths in men3.Therefore, it is crucial to prioritize the prevention of obesity to effectively control obesity-related non-communicable diseases (OR-NCDs) 1.
Obesity and overweight stand as the fifth leading risk factors that cause death worldwide4. Obesity prevalence is greatly influenced by age, gender, and ethnicity, as well as a variety of environmental, social, genetic, and biological factors that affect energy intake and expenditure4, 5.The majority of obesity cases are multifactorial, involving crucial factors like dietary patterns, physical activity, sleep patterns, medications, genetics, epigenetics, and environmental determinants. Monogenic obesity syndromes are rare, making up less than 5% of all obesity cases3. The World Obesity Federation predicts that 800 million people are currently obese, with 39 million being children under the age of 5years (2020) and 340 million being children and adolescents aged five to nineteen. Furthermore, an additional 1 billion individuals are susceptible to being overweight or obese6. Regional dissimilarities exists in the overweight prevalence, with 31% in the WHO Southeast Asia and African regions and 67% in the Region of the Americas7.
A recent estimate indicates that over 2.5 billion adults were overweight and over 890 million were obese in 20227.The rate of obesity worldwide has nearly doubled in last three decades. According to recent estimates, approximately 37 million children under the age of 5 years- were overweight and 16% of adults worldwide over the age of 18 years-were obese in the year 20228. Obesity is considered as most prevalent condition in the America, as it impacted 33% of adults and 17% of children, with a prevalence of 42.4% among adults in 2017-2018, including 42.1% for women and 43.0% for men1, 5. In Australia, approximately 30% of adults are obese, with 65% being overweight or obese9. In the United Kingdom, 67% of men and 60% of women were considered overweight or obese in 2018 10.The issue of overweight is no longer limited to high-income nations; it is also spreading to lower- and middle-income nations7. Over 135 million people in India are obese4. Overweight and obesity are prevalent among both adults and children in the Middle East and North Africa (MENA), with roughly 66% of females over the age of 20 being overweight11.
Materials and Methods
An extensive literature search is carried out in PubMed, Scopus, Web of Science, and Google Scholar databases and various medical search engines were used for exploring valid literature. The predefined search strategy was used to identify potentially relevant articles included in following aspects: weight management, drug-induced weight gain, Anti-obesity medications, clinical pharmacist role in weight management program and bariatric surgery. Mesh and text words were combined with Boolean operators “AND” and “OR”. The full search includes terms such as obesity, weight gain, drug-induced weight gain, obesogenic environment, economic burden, post-discharge care, collaborative approach, pharmacist interventions, direct care, patient-centered care, clinical pharmacist-led weight management program, bariatric surgery, obesity management.
Results and Discussion
Economic burden associated with obesity
Obesity has a significant economic impact. According to the Centers for Disease Control and Prevention (CDC), the total medical costs associated with adult obesity were $147 billion in 2008. Obese people spend 42% more on health care than normal-weight individuals, partly due to obesity-related health issues and risks. Medicare and Medicaid paid around $1000-1700 more for obese patients than for normal-weight adults. According to studies, obesity-related “absenteeism” and “presenteeism” cost up to $11 billion in productivity loss annually12.
Transportation expenses rose due to increased weight-based fuel requirements. In 2000, airlines incurred additional fuel expenses of around $275 million as a result of an rise in obese customers count. Several airlines, like Southwest Airlines and American Airlines, now require customers of a “certain size” to purchase two seats on the plane. The obesity epidemic has far-reaching economic consequences12. Furthermore, these individuals also confront serious challenges as a consequence of weight bias, such as discrimination and stigma, which increases their vulnerability to low self-esteem, depression, and a reduced quality of life. By addressing these biases and promoting a more inclusive and supportive environment, we can help improve their mental health and overall well-being13.Experts believe that without intervention, the global costs of obesity and overweight will exceed US$ 18 trillion by 2060 and US$ 3 trillion per year by 2030 7.
Contributing factors of obesogenic environment:
Obesity is the result of consuming more calories than the body uses, leading to an excess of energy and weight gain. This imbalance is influenced by various social and economic factors outside an individual’s control. Since the early 20th century, high-income countries have seen an increase in these factors, which are currently accelerating in low- and middle-income countries. These factors include economic growth, the availability of inexpensive but nutritionally deficient food, industrialization, automated transportation, and urbanization. Not everyone gains weight to the same extent when living in an environment that promotes obesity. Even in similar obesogenic environments, racial and ethnic differences, family history, genetics, and socioeconomic and cultural factors all contribute to the risk of obesity14.
Medication-Induced Obesity
Many medications now in use are related with weight fluctuations. Some medications, such as serotonin reuptake inhibitors and oral contraceptives, have conflicting evidence about their influence on body weight, whilst others are steadily allied with weight gain and tend to cause obesity, hence referred to as obesogenic drugs. This impact can result from a variety of processes, including increased appetite (steroids) or decreased metabolic rate (beta- blockers). In certain cases, the underlying illness may have contributed to weight loss; however, weight restoration following successful treatment is not viewed as a negative outcome. However, in numerous circumstances, weight gain is an unfavourable effect. These medications are used to treat chronic conditions and are consequently given for prolonged periods. Previous research found that 9% of respondents attributed their weight increase to prescription medicines15. In fact, data from the “National Health and Nutrition Examination Survey” conducted during the year 2017-2018 has revealed that around 20% of population were on medications which induce weight gain3.
Table 1: Class of medications associated with weight gain: 16, 17, 22
| Anti-cholinergics | Anticonvulsants |
| Antipsychotics | Glucocorticoids |
| Anti-retroviral agents | Beta-blockers |
| Antihistamines | Insulin |
| Hormonal contraceptives | Antipsychotics |
| Oral hypoglycaemic agents | Antidepressants |
Several prominent drugs cause weight gain as a side effect. This might lead to patients failing to follow their treatment plans, which can exacerbate their conditions. Diabetes medications such as meglitinides, sulfonylureas, thiazolidinedione, and insulin therapy; antihypertensives such as alpha-adrenergic blockers, beta-adrenergic blockers including nadolol, metoprolol, atenolol, and propranolol; Psychotropic agents like risperidone, olanzapine, clozapine, and quetiapine; Antidepressants such as doxepin, imipramine, amitriptyline, mirtazapine, paroxetine, and nortriptyline, as well as mood stabilizers like lithium, and antiepileptic medications like carbamazepine, valproate, and gabapentin18.
Medication-induced weight gain is a distressing experience for both patients and healthcare providers, and it is frequent with many routinely used medications. The increased usage of pharmaceuticals over the last decade may be contributing to global obesity trends, necessitating preventive measures. Adverse drug events, or unanticipated and unpleasant effects of medication use, are common in primary care and frequently preventable. “Food and Drug Administration’s Adverse Event Reporting System” (FAERS) has received a large number of reports on drug-induced weight gain over the last decade. These reports include instances of weight gain, abnormal weight gain, obesity, and poor weight gain. For instance, between 2003 and 2018, 137,370 reports of drug-induced weight gain were submitted to FAERS, with 68,294 classified as serious cases and 2,144 reported as fatal. Consumers made up the majority of reporters, with healthcare providers accounting for only 37.27% of the cases18.
Medications can have diverse effects on weight, leading to weight gain in some individuals and weight loss in others. In some cases, medications may initially cause weight loss but later contribute to weight gain. The effect of a medication on weight is often influenced by multiple variables. Understanding these aspects can assist healthcare providers to tailor treatment plans that minimize unwanted weight changes and promote better overall health. Furthermore, clinical studies on medication-related weight effects may underestimate the possibility for weight gain, as researchers frequently report an average weight change. With the nation’s obesity epidemic, it’s crucial for physicians to carefully consider the weight effects of prescribed medications and strive to strike a balance between the benefits of treatment and the potential for weight gain19.
Mangement of Obesity
A step-by-step integrated approach is used in the clinical management of obesity, starting with behavioural and lifestyle modification and progressing to anti-obesity medications, endobariatric procedures, and bariatric surgery20. Moreover, it is important for healthcare practitioners to recognize the potential link between certain medications and obesity. Furthermore, a number of illnesses that impact the hypothalamic-pituitary axis (HPA) may show important role in the development and progression of obesity21.
Table 2: Considerations for an obesity assessment’s components before managing it: 22, 31
| Assessment | Details |
| Physiologic | Understanding the psychological well-being of an obese patient prior to, during, and following treatment is a crucial step in the assessment process. A comprehensive physiologic assessment consists of various components, such as: Quality of life (QOL) evaluation, sleep and hunger assessment, psychological well-being and body image assessment.In the population of overweight and obese people, objective tools and subjective questionnaires have both been validated and widely used. |
| Physical activity | The frequency, duration, intensity, and kind of the patient’s activities can be incorporated by the clinical pharmacist into the treatment plan and goals with this information. |
| Dietary intake | A crucial step in the data gathering process since it gives the clinical pharmacist precise information about the patient’s dietary habits. |
| Body composition | To track progress toward treatment objectives that extend beyond weight loss, precise measurements of the body’s fat and fat-free components must be made at the cellular, molecular, and tissue levels. |
Safety concerns have enforced some promising medications intended for the treatment of obesity off the market. Over the decades, medications such as amphetamines, thyroid hormones, dinitrophenol, and drug combinations (known as rainbow pills) were granted approval but quickly withdrawn due to serious adverse reactions. Despite these setbacks, more recently approved medications for obesity control are now accessible, and can be used in conjunction with behaviour modifications23.At present, the FDA has approved five medications for the weight management: orlistat, liraglutide, naltrexone-bupropion, phentermine-topiramate, and, most recently, semaglutide. Although lorcaserin was previously used to treat obesity, it was withdrawn from the market in February 2020 due to an increased risk of cancer. 2.
Table 3: List of FDA approved anti-obesity medications (AOMs): 24
| Anti-Obesity Medications | Phentermine | Topiramate | Lorcarserin | Orlistat | Liraglutide |
| Benefits | Inexpensive, Weight loss (>3-5%) | Long-term data availability, Weight loss (>5%) | Long-term data, availability | Long-term data availability, Inexpensive | Long-term data availability |
| Concerns | Side effect profile | Expensive,Teratogen | Expensive | 2-3% weight loss | Expensive |
Concerns Associated with Use of Anti-Obesity Medications
Anti-obesity drugs (AOM) are recommended for patients with a BMI of ≥30 kg/m2 or ≥27 kg/m2 and one or more underlying health problems. However, the history of AOM is characterized by the disappointment of various medications due to substantial side effects. These consequences include cardiovascular events, suicidality, increased risk of addiction and dependence, and, most recently, cancer. Consequently, the “European Medicines Agency” (EMA) and the “Food and Drug Administration” (FDA) updated their approval standards for AOM, highlighting the significance of safety for the central-nervous system and cardiovascular system3.
One of the utmost challenging aspects of weight management is predicting patients’ responses to medications, as individuals’ weights vary greatly in response to a given treatment3. Because it involves a wide range of pathophysiological changes such as increased blood flow and gastrointestinal transit, changes in body composition, hepatomegaly, and liver and kidney dysfunction. These physiological variances cause medicine’s pharmacokinetic changes which can have a major impact on dosage, clinical tolerance, and efficacy25.Therefore, while selecting anti-obesity drugs (AOM), it is vital to focus on the safety and efficacy evidence for older patients, those with multiple conditions, and those using multiple medications. Potential drug interactions must be carefully considered22. For instance, limit the use of phentermine/topiramate and naltrexone/bupropion in patients with tachycardia or hypertension. Orlistat does not seem to have any side effects related to heart rate, but ligarglutide and semaglutide should be used carefully because they are linked to an elevated heart rate3.
Clinical Pharmacists in Weight Management Programs
As key members of the care-providers team, pharmacists play a substantial role in managing obese patients. It is critical that they take the initiative in launching weight management services, performing detailed patient interviews, developing personalized therapeutic plans, and actively monitoring treatment effectiveness and safety. Pharmacists should take a proactive approach in assessing the potential for weight gain resulting from medications and provide appropriate counseling to patients. Since obesity significantly alters body composition and can affect the effectiveness of drugs, pharmacists ought to promote personalized dosing strategies instead of depending on ineffective fixed-dosing methods.26.
Despite the availability of clinical care standards for obesity treatment and management, suboptimal outcomes continue due to a variety of variables, including a shortage of healthcare resources and qualified personnel27. Pharmacists should take an active role in addressing the needs of obese patients by providing treatment counseling, nutrition advice, and recommendations for physical activity. They should also offer support for adherence to treatment plans and conduct ongoing monitoring. It is essential for pharmacists to recognize that obesity is a chronic condition and to promote comprehensive management programs that help prevent weight regain after discontinuing anti-obesity medications26, 28.
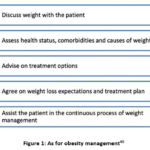 |
Figure 1: As for obesity management40Click here to view Figure |
Role in patient care
A comprehensive approach is required for effective obesity management. The first step in this is to encourage behavioural and lifestyle modifications. After that, anti-obesity drugs, endoscopic procedures, and bariatric surgery may be taken into consideration20. For the safe and effective obesity management, whether in an outpatient or inpatient setting, clinical pharmacists play an essential duty by carrying out detailed patient interviews and developing tailored treatment strategies. These strategies combine pharmacological and non-pharmacological treatments. In addition, they oversee the risk-benefit evaluations of therapeutic interventions and review the impact of medications on weight-related issues when managing the comorbid illness. In context of inpatient setting, clinical pharmacists handle medication reconciliation, address nutritional deficits, and provide medication management for obese patients, particularly those undergoing or considering bariatric surgery. They also provide thorough patient education, follow-up visits, and monitoring during the transition from inpatient to outpatient care22.
Identifying patients who are at a greater risk of medication-induced weight gain is critical in the era of personalized medicine. Pharmacogenomics can help manage obesity by optimizing the use of anti-obesity drugs and reducing undesirable weight outcomes20. Clinical pharmacists are in charge of many facets of medication-related patient care, including medication selection, dosage adjustments, therapy discontinuations when needed, drug interaction detection, patient adherence assessment, medication access facilitation, and patient education. Clinical pharmacists might suggest angiotensin-II receptor blockers (ARBs), calcium-channel blockers, and angiotensin converting enzyme inhibitors (ACE-inhibitors)-as treatment options for reducing high blood pressure, because they have not been observed to cause weight gain22.
Role in Bariatric Surgery
Bariatric procedures can result in a variety of complications, both immediately after the procedure and afterward. Early complications can include major concerns like leaking, bleeding, infections, blood clots, pulmonary issues, and even deaths. Later consequences can include stenosis, acid reflux, ulcers, nutritional deficiencies, and changes in bone density. Patients may also experience frequent vomiting, an increased dehydration risk, and abnormal laboratory test findings such as variations in blood sugar, International Normalized Ratio (INR), and drug levels in the bloodstream.
Furthermore, bariatric surgery causes major structural changes that can affect medication availability. These alterations result from lower stomach acidity, decreased stomach volume, partial intestinal bypass, and decreased surface area for the drug absorption. Furthermore, several transporters and enzymes involved in drug distribution and metabolism may be affected. Patients may also need to modify their long-term prescription regimens as a result of improvements in illnesses including diabetes, hypertension, and high cholesterol. It is important to remember that some pharmaceuticals, such as lithium and anti-epileptic medications, may require careful monitoring and dosage modifications. Managing medication in patients following bariatric surgery poses a formidable challenge29.
Upon bariatric surgery admission to the hospital, a clinical pharmacist is in charge of obtaining the patient’s medication history and evaluating the suitability and safety of each prescription. The patient’s at-home medication schedule, including any prescription and OTC medications, must be documented as soon as they are admitted. At every step of the patient’s hospital stay, the pharmacist should carefully document the patient’s medication history, adherence, and allergies. Then, they should compare this information to updated medication lists to find any medication-related issues. To lower prescription errors and avoid side effects, it’s critical to resolve discrepancies. To determine the appropriate dosages for pain management, venous thromboembolism prophylaxis, and infection prevention, the clinical pharmacist can determine the patient’s weight upon arrival and validate any prescriptions before surgery by taking an accurate medical history.
As the key medication expert, a clinical pharmacist actively participates in the formulation of policies pertaining to medications required prior to, during, and following bariatric surgical procedures. In order to ensure evidence-based medication practices and precise weight-based calculations, clinical pharmacists also provide valuable input into the medication orders set before and after surgical interventions. To ensure that patients receiving surgical intervention for obesity treatment are managed effectively, the clinical pharmacist is dedicated to reviewing policies and procedures in light of new research and offering educational support to the bariatric surgeon and other medical professionals22.
Impact of clinical pharmacist interventions in combating obesity and weight gain:
In comparison to conventional weight management techniques, several studies that have examined models for pharmacist contribution in lifestyle changes and medication related- weight-loss management and found that clinical pharmacists’ involvement in interdisciplinary care through pharmacotherapy and medication-related services significantly improves weight loss outcomes30.
Table 4: List of evidence showing effective pharmacist-led weight management interventions: 32-36
| Author | Intervention | Nature of intervention program | Impact |
| Morrison D ,Scotland32 | “Pharmacy-based weight management programs”32 | “Counterweight Program- Keep Well Project.” | At the end of a year, 42% of enrolled patients, who attended all the meeting experienced weight loss of at least 5%. |
| Lloyd KB, USA33 | “The Healthy Habits weight-loss program”33 | A standalone pharmaceutical care center was set up. Wherein residents, faculty, and students of pharmacy continue to support patients. | More than 13% of the 289 enrolled patients reduced more than 10% of their body weight. Relative to baseline, 76 patients had a lower risk status, and 83 patients were able to lower their BMI category. |
| Milton-Brown, USA34 | “Clinical pharmacist-led weight loss program using meal replacement stratergy.34 | A clinical pharmacist oversees a six-month intervention that includes pre- and post-study surveys. | At the end of the third month, 15 patients had lost an average of 10.2 pounds, and at the end of the sixth month, 3 patients had lost an average of 14.17 pounds. |
| Murphy, USA35 | “Free pharmacist-led Cardiovascular risk reduction clinic”35 | Retrospective chart review of patients | Average drop in BMI of 0.42 kg/m2. Six patients were able to transition from the obese to the overweight category, and six from the overweight to the normal weight category. |
| Haverkamp K, USA36 | “Pharmacist-run weight loss medication management service”36 | Patients who participated in the MOVE! Weightloss-program were consulted with the clinical pharmacist for further ongoing weight management, and follow-up via telehealth visits. | Approximately 17% of the patients reduced 5% of their body weight. |
Role of Multidisciplinary Healthcare Professionals and Alternative Therapies in Weight Managament Programs
Maintaining a healthy weight necessitates continuous dietary changes and exercise, as no single diet or exercise regimen is universally effective. In order to promote metabolism, effective weight management usually entails losing at least 5% of body weight. Overweight individuals frequently face challenges such as impaired metabolic flexibility, which makes it difficult to switch between energy sources and increases the risk of chronic health problems. Weight loss programs frequently focus on fatty acid usage, which complicates the process for those with metabolic inflexibility. Unhealthy weight gain often arises from a variety of factors that can disrupt metabolism, which may vary from person to person. It’s essential for practitioners to recognize and assess these underlying causes in order to develop a customized weight loss program that effectively addresses individual needs 37.
Additionally, weight regain is another common challenge; emphasising the importance of a personalized approach focused on metabolic influences to help maintain lost weight. This goal can be achieved through a collaborative effort involving a multidisciplinary team of professionals, including physicians, nutritionists, exercise physiologists, and trainers. For instance, Nutritionists play a key role in this collaboration by designing dietary plans that take into account the patient’s metabolic profile and any existing comorbidities. Laboratory technologists play an important role in diagnosing metabolic issues and enabling a more targeted approach to weight management. Once comorbidities are identified, nutritionists can create a calorie-restricted plan that is specific to the patient’s needs. The evaluation of key indicators that may indicate metabolic disturbances, which are frequently associated with weight regain, is critical in developing an effective therapeutic regimen. As a result, diagnostic laboratory specialists offer invaluable assistance in guiding treatment decisions 37.
Herbal medicine (HM) is one of the most common complementary and integrative medicine (CIM) therapies for weight loss around the world 38. While herbal therapy can aid in weight reduction, they should be paired with regular exercise and a balanced diet for optimal results. It is critical to notify the physician about any herbal remedies you intend to use to avoid potential interactions with prescription medications or underlying health conditions. While herbal weight loss treatments may provide a more natural, long-term approach, they are risky if not used responsibly; misuse can result in serious health problems or, in severe cases, be fatal38. An interprofessional team can identify underlying causes, develop effective treatment strategies, and create comprehensive plans, promoting a holistic approach to weight management for optimal outcomes. Collaboration in decision-making and patient counseling is critical for long-term weight management and the prevention of future challenges. Prioritizing integrated care management alongside evidence-based practices allows the care team to provide effective and patient-centered interventions37.
Conclusion
Clinical pharmacists play a vital role in managing weight gain and obesity by leveraging their expertise in pharmacotherapy, medication management, and patient education. They contribute significantly to personalized treatment plans, ensuring the safe and effective use of weight-loss medications while promoting lifestyle changes. As key members of interdisciplinary care teams, pharmacists help enhance the quality of obesity management by reducing medication-related risks and optimizing therapeutic outcomes. Integrating them into obesity care is essential for achieving better long-term health results and providing comprehensive patient support.
Acknowledgement
All authors sincerely acknowledge JSS Academy of Higher Education and Research, Mysuru, India for continuous support and for providing resources.
Funding Sources
The author(s) received no financial support for the research, authorship, and/or publication of this article
Conflict of Interest
The author(s) do not have any conflict of interest
Data Availability
This statement does not apply to this article.
Ethics Statement
This research did not involve human participants, animal subjects, or any material that requires ethical approval.
Informed Consent Statement
This study did not involve human participants, and therefore, informed consent was not required.
Clinical Trial Registration
This research does not involve any clinical trials
Authors Contributions
Each author mentioned has significantly and directly contributed intellectually to the research work carried out and has given their approval for its publication.
- Ravindra Pukharaj Choudhary: Conceptualization, Visualization, Writing – Original Draft.
- Adinarayana Andy: Conceptualization, Data Collection, Writing – Review & Editing.
- Divya Andy: Data Collection, Visualization, Writing – Review & Editing.
- Srikanth Malavalli Siddalingegowda: Reviewing & Editing, Resources, Supervision.
References
- Tiwari A, Balasundaram P. Public health considerations regarding obesity. In: StatPearls Publishing; 2024.
- Francis BR, Challen L. The impact of a clinical pharmacist in an interdisciplinary weight loss service: A follow-up study. Inov Pharm. 2021;12(4):13.
CrossRef - Chakhtoura M, Haber R, Ghezzawi M, Rhayem C, Tcheroyan R, Mantzoros CS. Pharmacotherapy of obesity: an update on the available medications and drugs under investigation. 2023; 58(101882):101882.
CrossRef - Karami DD, Iram M, Prasad S. Role of clinical pharmacist in educating obese and over weight patients for better health related outcomes: Pharmaceutical science-clinical pharmacy. Int J Life Sci Pharma Res. 2019;9(4):1-6.
CrossRef - Mallhi TH, Ijaz I, Khan YH, Javed A, Saleem U, Aftab RA, Alzarea AI, Alotaibi NH, Alanazi AS, Salman M, Butt MH. Relationship between the use of drugs and changes in body weight among patients: A systematic review and meta-analysis. Trop J Pharm Res. 2022;21(4):899-908.
CrossRef - Masood B, Moorthy M. Causes of obesity: a review. Clin Med. 2023;23(4):284-291.
CrossRef - One in eight people are now living with obesity. Saudi Med J. 2024;45(4):448-449. https://www.who.int/news/item/01-03-2024-one-in-eight-people-are-now-living-with-obesity , Accessed October 2, 2024.
- World Health Organization. Obesity and overweight. World Health Organization. Published March 1, 2024. https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight
- Barras M, Legg A. Drug dosing in obese adults. Aust Prescr. 2017;40(5):189-193.
CrossRef - Broughton M, Lymn JS, Redsell SA. Barriers and enablers to weight management programmes for working men: A qualitative study. Health Soc Care Community. 2023;2023:1-9.
CrossRef - AlMukdad S, Zaghloul N, Awaisu A, Mahfoud ZR, Kheir N, El Hajj MS. Exploring the role of community pharmacists in obesity and weight management in Qatar: A mixed-methods study. Risk Manag Healthc Policy. 2021;14:2771-2787.
CrossRef - O’Neal KS. Chapter 14. Obesity—weight management services. In: McGraw Hill Medical. Available at: https://accesspharmacy.mhmedical.com/content.aspx?bookid=684§ionid=45145849
- Winters A, Johnson HE. The role of pharmacy education in mitigating weight bias. Am J Pharm Educ. 2022;86(9):ajpe8844.
CrossRef - Hruby A, Hu FB. The epidemiology of obesity: A big picture. 2015;33(7):673-689.
CrossRef - Leslie WS, Hankey CR, Lean MEJ. Weight gain as an adverse effect of some commonly prescribed drugs: a systematic review. 2007;100(7):395-404.
CrossRef - Holman RR, Farmer AJ, Davies MJ, Levy JC, Darbyshire JL, Keenan JF, Paul SK. Three-year efficacy of complex insulin regimens in type 2 diabetes. N Engl J Med. 2009;361(18):1736-1747.
CrossRef - Nudel J, Sanchez VM. Surgical management of obesity. Metabolism. 2019;92:206-216.
CrossRef - Ahmed NJ, Alshehri AM, Almalki ZS, Alahmari A. Drug-induced weight gain in the last 10 years: a descriptive study. 2022;77(10):299-301.
- Dabom F, Shukla AP, Aronne LJ. Drug-induced weight gain: Mdedge.com. https://cdn.mdedge.com/files/ s3fs-public/JFP06511780.PDF .Accessed October 2, 2024.
- Singh S, Ricardo-Silgado ML, Bielinski SJ, Acosta A. Pharmacogenomics of medication‐induced weight gain and antiobesity medications. Obesity (Silver Spring). 2021;29(2):265-273.
CrossRef - Singh A, Hardin BI, Singh D, Keyes D. Epidemiologic and etiologic considerations of obesity. In: Treasure Island (FL): StatPearls Publishing; 2024.
- Clements JN, Albanese NP, D’Souza JJ, Misher A, Reece S, Trujillo J, Whitley HP. Clinical review and role of clinical pharmacists in obesity management: An opinion of the endocrine and metabolism practice and research network of the American College of Clinical Pharmacy. J Am Coll Clin Pharm. 2021;4(11):1469-1484.
CrossRef - Müller TD, Blüher M, Tschöp MH, DiMarchi RD. Anti-obesity drug discovery: advances and challenges. Nat Rev Drug Discov. 2022;21(3):201-223.
CrossRef - Apovian CM, Aronne LJ, Bessesen DH, McDonnell ME, Murad MH, Pagotto U, Ryan DH, Still CD. Pharmacological management of obesity: an endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2015;100(2):342-362.
CrossRef - Gouju J, Legeay S. Pharmacokinetics of obese adults: Not only an increase in weight. Biomed Pharmacother. 2023;166(115281):115281.
CrossRef - Jovanović M, Kovačević M, Ćulafić M. Role of pharmacists in the management of patients with obesity. Arh Farm (Belgr). 2024;74(3):483-508.
CrossRef - Leach J, Powis R, Baur J, Caterson LA, Dietz ID, Logue W. Clinical care for obesity: A preliminary survey of sixty‐eight countries. Clinical Obesity. 2020;10(2).
CrossRef - Tchang BG, Aras M, Kumar RB, Aronne LJ. Pharmacologic treatment of overweight and obesity in adults. In: South Dartmouth (MA): MDText.com, Inc.; 2000.
- Azran C, Dahan AE, Shimoni O, Dicker D, Hammerman A, Dahan A. Can consultation by a clinical pharmacist prevent morbidity and mortality in patients undergoing bariatric surgery? Journal of Clinical Medicine. 2024;13(2):310.
CrossRef - Jordan M, Harmon J. Pharmacist interventions for obesity: improving treatment adherence and patient outcomes. Integr Pharm Res Pract. 2015:79.
CrossRef - Beechy L, Galpern J, Petrone A, Das SK. Assessment tools in obesity- Psychological measures, diet, activity, and body composition. Physiol Behav. 2012;107(1):154-171.
CrossRef - Morrison D, McLoone P, Brosnahan N, McCombie L, Smith A, Gordon J. A community pharmacy weight management programme: an evaluation of effectiveness. BMC Public Health. 2013;13(1):282
CrossRef - Lloyd KB, Thrower MR, Walters NB, Krueger KP, Stamm PL, Evans RL. Obesity: Implementation of a weight management pharmaceutical care service. Ann Pharmacother. 2007;41(2):185-192.
CrossRef - Milton-Brown J, Barnes AS, Ndefo UA, Erowele GI. Pharmacist-managed weight-loss program using meal-replacement product. Am J Health Syst Pharm. 2012;69(17):1456- 1458.
CrossRef - Murphy PZ, Sands C, Ford F. Effectiveness of a pharmacist-led Cardiovascular Risk Reduction Clinic in rural Perry County, Alabama. Int J Chronic Dis. 2016;2016:1-6.
CrossRef - Haverkamp K, Newberry P, Baker J. Impact of a pharmacist-run weight loss medication management service. J Am Pharm Assoc (2003). 2022;62(3):883-888.
CrossRef - Farhana A, Rehman A. Metabolic consequences of weight reduction. In: StatPearls Publishing; 2024.
- Yim MH, Lee B. Factors affecting the use of herbal medicines for weight loss in overweight and obese adolescents. Front Pediatr. 2023;11:1166786.
CrossRef - Nannar AR, Raosaheb S. S, Salunkhe K. Review on weight loss management by herbal therapy. BOHR Journal of Pharmaceutical Studies. 2023;1(1):28-34.
CrossRef - Welzel FD, Stein J, Pabst A, Luppa M, Kersting A, Blüher M, Luck-Sikorski C, König HH, Riedel-Heller SG. Five A’s counseling in weight management of obese patients in primary care: a cluster-randomized controlled trial (INTERACT). BMC Fam Pract. 2018;19(1):97.
CrossRef







