Manuscript accepted on :21-02-2025
Published online on: 28-02-2025
Plagiarism Check: Yes
Reviewed by: Dr. Elina Margarida Ribeiro Marinho and Dr. Nurul Diyana Sanuddin
Second Review by: Dr. Salma Rattani and Dr. Adinarayana Andy
Final Approval by: Dr. Prabhishek Singh
Susheela Vishnoi1 , Saneh Lata Yadav2
, Saneh Lata Yadav2 , Ashok Kumar Saini1
, Ashok Kumar Saini1 and Prashant Vats1*
and Prashant Vats1*
1Department of CSE, Manipal University Jaipur, Jaipur, Rajasthan, India
2Department of CSE, K. R. Mangalam University, Gurugram, Haryana, India
Corresponding Author E-mail: prashant.vats@jaipur.manipal.edu
DOI : https://dx.doi.org/10.13005/bpj/3091
Abstract
This paper investigates the transformative impacts of e-governance strategies on the Internet of Medical Things (IOMT) and IOMT-based medical system administration in the context of the COVID-19 pandemic within the Indian Subcontinent, leveraging applications of Artificial Intelligence and Machine Learning (AIML). As the pandemic continues to strain healthcare systems worldwide, effective utilization of digital technologies becomes paramount in ensuring efficient healthcare delivery. E-governance initiatives play a crucial role in facilitating the integration of IOMT devices and AIML algorithms into medical systems, thereby enhancing healthcare accessibility, quality, and responsiveness during crises. This study examines the implementation and outcomes of e-governance measures in leveraging IOMT technologies and AIML applications to address pandemic-related challenges in the Indian Subcontinent's healthcare sector. Through a comprehensive analysis, it elucidates the synergistic relationship between e-governance strategies, IOMT adoption, and AIML utilization, highlighting their collective contributions to strengthening medical system administration and mitigating the impact of the pandemic on public health. E-Governance began by offering citizens e-services that help them deal with the challenges of technological advances, and since then has extended to include consumer networking, demographic forecasting, financial management, and e-healthcare operations. E-governance is defined as the provision of social programs via the use of information systems, which indicates the amount, and sharing of information, the implementation of innumerable electronic systems, and subtypes between both the government and its constituents, the business and government environments, and government and state organizations. Using SPSS tools to collect data from 433 employees in India's tourist industry, the links mentioned above were verified. The data reveal that the information governance approach does have a significant impact on health catastrophes, particularly joblessness negatively forecasting emergencies. As per the data, parental involvement reduced the link between E-Governance programs and rising unemployment. The study's outcomes backed up this theory, indicating that employees with strong family support are less likely to be unemployed than those with a lower degree of interpersonal assistance.
Keywords
Artificial Intelligence; Digital Transformation; E-Governance; Good Health; Healthcare Administration; Healthcare Technology; Indian Subcontinent; Internet of Medical Things (IoMT); Machine Learning, Pandemic
Download this article as:| Copy the following to cite this article: Vishnoi S, Yadav S. L, Saini A. K, Vats P. Transforming Healthcare Delivery: Assessing the Role of E-Governance Strategies in IOMT and AIML-Based Medical System Administration during the Pandemic in the Indian Subcontinent. Biomed Pharmacol J 2025;18(March Spl Edition). |
| Copy the following to cite this URL: Vishnoi S, Yadav S. L, Saini A. K, Vats P. Transforming Healthcare Delivery: Assessing the Role of E-Governance Strategies in IOMT and AIML-Based Medical System Administration during the Pandemic in the Indian Subcontinent. Biomed Pharmacol J 2025;18(March Spl Edition). Available from: https://bit.ly/3R3NiAt |
Introduction
The COVID-19 pandemic has underscored the critical need for innovative approaches to healthcare delivery, particularly in regions like the Indian Subcontinent, where population density and resource constraints pose significant challenges. In response to these challenges, governments and healthcare authorities have increasingly turned to digital solutions, including e-governance strategies, the Internet of Medical Things (IOMT), and applications of Artificial Intelligence and Machine Learning (AIML), to enhance medical system administration. E-governance initiatives encompass a range of digital technologies and practices aimed at improving government efficiency, transparency, and service delivery. In the context of healthcare, e-governance strategies facilitate the integration of IOMT devices—such as wearable sensors, remote monitoring tools, and medical imaging systems—into existing medical infrastructure. These devices generate vast amounts of data that can be analyzed and leveraged using AIML algorithms to optimize healthcare processes, personalize patient care, and support decision-making by healthcare professionals.
In the Indian Subcontinent, where the COVID-19 pandemic has placed immense strain on healthcare systems, the role of e-governance strategies in enabling the adoption of IOMT and AIML technologies has become increasingly prominent. This paper seeks to examine the impacts of e-governance measures on IOMT and IOMT-based medical system administration during the pandemic in the Indian Subcontinent, with a specific focus on the applications of AIML. By exploring the implementation and outcomes of e-governance strategies in the healthcare sector, this study aims to shed light on how digital technologies are reshaping healthcare delivery in the region. Through a comprehensive analysis of relevant literature, case studies, and empirical evidence, this paper will elucidate the synergistic relationship between e-governance strategies, IOMT adoption, and AIML utilization, highlighting their collective contributions to strengthening medical system administration and mitigating the impact of the pandemic on public health in the Indian Subcontinent. The COVID-19 epidemic seems to have had a major impact on the service economy, particularly tourism. Either intrinsically or extrinsically, the tourism sector is a vital driver for job generation and economic growth across the globe. Governments’ aggressive measures to curb the disease’s development and effects have created barriers for workers in the industry. Employment restrictions, crowded public prohibitions, and traveling limitations are instances of such measures. Since such restrictions were meant to inhibit the spread of infectious infection, spending time absent from work due to them raised the risk of loss of employment and lower income. According to a study of the pertinent literature,1, 2 studies have widely confirmed the negative effects of COVID-19 and E-governance measures like shutdown on medical concerns. According to earlier studies,3 among some of the e-attempts the administration is doing to reduce fear of the illness are awareness of preventative measures, awareness about the virus, and closings. However, E-governance neglected to consider emotional factors that influence people’s psychological and emotional well-being.4 From this standpoint, further investigation is necessary to evaluate the relationship between electronic government policies and social and economic issues, especially among tourism sector employees. Furthermore, there’s been a minimal study on how well the pandemic has impacted individuals’ healthcare problems. Carry-out employees,5 professional healthcare workers,6, 7 and poor migrant employees3 ,6 have all been the subject of earlier research. These studies were done from outside the tourist sector, namely from outside India, where the tourist industry is a major driver of economic development. COVID-19 is also a worldwide problem that impacts individuals, institutions, businesses, and nations across the globe. Previous research suggests that the threat of losing one’s employment is by far the most serious impact of E-Governance practices like shutdown.8 Put simply, the policies have caused people in the business to feel increasingly insecure about their jobs and also have increased their sense of rising unemployment. “A personal anxiety about just the sustainability of the employment” is what work anxiety is defined as. This anxiety has been connected to a detrimental impact on companies’ productivity9 as well as various healthcare issues.10 Offering social assistance to workers is a significant approach for a company to have an influence. This emphasizes the possible significance of social assistance in reducing poor outcomes both outside and inside employment.11 The company must give psychosocial assistance to employees who are facing the effects of electronic government policies like shutdown. As a result, research into treatments that might mitigate the effects of E-Governance policies on employee health insurance emergencies is required. Lengthy strategic vision and organizational innovation, disease health and prevention improvement, excellence, incorporation of environmental concerns, organizational responsibility, and personal accountability are indeed the five fundamental elements of sustainable health service as shown in Figure 1.
 |
Figure 1: To show the fundamental elements of a sustainable health serviceClick here to view Figure |
Hypothesis Formulation and Analytical Framework
Studies show that as occupational uncertainty rises, job losses become even more frequent and individuals who currently hold work worry even more about their futures.12 Job uncertainty is a stressful environment that was associated throughout investigations with psychological distress.13, 14 Due to the frequency of the COVID-19 epidemic, only a few research have looked at the psychiatric effects of work instability.15 Nevertheless, some data suggest that employment instability induced by the COVID-19 epidemic has a major mental health impact. Prior studies showed the harmful mental health effects of job instability before the current epidemic, which supports this finding.16, 17 According to a recent study on the COVID-19 pandemic, employment uncertainty is linked to healthcare issues.18
The “sensation of enjoying life and/or genuine and important in someone’s life” is classified as a healthcare problem.19 The procedural and hedonistic elements of medical crises are included in this description; the former is associated with the attainment of an individual’s ability and a feeling of belonging, while the latter is focused on the absence of risk impact and the prevalence of detrimental effects. Occupational medical problems have been studied in terms of job attributes and workplace stress.20, 21 As a result, further research is necessary during the COVID-19 epidemic. The “perception of being cared for, respected, and a member of a mutually interdependent social media network” is defined as “the feeling of being cared for, valued, and a member of a mutually reinforcing social media platform.22” The positive effects on personal health have been demonstrated in research.22 Numerous studies have found that social influence plays a critical role in minimizing occupational discomfort.23,24 According to Household,25 health support has three different consequences on anxiety and its outcomes. A supportive social network could just have a significant impact on growth since people who have received additional aid seem to be more likely to be satisfied with their occupations and to have fewer depressive symptoms. Second, it could have a significant or instantaneous impact on perceived anxiety, so that the level of strain perceived is lowered whenever a supportive signal is present. Finally, the ultimate effect is postponement. The key concept is that psychological advantages could change the relationship between socioeconomic status and its repercussions. The latter might be in line with the primary research purpose, which was to see whether the external effects of E-Governance initiatives on healthcare crises are influenced by social cooperation.
Medical Emergencies and E-Governance Policy
Medical emergencies have been claimed to be exacerbated by E-Governance initiatives which include prohibitions.26, 27, 28 While Electronic government measures like limits are meant to slow the spread of illness, they have quickly altered the structure of human existence, prohibiting, or outright prohibiting any kind of public connection and forcing individuals to adjust to whole everyday habits. From this perspective, Rudolph et al29 brought out that, whereas these E-Governance techniques are successful in preventing viral propagation, they constitute psychological stresses. Some nations implemented limited shutdowns, whereas others implemented complete shutdowns and inoculations. Many portions of their populace are subjected to different degrees of restrictions as a result of such efforts. Previous research has revealed that such policies have just a negative impact on healthcare emergencies and physical health wellbeing.30 This research was carried out in several different directions and outside the tourism business. As a result, the link between E-Governance policies and healthcare problems in the tourist sector, notably in India, is still to be investigated. We propose the following hypothesis based on the aforementioned facts and literature available:
H1: E-Governance policies are strongly linked to medical emergencies.
Rising Unemployment and E-Governance Strategy.
The Adaptive National Healthcare paradigm has attracted the interest of researchers from all over the globe. Adequate treatment, reduced healthcare costs, and significantly lesser resource usage can be achieved through extensive healthcare information reprocessing and also the incorporation of patients’ opinions into therapeutic paradigms.31,32 The COVID-19 regulations’ potential consequences and related effects are unprecedented in recent decades.33 Individuals are likewise thought to be poor prognosticators about their potential outcomes.34,35 According to Rosenblatt et al.36, employment insecurity is the fear of having one’s employment when employed by a company where this possibility exists. As a result, the link between E-Governance policies and employment instability may be especially crucial during the COVID-19 epidemic. Furthermore, although governments provide monetary support to firms, the adoption of a countrywide shutdown affects corporate operations, causing workers to fear for their employment security. We propose the following hypothesis based on the aforementioned logic:
H2: E-Governance policies are negatively linked to employment uncertainty.
Mass unemployment and Health-Care Shortages.
Work uncertainty has been connected to both mental and physical health issues.37-40 These include psychological tiredness, melancholy emotions, anxiousness, somatic complaints, psychosocial problems, and annoyance. Furthermore, Khan et al.4 said that work uncertainty is one of the major causes that contribute to worker dissatisfaction, which has an impact on their healthcare problems. Likewise, Llosa et al.41 found that job uncertainty had a considerable impact on the employees’ psychological health. Employment instability may be a significant concern in the COVID-19 epidemic. Since companies tend to experience monetary damage as a result of the epidemic, employment instability among workers is expected to increase. As a result, further study on the impact of uncertainty on medical emergencies, particularly in the tourism business, is needed in the epidemic setting, taking into consideration the dynamic structure of the crisis. We recommend the following based on the information mentioned above:
H3: Uncertainty about one’s job has a bad impact on healthcare emergencies.
Rising Unemployment as a Moderator in the Relationship Factor
Rising Unemployment as a Moderator in the Relationship Factor has been stated under “A projected danger to the continuation and sustainability of occupation as it is now understood,” by Meyer et al.42 in a detailed study on job uncertainty. Additionally, many researchers have observed that the prospect of losing one’s job can increase mental health problems when in an epidemic43,44, and lawmakers ought to be aware that E-Governance activities when in an epidemic can now have important macroeconomic consequences.14,45 Zhang et al.8 discovered that one-fourth into the epidemic, emergencies amongst those who were exceedingly engaged previous to the outbreak seemed especially vulnerable to the disease’s incidence in their immediate vicinity among some of the Chinese population. Therefore, with respect, cross-national research of current and predicted unemployment rates in 28 European nations indicated that employment instability is linked to related to the characteristics of health and wellbeing.46 In contrast, Llosa et al.41 discovered that people with poor living standards, and other physiological and mental challenges, are more likely to perceive future economic security as in threat. Employee empowerment has been found to have a series of adverse implications in previous research. Psychiatric issues, an absence of truthfulness, and extreme occupational anxiousness are only a few drawbacks of rising unemployment, according to Kalleberg.47 We assert that perhaps the relationship between e-government projects and economic and social problems in this specific instance was moderated by job uncertainty. As a consequence, we suggest that you do the aforementioned:
H4: The association between E-Governance policies and clinical problems is mediated by economic uncertainty.
The Peer Support Mediational Influence
Consumers’ views of the wider availability of help or contentment with both the grants received are measured by support networks.48 The epidemic is a worldwide threat. Patients’ wellness is afflicted by extremely contagious infections like COVID-19, which impact people’s healthcare needs.8 People with insufficient social interaction are much more inclined to perceive psychological trauma during the epidemic, according to research work.42 The researchers determined that activities aimed at lessening the pandemic’s psychological negative impacts on the capitalist poor should have been explored and that assistance (at home and work) moderated the relationship between pandemic duration and emotional health complications amongst populations. Due to the project’s restricted ability to handle harmful materials, the current socialized healthcare infrastructure currently appears insufficient to handle the surge in the number of COVID-19 occurrences. Adams and Stuart49 aimed to promote discussion on changing the Canadian national healthcare system by adapting Maslow’s hierarchy of needs to the healthcare ecosystem (see Figure 2). The COVID-19 pandemic has revealed weaknesses in patient care facilities as well as the healthcare industry’s failure to provide essential health treatment during lengthy emergencies. The Indonesian government needs to enhance the nation’s economic medical system. To tackle those growing problems, several solutions have been developed. Notwithstanding this, the challenges of growing healthcare infrastructure highlight the reality that certain initiatives may be just one part of the epidemic management scenario. To respond effectively to an epidemic, administrations must commit to expanding medical infrastructure whilst simultaneously smoothing the curves (family and community assistance) in stress reduction as well as its consequences. As a result, we make the following recommendations:
H5: The association between the E-Governance strategy and medicine emergencies is moderated by welfare protection, with more support networks reducing the detrimental impact of the E-Governance strategy on medical emergencies.
E-governance strategies, coupled with the adoption of the Internet of Medical Things (IOMT)
E-governance strategies, coupled with the adoption of Internet of Medical Things (IOMT) technologies and the utilization of Artificial Intelligence and Machine Learning (AIML) applications, have significantly improved medical system administration during the COVID-19 pandemic in the Indian Subcontinent.
Analytical Framework
E-Governance Strategies: This component examines the various e-governance initiatives implemented by governments and healthcare authorities in the Indian Subcontinent to enhance healthcare delivery during the pandemic. It explores the effectiveness of these strategies in facilitating the integration of digital technologies, streamlining administrative processes, and improving access to healthcare services.
 |
Figure 2: To show Maslow’s hierarchy of needs in the healthcare ecosystem.Click here to view Figure |
Adoption of IOMT Technologies: This aspect focuses on the uptake of Internet of Medical Things (IOMT) devices and platforms within the healthcare sector. It evaluates the extent to which healthcare facilities in the Indian Subcontinent have integrated IOMT technologies into their infrastructure, the types of devices and applications deployed, and the impact of IOMT on medical system administration and patient care during the pandemic.
Utilization of AIML Applications: This component assesses the use of Artificial Intelligence and Machine Learning (AIML) algorithms in healthcare settings, particularly in the context of the Covid-19 pandemic. It examines how AIML applications have been employed to analyze medical data, support clinical decision-making, optimize resource allocation, and enhance patient outcomes in the Indian Subcontinent.
Impact on Medical System Administration: This dimension analyzes the overall impact of e-governance strategies, IOMT adoption, and AIML utilization on medical system administration during the pandemic. It considers factors such as efficiency gains, cost-effectiveness, improvements in healthcare access and quality, and the ability to respond effectively to public health emergencies.
Through this analytical framework, we aim to test the hypothesis that e-governance strategies, combined with the adoption of IOMT technologies and the utilization of AIML applications, have contributed significantly to the enhancement of medical system administration during the Covid-19 pandemic in the Indian Subcontinent. We will gather empirical evidence from relevant literature, case studies, and empirical studies to support our analysis and conclusions.
Rationale behind the proposed work
The rationale behind the proposed work lies in the urgent need to address the challenges faced by the healthcare system in the Indian Subcontinent during the Covid-19 pandemic through the strategic implementation of digital technologies, particularly e-governance strategies, Internet of Medical Things (IOMT), and Artificial Intelligence/Machine Learning (AIML) applications. Several key factors underscore the importance and relevance of this research:
Healthcare System Strain
The Indian Subcontinent, with its dense population and limited healthcare resources, has faced significant challenges in managing the COVID-19 pandemic. The strain on healthcare infrastructure, shortage of medical personnel, and logistical difficulties necessitate innovative solutions to enhance the efficiency and effectiveness of medical system administration.
Potential of Digital Technologies
E-governance strategies offer a framework for leveraging digital technologies to improve governance and service delivery in various sectors, including healthcare. The integration of IOMT devices and AIML algorithms presents promising opportunities to enhance healthcare accessibility, quality, and responsiveness, particularly during public health crises.
Data-Driven Decision-Making
The proliferation of digital health technologies generates vast amounts of data that can be analyzed to inform decision-making processes in healthcare administration. AIML applications enable data-driven insights, predictive analytics, and personalized healthcare interventions, thereby improving resource allocation and patient outcomes.
Policy Relevance
Research on the impacts of e-governance strategies, IOMT adoption, and AIML utilization in the healthcare sector is highly relevant for policymakers, healthcare administrators, and other stakeholders. Evidence-based findings can inform the development of policies, guidelines, and investment strategies to strengthen healthcare systems and build resilience against future pandemics or health emergencies.
Knowledge Gap Address
Despite growing interest in digital health solutions, there remains a knowledge gap regarding their implementation, effectiveness, and best practices, particularly in the context of the Indian Subcontinent. This research seeks to address this gap by providing empirical evidence, insights, and recommendations based on rigorous analysis and synthesis of existing literature and data.
Capacity Building and Collaboration
By promoting research and dialogue on digital health innovation, this work contributes to capacity building among healthcare professionals, technology developers, policymakers, and researchers in the Indian Subcontinent. It also fosters collaboration between various stakeholders to drive innovation, knowledge sharing, and collective action in improving healthcare delivery.
In summary, the proposed research is driven by the imperative to harness the transformative potential of digital technologies to address the pressing challenges facing the healthcare system in the Indian Subcontinent amidst the COVID-19 pandemic. By examining the impacts of e-governance strategies, IOMT adoption, and AIML utilization, this work aims to provide actionable insights and recommendations to strengthen medical system administration and enhance public health outcomes in the region.
Materials and Methods
The subjects in this research included comprehensive workers of 50 distinct tourism attractions in India’s various regions. Since people commute from all around the country and worldwide for religious events, such tourist locations are vital to the country’s economy. Mata Vaishnava’s Shrine, Haridwar and Rishikesh Shrine, Mumbai’s location, Delhi’s Akshardham temple, Cluster areas of Dharavi slum in Mumbai, and others were among the epidemic’s fragile sites examined. To analyze our research variables, we sent out a conscience questionnaire survey to the respondents. Human capital (HR) directors of these key destinations were approached by data collection procedures to obtain appropriate approval. Workers were motivated to participate in this survey when designers explained the goal to participants and also guaranteed individuals that their identity and anonymity would be respected. An intentional purposeful sampling was included in this study to ensure willingness to participate, and also no monetary rewards as offered to the respondents. Online Surveys were used to send the survey. Although some respondents submitted the answered questionnaires right once, others waited up to several hours to do so. On February 12, 2020, and August 2, 2022, data was collected. A maximum of 655 questionnaires have been distributed, with 433 legitimate replies being found. There have been several 222 incorrect replies deleted. After removing invalid replies, we have several respondents of 66.92 percent. Descriptive statistics may be seen in Table 1. There are 293 women (67.12 percent), 144 men (34.76 percent), and 121 Transgenders (12.56) percent in the final study. The overwhelming (96%) of the respondents were above the age of 27, and the overwhelming (94%) had to have at least a bachelor’s degree. 456 (78.87 percent) of them will have at least seven years of experience. The results are shown in Fig. 3.
Table 1: Demographic Information on the surveyed participants’ ethnicities.
| Statistics on the population (n=433) | Periodicity | Proportion (in %) |
| Sexual identity | ||
| Female | 293 | 67.12 |
| Male | 144 | 34.76 |
| Transgenders | 121 | 12.56 |
| Age longevity (in years) | ||
| 18-26 | 11 | 2.78 |
| 27-36 | 113 | 26.89 |
| 37-46 | 244 | 58.69 |
| 47-56 | 58 | 14.56 |
| 56 and above | 13 | 2.56 |
| Qualification | ||
| Matriculation | 39 | 8.96 |
| Senior Secondary | 89 | 16.73 |
| Graduates | 456 | 78.87 |
| Postgraduates | 58 | 14.56 |
| Doctorates | 8 | 2.36 |
| Work Exposure (in years) | ||
| 1-4 years | 89 | 13.56 |
| 5-8 years | 115 | 25.69 |
| 9-12 years | 165 | 46.68 |
| 12-16 years | 268 | 68.23 |
| More than 16 years | 68 | 13.45 |
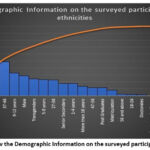 |
Figure 3: To show the Demographic Information on the surveyed participants’ ethnicities Click here to view Figure |
Table 2: Pearson’s association and descriptive analytics.
| Factors | GP | M | JI | SD | HC | SS |
| SS | 3.768 | 0.589 | 0.796 | – | – | – |
| GP | 3.456 | 0.456 | 0.546 | 0.875 | – | – |
| HC | 3.447 | 0.589 | -0.568 | -0.452 | 0.864 | – |
| JI | 4.758 | 0.546 | 0.485 | 0.879 | -0.512 | 0.778 |
Measures of demography
E-Governance Strategy
Nine questions were used to gauge the general public’s opinions of the E-crucial president’s tasks regarding the epidemic. The very first five elements came from Lazarus et al.50, while the last children came from the WHO. The eight items are scored on a five-point rt system, where one represents “strong disagreement” and five represents “total agreement.” This metric was deemed to be trustworthy in the most recent investigation.51 The indicator in this study displays good internal consistency (Cronbach’s alpha = 0:922).
Humanitarian Assistance
Seven items were used to gauge support networks. Structured questionnaires were used to gauge support networks. Eisenberger et al.52 provided the very first four elements, while Heaney 53 provided the latter two. The items evaluate the institution’s and supervisor’s support networks. Participants were required to determine how strongly they disagreed or agreed with the statement (1 = strongly disagree, 5 = strongly agree). Cronbach’s alpha = 0:931 indicates that the model is accurate.
Uncertainty about one’s job
Workers’ anxieties regarding their jobs are measured by employment prospects. De Witte et al.10 included four questions about anticipated employment uncertainty. “Possibilities are I’ll leave my job eventually” and “I’m concerned regarding my employment’s destiny” are among the things. On a 5-point Likert scale, individuals scored each topic from 1 (“completely disagree”) to 5 (“absolutely concur”). This measure was shown to be reliable in the current investigation (Cronbach’s alpha = 0:897).
Wellbeing Shortages
Five factors were used to assess health emergencies. The data was provided by Bech & Gudex et al.54 The purpose of the questionnaires is to gauge the participants’ struggles with their psychological well-being over the preceding period. Positively chosen examples included “I would have felt at ease and relaxed” and “I had already been upbeat and in fantastic emotions.” In this study, healthcare crises were examined using Cronbach’s alpha. Within the context of the current inquiry, this measurement was proved to also be trustworthy (Cronbach’s alpha= 0:8994).
Results
Data collected were analyzed using AMOS 24.0 and SPSS 27.0. The demographic statistics means standard deviation (average and sample variance), and correlations were all analyzed using SPSS (relationship between constructs). For conceptual reliability and validity, AMOS was employed. To test our report’s assumptions, we used the PROCESS macro in SPSS rather than multiple linear regression analysis (SEM). It’s because, unlike the SEM program, conditionally influencing factors and mediational indexes may be estimated quickly and easily, avoiding the problems associated with association estimating in the latent construct’s technique.55
Mechanism for Surveying.
Cronbach’s alpha, composite reliability and divergent validity were used by Henseler et al.56 to assess the estimation procedure. Table 3 shows that Cronbach’s alpha and composite repeatability (CRR) levels are greater than the maximum level of 0.70. Moreover, the AVEG for any measured variables used in this study was higher than 0.50. As a consequence, the results indicate long-term mutual reliability and validity (p. 4). The guarantee of overall benefits has earned the customer’s confidence. Having trust and confidence in the public health system perpetuates its functioning and stimulates participation in healthcare operations. Moreover, trust in the public values in other parts of the constitutional framework is influenced by public frequency in those other parts of the constitutional framework.57 Lastly, people’s confidence is influenced by a variety of actors within and without the public health system. In the long term, such a theoretical model will have to be converted into a policy document and a survey instrument, as well as verified for health services besides the NHS in the United Kingdom. Table 4 shows psychometric properties, in which the reciprocal of each hidden variable’s AVEs ought to be bigger than the neighboring associations. Each one of the equations in the diagonally is higher than the typical association, as shown in Table 4, demonstrating predictive relevance.58
Table 3: Measures of validity and reliability.
| Variable Factors | Measuring Factors | SFL | AVG | CRR |
| E-GOVERNMENT POLICY | GPP1 | 0.644 | 0.622 | 0.934 |
| GPP2 | 0.948 | |||
| GPP3 | 0.912 | |||
| GPP4 | 0.677 | |||
| GPP5 | 0.831 | |||
| GPP6 | 0.798 | |||
| GPP7 | 0.913 | |||
| GPP8 | 0.711 | |||
| SOCIAL NETWORKING SUPPORT | SSR 1 | 0.945 | 0.632 | 0.946 |
| SSR 2 | 0.611 | |||
| SSR 3 | 0.968 | |||
| SSR 4 | 0.845 | |||
| SSR 5 | 0.756 | |||
| SSR 6 | 0.967 | |||
| JOB INSECURITY | JII1 | 0.722 | 0.621 | 0.956 |
| JII2 | 0.833 | |||
| JII3 | 0.823 | |||
| JII4 | 0.917 | |||
| HEALTHCARE CRISIS | HLCC 1 | 0.734 | 0.622 | 0.978 |
| HLCC 2 | 0.834 | |||
| HLCC 3 | 0.768 |
Statistical Technique Impairment
To identify the hazards of similar technique prejudice, Harman’s 1 single trait was used.58 When all of the measured variables were included, the very first component represented 37.29% of the variance throughout all four components with a value higher than just one. That would be less than the permissible threshold of 50 percent. As a result, in our study, general technique variance is not a concern. Additionally, the correlation did significantly skew our results, as shown by the dynamic amplification component (VIF) estimations for all observational data in the analysis being below 4.59
Table 4: Simple mediation coefficient estimates FOR Regression results.
| B% | SEE | p | |
| The E-Governance strategy has degraded as a result of medical emergencies. | 1.021 | 0.234 | p ≤ 0:0001 |
| Rising unemployment has worsened as a result of E-Governance initiatives. | -0.932 | 0.188 | p ≤ 0:0013 |
| Accounting for E-Governance policies, medical emergencies reverted to rising unemployment. | -0.256 | 0.037 | p ≤ 0:0014 |
| E-Governance policy underperformed on medical emergencies while allowing for rising unemployment | 0.256 | 0.035 | p ≤ 0:0001 |
Table 5: The estimated indirect influence of E-Governance policies on medical problems via Employment Prospects.
| B% | SEE | LLCCI | |
| Uncertainty in the workplace | -0.222 | 0.073 | -0.432 |
Immediate and Interaction Impacts are being investigated
The simple mediation analysis reveals overall E-Governance strategies were strongly linked to increased medical emergencies (B = 1.021, p 0.0001), as shown in Table 4, confirming main Hypothesis H1. Rising unemployment was adversely linked with the E-Governance strategy (B = -0.932, p 0.0013), confirming assumption H2. When accounting for E-Governance policies, employment instability was found to be inversely linked with medical emergencies (B = -0.256, p 0.0014) confirming assumption H3. Eventually, the discrimination percentage point detailed implementation revealed that now the path coefficient direction among E-Governance strategy and public health care catastrophes via rising unemployment has been statistically meaningful (B% = -0.218, SEE = 0:0723, 97 percent LLCI = 0:423, & ULCCI=-0.118),47 as seen in Table 5 (B% = -0.222, SEE = 0.073, LLCCI = -0.432, ULCCI = -0.113), lying out beyond zero, validating assumption H4. The unintended byproduct (mediated) was responsible for 42.26% of the net impact. The 4 situations also corroborated Mackinnon’s multiple processes41 and the moderating roles.
Counselling in a regulated manner
Support networks appear to be a modulator of the indirect impacts of the E-Governance strategy on medical emergencies, according to the findings. In comparison to poor social services and high rising unemployment, the plot revealed that having high support networks will lessen the negative impact of electronic government policies on rising unemployment. Whenever the ratings of support networks have been the scale parameter (SD), the positive indirect effect of social E-Governance assistance on medical emergencies mediated employment instability was investigated. The three conditionally secondary impacts were statically important, and bootstrapping intervals confirmed those findings (see Table 6). In conclusion, the results demonstrated a moderate influential communication in which employment uncertainty was a mediating factor of E-Governance tax policies’ effect on health emergencies.
Discussions
In this research, we have examined how COVID-19-wide medical problems were impacted by E-Governance rules. First, it had to be proven whether regulations for e-government constituted, in reality, a predictor of workers’ health disorders. This outcome is consistent with the previous studies1-2. These results are consistent, which raises the question of whether E-Government initiatives had to have an impact on the employees’ health even during the COVID-19 pandemic. For instance, according to Khan et al.,4 it’s possible that perhaps the E-Government presently disregards the emotional psychosocial factors. Therefore, an E-Governance approach should also include steps to help employees with health complications. Moreover, it’s been found that E-Governance legislation is a poor indicator of job instability. It is in line with the observations of.31,32 Due to E-Government measures like shutdowns, which aren’t totally within their authority, employees are concerned about whether or not they will be able to maintain their current jobs. Ultimately, a significant and damaging way that employment uncertainty predicted medical problems. This outcome is consistent with the study that was done.38 The hospitality business in India has found a negative correlation between employment instability and health problems, demonstrating that another connection is just not unique to the advanced economies. Additionally, the results of the mediation impact analysis demonstrate that now the E-Governance strategy reduces unemployment instability both intrinsically and extrinsically. Therefore, any impact of E-Government policies on medical problems is mostly communicated through the occupational category (see Table 7). Economic stress is much more likely to affect individuals who have weak supporting ties with their employers, whereas it’s much less likely to affect individuals who have strong support networks, suggesting that social worth now determines how satisfied we are. It is therefore in favor of Lim, V. K.11
Conceptual Consequences
The present study used a sample from 52 tourist hotspots to evaluate a mediation model in which we expected that now the influence of E-Governance policies on medical emergencies would be moderated by rising unemployment. The degree of interpersonal assistance reduced the secondary impacts of E-Governance policies on medical emergencies via employment instability. Our findings add to the poor understanding of E-Governance policies and workers’ medical concerns in the setting of the epidemic, notably in India’s tourism industry. Firstly, the results add to the healthcare crisis study by evaluating the effects of contextual variables including such E-Governance policies on healthcare emergencies among tourist personnel. Secondly, to our understanding, this is the very first study to look into the influence of E-Governance policies on medical emergencies via the mediation relationship between job instability, as well as whether or not the unintended byproduct is reliant on public support. Thirdly, this research is unusual in that it examines support networks as a mediator for developing organizational support networks throughout an epidemic.
Table 6: A probabilistic process monitoring study was undertaken (N = 433).
| B% | SEE | p | LLCC I | ULCC I | |
| JOB INSECURITY | |||||
| Policy on E-Governance (GPP) | -0.234 | 0.034 | p ≤ 0:0011 | -0.168 | -0.322 |
| Social assistance (SS) | 0.143 | 0.022 | p ≤ 0:001 | 0.188 | 0.309 |
| (GPP x SS) | -0.112 | 0.054 | 0.034 | -0.029 | -0.011 |
| Health-care shortages | |||||
| Strategy on E-Governance | 0.214 | 0.038 | p ≤ 0:001 | 0.122 | 0.234 |
| Uncertainty in the job | -0.292 | 0.032 | p ≤ 0:001 | -0.223 | 0.018 |
|
At a certain degree of social assistance, there is a conditionally indirect consequence |
|||||
| 1 standard deviation below the median | 0.324 | 0.052 | p ≤ 0:001 | 0.211 | 0.418 |
| Median | 0.248 | 0.038 | p ≤ 0:001 | 0.156 | 0.322 |
| 1 standard deviation above the median | 0.126 | 0.058 | 0.006 | 0.078 | 0.264 |
Table 7: Mediation Analysis Indicator
| Indices | SEE | LLCCI | |
| Impact of Social Assistance | 0.034 | 0.021 | 0.058 |
Management and Operational Consequences
This research has several policy implications. To begin with, this study can help firms by providing guidelines for managing their personnel throughout a catastrophe. It underlines a need for the administration to emphasize psychological factors by giving workers tools to help them cope with the current healthcare crisis. Since clients engage with staff to deliver the services, workers’ medical problems must be prioritized in the tourist industry. Secondly, due to the obvious pandemic’s rapid evolutionary changes behavior, this research could aid firms in developing a strategy to give or increase social assistance among their workers. The human resource department, for instance, must concentrate on strategies to reduce employment instability by implementing educational programs that increase support networks. Organizations will be able to dissipate misconceptions and alleviate personal fears and anxieties by providing employees with accurate and timely information even during an epidemic.
Conclusions
In general, this experimental research looks at E-Governance policies on medical emergencies from the employees’ perspective. The data was gathered through a self-assessment, and the results showed that E-Governance regulations were a reliable indicator of medical situations. Stagnant wages were also a significant mediator between the E-Governance strategic plan and the catastrophic healthcare events, with social connections mediating. Employees with weaker institutional support systems reported higher levels of job insufficiency, whereas those with stronger support systems reported lower levels of workforce insufficiency. The implications for management and theory are also looked at. In conclusion, this empirical study examines E-Government regulations on healthcare crises once more from the viewpoint of workers. Data was collected using a self-reported measurement, and the findings indicated that e-government legislation was a significant factor in predicting emergency scenarios. Moreover, high unemployment was indeed a key mediator between the E-Governance strategic plan and global health disasters, with support system having to serve as a crucial moderator variable: individuals with weaker support systems outside of their organization had much more employment ambiguity, whereas employees with solid support channels had less. Managerial and theoretical ramifications are also examined. Notwithstanding its accomplishments, the current study has limited what future research should address. For starters, the sampling was restricted to India’s tourism business, so future research will need to expand to other countries and industries. Secondly, our research used a cross-sectional approach, allowing us to deduce correlations but not causation or connection orientations. The information gathered was focused on the COVID-19 epidemic’s direct impact at the moment of gathering. So, because the self-reporting approach was employed to assess E-Governance policies, employment instability, support networks, and medical emergencies, respondents were able to react in a manner that matched their desirability biases.58 To corroborate the robustness of our findings, future research must employ more observable and standardized instruments (longitudinal cohort methodology). Finally, we did not consider all factors which could have impacted the outcomes, such as age and gender.
Acknowledgment
The author(s) express sincere gratitude to Dr. Kamal Upreti, Department of Computer Science, CHRIST (Deemed to be University), Delhi NCR, Ghaziabad, Uttar Pradesh, India, for his invaluable guidance and support throughout this research. His insights and expertise have significantly contributed to the completion of this work.
Funding Sources
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Conflict of Interest
The author(s) do not have any conflict of interest.
Data Availability Statement
This statement does not apply to this article.
Ethics Statement
This research did not involve human participants, animal subjects, or any material that requires ethical approval.
Informed Consent Statement
This study did not involve human participants, and therefore, informed consent was not required.
Clinical Trial Registration
This research does not involve any clinical trials
Author contributions
Prashant Vats: Conceptualization, Methodology, Software, Field study Data curation, Writing-Original draft preparation, Software, Validation., Field study
Ashok Kumar Saini: Visualization, Investigation, Writing-Reviewing, and Editing.
References
- Jemberie WB, Stewart Williams J, Eriksson M, Grönlund AS, Ng N, Blom Nilsson M, Padyab M, Priest KC, Sandlund M, Snellman F, McCarty D, Lundgren LM. Substance Use Disorders and COVID-19: Multi-Faceted Problems Which Require Multi-Pronged Solutions. Front Psychiatry. 2020, 21; 11: 714.
CrossRef - Sibley CG, Greaves LM, Satherley N, Wilson MS, Overall NC, Lee CHJ, Milojev P, Bulbulia J, Osborne D, Milfont TL, Houkamau CA, Duck IM, Vickers-Jones R, Barlow FK. Effects of the COVID-19 pandemic and nationwide lockdown on trust, attitudes toward government, and well-being. Am Psychol. 2020; 75(5):618-630.
CrossRef - Wang C, Pan R, Wan X, Tan Y, Xu L, Ho CS, Ho RC. Immediate Psychological Responses and Associated Factors during the Initial Stage of the 2019 Coronavirus Disease (COVID-19) Epidemic among the General Population in China. Int J Environ Res Public Health. 2020, 6;17(5):1729.
CrossRef - Khan, Kanwal Iqbal, Amna Niazi, Adeel Nasir, et al., “The effect of COVID-19 on the hospitality industry: The implication for open innovation.” Journal of Open Innovation: Technology, Market, and Complexity, 2021, 7 (1), 30.
CrossRef - Apouey B, Roulet A, Solal I, Stabile M. Gig Workers during the COVID-19 Crisis in France: Financial Precarity and Mental Well-Being. J Urban Health. 2020; 97 (6):776-795.
CrossRef - Makowiecki, Matteo, Valentina Ungaretti, Marta Arzilli, et al., “Subjective wellbeing of Italian healthcare professionals during the SARS-CoV-2 outbreak: a quasi-experiment.” International Journal of Wellbeing, 2020,10 (3).
CrossRef - Saladino V, Algeri D, Auriemma V. The Psychological and Social Impact of Covid-19: New Perspectives of Well-Being. Front Psychol. 2020; 11:577684.
CrossRef - Zhang SX, Wang Y, Rauch A, Wei F. Unprecedented disruption of lives and work: Health, distress and life satisfaction of working adults in China one month into the COVID-19 outbreak. Psychiatry Res. 2020; 288:112958.
CrossRef - Giunchi, M., Emanuel, F., Chambel, M.J. and Ghislieri, C., “Job insecurity, workload and job exhaustion in temporary agency workers (TAWs) Gender differences.”, Career Development International, 2016, 21(1), 3-18.
CrossRef - De Witte, H., Vander Elst, T., & De Cuyper, N., “Job insecurity, health and well-being.” In J. Vuori, R. Blonk, & R. H. Price (Eds.), Sustainable working lives: Managing work transitions and health throughout the life course, 2015, 109–128.
CrossRef - Lim, V. K., “Job insecurity and its outcomes: Moderating effects of work-based and nonwork-based social support”, Human Relations, 1996, 49 (2), 171-194.
CrossRef - Spence, A. M., “The financial and economic crisis and the developing world.”, Journal of Policy Modeling, 2009, 31(4), 502-508.
CrossRef - Ashford, S. J., Lee, C., & Bobko, P., “Content, cause, and consequences of job insecurity: A theory-based measure and substantive test.”, Academy of Management Journal, 1989, 32(4), 803-829.
CrossRef - Lima CKT, Carvalho PMM, Lima IAAS, Nunes JVAO, Saraiva JS, de Souza RI, da Silva CGL, Neto MLR. The emotional impact of Coronavirus 2019-nCoV (new Coronavirus disease). Psychiatry Res. 2020; 287: 112915.
CrossRef - Wilson JM, Lee J, Fitzgerald HN, Oosterhoff B, Sevi B, Shook NJ. Job Insecurity and Financial Concern During the COVID-19 Pandemic Are Associated with Worse Mental Health. J Occup Environ Med. 2020;62(9):686-691.
CrossRef - McGee RE, Thompson NJ. Unemployment and depression among emerging adults in 12 states, Behavioral Risk Factor Surveillance System, 2010. Prev Chronic Dis. 2015, 19; 12: E38.
CrossRef - Olesen SC, Butterworth P, Leach LS, Kelaher M, Pirkis J. Mental health affects future employment as job loss affects mental health: findings from a longitudinal population study. BMC Psychiatry. 2013; 13: 144.
CrossRef - Wood SJ, Michaelides G, Inceoglu I, Hurren ET, Daniels K, Niven K. Homeworking, Well-Being and the COVID-19 Pandemic: A Diary Study. Int J Environ Res Public Health. 2021; 18 (14):7575.
CrossRef - Sonnentag, S., “Dynamics of well-being.”, Rev. Organ. Psychol. Organ. Behav., 2015, 2 (1), 261-293.
CrossRef - Evolahti A, Hultell D, Collins A. Development of burnout in middle-aged working women: a longitudinal study. J Womens Health (Larchmt). 2013;22(1):94-103.
CrossRef - Karasek Jr, R. A., “Job demands, job decision latitude, and mental strain: Implications for job redesign.”, Administrative Science Quarterly, 1979, 285-308.
CrossRef - Taylor, S. E., “Social support: A review.”, The Oxford Handbook of Health Psychology, 2011, 1, 189-214.
CrossRef - Fenlason, K. J., & Beehr, T. A., “Social support and occupational stress: Effects of talking to others.”, Journal of Organizational Behavior, 1994 15(2), 157-175.
CrossRef - George JM, Reed TF, Ballard KA, Colin J, Fielding J. Contact with AIDS patients as a source of work-related distress: effects of organizational and social support. Acad Manage J. 1993; 36(1):157-71.
CrossRef - de Zwart O, Veldhuijzen IK, Elam G, Aro AR, Abraham T, Bishop GD, Voeten HA, Richardus JH, Brug J. Perceived threat, risk perception, and efficacy beliefs related to SARS and other (emerging) infectious diseases: results of an international survey. Int J Behav Med. 2009; 16 (1): 30-40.
CrossRef - Mækelæ MJ, Reggev N, Dutra N, Tamayo RM, Silva-Sobrinho RA, Klevjer K, Pfuhl G. Perceived efficacy of COVID-19 restrictions, reactions and their impact on mental health during the early phase of the outbreak in six countries. R Soc Open Sci. 2020; 7 (8): 200644.
CrossRef - Bavel JJV, Baicker K, Boggio PS, Capraro V, Cichocka A, Cikara M, Crockett MJ, Crum AJ, Douglas KM, Druckman JN, Drury J, Dube O, Ellemers N, Finkel EJ, Fowler JH, Gelfand M, Han S, Haslam SA, Jetten J, Kitayama S, Mobbs D, Napper LE, Packer DJ, Pennycook G, Peters E, Petty RE, Rand DG, Reicher SD, Schnall S, Shariff A, Skitka LJ, Smith SS, Sunstein CR, Tabri N, Tucker JA, Linden SV, Lange PV, Weeden KA, Wohl MJA, Zaki J, Zion SR, Willer R. Using social and behavioral science to support COVID-19 pandemic response. Nat Hum Behav. 2020;4(5):460-471.
CrossRef - Rudolph CW, Zacher H. COVID-19 and careers: On the futility of generational explanations. J Vocat Behav. 2020; 119: 103433.
CrossRef - Hawkley LC, Cacioppo JT. Loneliness matters: a theoretical and empirical review of consequences and mechanisms. Ann Behav Med. 2010; 40 (2): 218 – 27.
CrossRef - Dean M, McClement S, Bond JB Jr, Daeninck PJ, Nelson F. Parental experiences of adult child death from cancer. J Palliat Med. 2005; 8 (4): 751 – 65.
CrossRef - Watson J, Simmonds A, La Fontaine M, Fockler ME. Pregnancy and infant loss: a survey of families’ experiences in Ontario Canada. BMC Pregnancy Childbirth. 2019, 16; 19 (1): 129.
CrossRef - Kachanoff, F. J., Bigman, Y. E., Kapsaskis, K., & Gray, K. Measuring Realistic and Symbolic Threats of COVID-19 and Their Unique Impacts on Well-Being and Adherence to Public Health Behaviors. Social Psychological and Personality Science, 2021, 12(5), 603-616.
CrossRef - Kahneman, D., & Snell, J., “Predicting a changing taste: Do people know what they will like?”, Journal of Behavioral Decision Making, 1992, 5(3), 187-200.
CrossRef - Kahneman, D., & Tversky, A., “On the psychology of prediction.”, Psychological Review, 1973, 80(4), 237.
CrossRef - Greenhalgh, L., & Rosenblatt, Z., “Job insecurity: Toward conceptual clarity.”, Academy of Management Review, 1984, 9 (3), 438-448.
CrossRef - Cheng, G. H. L., & Chan, D. K. S., “Who suffers more from job insecurity? A meta‐analytic review.”, Applied Psychology, 2008, 57 (2), 272-303.
CrossRef - Dekker, S. W., & Schaufeli, W. B., “The effects of job insecurity on psychological health and withdrawal: A longitudinal study.”, Australian Psychologist, 1995, 30 (1), 57-63.
CrossRef - Kinnunen, U., Mäkikangas, A., Mauno, S., et al., “Development of perceived job insecurity across two years: associations with antecedents and employee outcomes”, Journal of Occupational Health Psychology, 2014, 19 (2), 243.
CrossRef - Norlund S, Reuterwall C, Höög J, Lindahl B, Janlert U, Birgander LS. Burnout, working conditions and gender–results from the northern Sweden MONICA Study. BMC Public Health. 2010; 10: 326.
CrossRef - Jose A. Llosa, Sara Menéndez-Espina, Esteban Agulló-Tomás, and Julio Rodríguez-Suárez., “Job uncertainty and mental health: a meta-analytic review of the consequences of precarious work on mental disorders.”, Annals of Psychology, 2018, 34 (2), 211–223.
CrossRef - Meyer B, Zill A, Dilba D, Gerlach R, Schumann S. Employee psychological well-being during the COVID-19 pandemic in Germany: A longitudinal study of demands, resources, and exhaustion. Int J Psychol. 2021; 56 (4):532-550.
CrossRef - Ganson KT, Tsai AC, Weiser SD, Benabou SE, Nagata JM. Job Insecurity and Symptoms of Anxiety and Depression Among U.S. Young Adults During COVID-19. J Adolesc Health. 2021; 68 (1): 53-56.
CrossRef - Pacheco H, Díaz-López S, Jarre E, Pacheco H, Méndez W, Zamora-Ledezma E. NO2levels after the COVID-19 lockdown in Ecuador: A trade-off between environment and human health. Urban Clim. 2020; 34: 100674.
CrossRef - Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, Rubin GJ. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. 2020; 395 (10227): 912-920.
CrossRef - Lee S. Subjective Well-being and Mental Health During the Pandemic Outbreak: Exploring the Role of Institutional Trust. Res Aging. 2022;44(1):10-21.
CrossRef - Kalleberg, A. L., “Precarious work, insecure workers: Employment relations in transition.”, American Sociological Review, 2009, 74 (1), 1-22.
CrossRef - Sarason, B. R., Pierce, G. R., & Sarason, I. G., “Social Support: The Sense of Acceptance and the Role of Relationships.”, In Social Support: An Interactional View.1990, Hoboken, NJ: John Wiley & Son.
- Stuart N, Adams J. The sustainability of Canada’s healthcare system: a framework for advancing the debate. Healthc Q. 2007; 10 (2): 96 – 103.
CrossRef - de Girolamo, Giovanni., “Monitoring knowledge, risk perceptions, preventive behaviours and trust to inform pandemic outbreak response.” 2021.
- Lazarus JV, Binagwaho A, El-Mohandes AAE, Fielding JE, Larson HJ, Plasència A, Andriukaitis V, Ratzan SC. Keeping governments accountable: the COVID-19 Assessment Scorecard (COVID-SCORE). Nat Med. 2020;26(7):1005-1008.
CrossRef - Eisenberger R, Cummings J, Armeli S, Lynch P. Perceived organizational support, discretionary treatment, and job satisfaction. J Appl Psychol. 1997;82(5): 812-20.
CrossRef - Heaney CA. Enhancing social support at the workplace: assessing the effects of the caregiver support program. Health Educ Q. 1991 Winter;18(4):477-94.
CrossRef - Bech P, Gudex C, Johansen KS. The WHO (Ten) Well-Being Index: validation in diabetes. Psychother Psychosom. 1996; 65 (4):183-90.
CrossRef - Igartua JJ, Hayes AF. Mediation, Moderation, and Conditional Process Analysis: Concepts, Computations, and Some Common Confusions. Span J Psychol. 2021; 24: e49.
CrossRef - JHenseler, Jörg, Christian M. Ringle, and Marko Sarstedt. “A new criterion for assessing discriminant validity in variance-based structural equation modeling.” Journal of the academy of marketing science, 2015 43: 115-135.
CrossRef - Fornell, C., “Structural equation models with unobservable variables and measurement error: Algebra and statistics”, 1981.
CrossRef - Podsakoff PM, MacKenzie SB, Lee JY, Podsakoff NP. Common method biases in behavioral research: a critical review of the literature and recommended remedies. J Appl Psychol. 2003; 88 (5): 879-903.
CrossRef







