Najam Siddiqi1 and Edmond YS Chao2
and Edmond YS Chao2
1Department of Anatomy and Neurobiology, College of Medicine and Health Sciences, National University of Sciences and Technology, Worked as Postdoc Fellow, Orthopedic Biomechanics Laboratory, School of Medicine, Johns Hopkins University, Rutland Avenue, Baltimore, MD, USA.
2Biomechanics Laboratory, School of Medicine, Johns Hopkins University, Rutland Avenue, Baltimore, MD, USA.
Corresponding Author E-mail: najamsiddiqi@nu.edu.om
DOI : https://dx.doi.org/10.13005/bpj/2968
Abstract
With emerging technologies and improved operative techniques, cementless total hip arthroplasty is becoming more popular and showing better results. The femoral prosthesis and intramedullary nail should precisely fit in the medullary canal to prevent micromotion and loosening. Most of the femoral prosthesis and nail designs are made from the data obtained from Caucasian femur and may not press fit if used in Asian populations. This study compares the femoral medullary canal diameter in American and Oriental populations at different bony levels. A total of 245 dry femora were collected which included 47 from United States, 77 from China, 44 from Japan, 50 from Korea and 27 from Taiwan, and plan radiographs were taken. Radiographs were digitized to measure the medullary canal width at 20% (lesser trochanter; LT), 35% (supra-isthmus; SI), 50% (mid-isthmus; MI), 65% and 80% of the total femur length. The results revealed significant differences in the medullary canal width between the US and East Asian Oriental populations. The medullary canal in the US population was significantly larger at the LT, SI, MI, and 65% but significantly smaller at 80% of the femoral shaft length compared to the East Asian populations. Among the East Asian populations, significant differences were obse4rved between the Chinese and Taiwanese populations as well as the Japanese and Taiwanese populations. The Taiwanese population had the smallest femoral medullary canal size among the east Asian populations. We conclude that there are significant differences in the femoral medullary width between the American and East Asian populations. These results will be useful for surgeons operating on the proximal or distal femur.
Keywords
American; East Asian; Isthmus; Medullary Canal; Proximal Femur
Download this article as:| Copy the following to cite this article: Siddiqi N, Chao E. Y. S. Differences in Femoral Medullary Canal Dimensions in the USA and East Asian Populations. Biomed Pharmacol J 2024;17(3). |
| Copy the following to cite this URL: Siddiqi N, Chao E. Y. S. Differences in Femoral Medullary Canal Dimensions in the USA and East Asian Populations. Biomed Pharmacol J 2024;17(3). Available from: https://bit.ly/47Gxafq |
Introduction
Total hip arthroplasty (THA) remains the most appropriate treatment for patients with severe degenerative arthritis or osteonecrosis. Femoral morphology influences initial fixation and secondary osteointegration, which are critical for cementless stem fixation. Uncemented implants became more popular in the USA after advances in mechanical engineering for press-fit fixation1. Studies have suggested component instability is a cause for subsidence and thigh pain 2,3. Best press fit of the femoral stem in the femoral medullary canal ensures better results in terms of achieving three-point fixation of the flat and tapered stem and prevent postoperative subsidence, loosening and thigh pain4.
The femoral dimensions are different in different races. Darius reported femurs of female Caucasians from Asia are different from Caucasians at the isthmus; Caucasian’s femora are wider 5. Most of the prostheses are made from the Caucasian data and it is suggested that there could be a miss-match if used in Asian populations6, 7. Several Japanese studies reported the importance of the endosteal canal diameter of the proximal femur for cementless hip system optimum fixation8. Total hip arthroplasty should be made to get the best results because the morphology of the proximal femur shows racial differences9.
This data may be useful for designing the implants for the femoral shaft in the two populations and for the surgeons in decision-making and preoperative planning for THA.
Hypothesis
It is hypothesized that the femoral medullary canal diameters at different bone lengths are different in the US and East Asian populations.
Objectives
The objective of this study was to study the femoral medullary canal diameter width in American and Oriental populations at 20%, 35%, 50%, 65% and 80% of the length of the femur on plane radiographs.
Material and Methods
Study Design
The study utilized dry cadaveric femurs from American and Oriental cohorts, assessing the medullary canal diameter at 20%, 35%, 50%, 65%, and 80% of the bone length using plane radiographs. A total of 245 dry femora were collected from the USA, Beijing, Shanghai, Korea, Japan, and Taiwan.
Collection of Bone Specimens and Radiographs
American Femora
A total of 47 white American dry femora (23 right, 24 left) were collected from Mayo Clinic in the USA with no record of their age or gender. These are collected from the donated bodies to Mayo clinic for teaching purposes.
East Asian Femora
One hundred and ninety-eight unpaired dry femora were received from Beijing, China (27 femora, 17 right, 10 left), Shanghai, China (50 femora, 24 right, 26 left), Taipei, Taiwan (27 femora, 12 right, 15 left), Seoul, Korea (50 femora, 44 right, 6 left) and Kurume, Japan (44 femora, 21 right 23).
Most of the femora were collected from the anatomy department or orthopedic research laboratories and were without either sex or any other identifications. These bones were not matched from the same donor, and were embalmed. Bones with internal fixations, deformities or fractures were excluded from this study. When both side femora were available, only one side bone was included in the study to ensure true random unbiased selection. This research was conducted after approval from the concerned Ethical committees.
Identification of Key Measurement Parameters
The femoral medullary canal diameter was measured at the following sites on a plane radiograph:
20% (lesser trochanter)
35% (supra-isthmus)
50% (mid-isthmus),
65%
80%
Measurement Technique
Radiographic measurements were chosen due to their comparability with CT scans in assessing femoral dimensions, particularly at critical points such as the isthmus10.A bone-holding jig was developed to ensure consistent bone positions and avoid rotation of the bone during radiography11.
A digitizer table was used to mark the identified points on the radiographs and data was collected on the hard disc. This digitizer consisted of an x-ray table with an integrated electrostatic micro grid which facilitates accurate point position (0.01mm accuracy) through a movable metal crosshair. A custom-made software program was written through the serial port for the collection of the data. A series of subprograms were used to compute the x-ray magnification factor, and to format the data so that it can be transferred to the database software package.
The distance between the digitizer grid and the radiograph was calibrated at the beginning of digitizing using a radio-opaque scale on the x-ray film. Exact magnification was also computed although the distance between the specimens, the radiation source and the cassette were maintained constant. This software program calculated distances between two selected endpoints on the digitizer. Measurements were recorded three times with the calculation of the mean and standard deviations. User to re-digitize the parameter if the percentage errors between the mean and standard deviation were exceeding 5%. Repeatability and reliability tests were conducted and reported earlier 11.
The femoral medullary canal diameter was measured for each femur12.
The anatomical axis of the femur was defined by a line passing through the midpoints of the medullary canal at 20mm proximal and distal to the canal isthmus (X-X’) [20] (Figure 1.). Two lines were drawn passing perpendicular to the femoral axis at the superior surface of femoral head (A-A’) and other connecting the inferior surface of the medial and lateral condyles (B-B’). The mid-isthmus was defined as the narrowest point between the endosteal surfaces of the medial and lateral cortices and lies at the mid-point of the femoral shaft (D-D’). The radiographs were then placed on the digitizer and points A’ and B’ were digitized to calculate the length of the femur (Figure 1.). The software after calculating the length of the femur can identify these 5 levels to be marked at 20%, 35%, 50% 65% and 80% of the total length of the femur. The points can be adjusted if needed especially if it is not passing through the midpoint of the lessor trochanter. Two points on the inner margin of the medullary canal were then digitized at each level shown as red and the software will calculate the distance between these two points which is the width of the medullary canal.
Statistical Correlation Analysis
Student’s t-test was used for the significance of normally distributed continuous variables. Two groups were compared by using Analysis of variance (ANOVA). Relationships between the variables were analyzed by Pearson’s correlation. A p-value <0.05 was considered as significant.
Population Demographics
While specific demographic data (age, sex) were not available for the specimens used in this study, it’s acknowledged that these factors can influence femoral canal dimensions, as reported in previous literature5,13.
Results
American vs. East Asian Populations
The femoral medullary canal width measurements are given in Table 1. Significant diameter differences were observed in the femoral canal diameters of the American population when compared to East Asian populations (Figure 1). The American femoral canal diameter was significantly wider at the lesser trochanter (20%), supra isthmus (35%) and mid-isthmus (50%) (p<0.05) than all the East Asian populations. (Figure. 2, 3, 4). At 65% no significant differences were noted. Conversely, at 80% of the bone length, the American population exhibited significantly narrow diameter (p<0.05) when compared with the East Asian populations except Taiwanese (Figure 5). When compare the American and the Korean populations, femoral medullary canal diameter was significantly narrower in Korean population at all the levels except 80% of the bone length where it was significantly wider (Figure 1, 6).
Table 1: The femoral medullary canal width of USA and East Asian populations at different femoral bone lengths
|
Femoral bone length |
USA |
China (B) |
China (S) |
Japan |
Korea |
Taiwan |
|
LT (20%) |
20.16 ±4.0 |
16.47 ±2.6 |
16.24 ±2.1 |
16.83 ±2.4 |
14.91 ±2.5 |
13.41 ±2.9 |
|
SI (35%) |
17.64 ±3.5 |
11.89 ±2.1 |
11.35 ±1.9 |
12.40 ±1.9 |
10.88 ±2.0 |
9.50 ±2.4 |
|
MI (50%) |
19.52 ±2.4 |
12.39 ±1.8 |
11.93± 2.0 |
12.45 ±1.7 |
11.62± 1.8 |
9.93 ±2.5 |
|
65% |
19.63 ±3.8 |
18.34 ±2.0 |
18.03 ±2.9 |
18.50 ±2.3 |
16.89 ±2.6 |
15.29 ±2.6 |
|
80% |
25.42 ±4.2 |
29.76 ±3.1 |
29.51 ±3.4 |
30.08 ±3.0 |
28.71 ±3.4 |
27.10 ±2.5 |
East Asian Population
Within East Asian populations, variations were noted between different subgroups particularly at the mid-isthmus. Medullary canal diameter reduces significantly from 20% to 35% levels but did not show any change between supra-isthmus and mid-isthmus regions (Figure 1). The medullary canal significantly increases from 65% to 80% of the bone length (Figure 1). There was a significant difference noted between the femoral medullary canal diameter between the Chinese (Beijing and Shanghai) and Taiwanese populations at all the levels except 80% (Figure 1). Taiwanese population was significantly (p<0.05) narrower than Chinese and Japanese populations at 35%, 50% and 65% levels of the femoral bone length (Figure 2,3,4,5).
On the lateral view radiographs, a significant (p<0.05) wider femoral medullary canal diameter in the American population at 20%, and a narrower diameter (p<0.05) at 80% of the bone length when compared to East Asian populations. The Chinese populations (Beijing and Shanghai) are significantly wider (p<0.05) than the Taiwanese populations at 20% and 80% level of the femoral length. (Figure 1.2,3,4,5). A significant difference was also seen between the Japanese and the Taiwanese populations at 20%, 35%, and 50% levels of the femoral bone length (Figure 2,3,4,5).
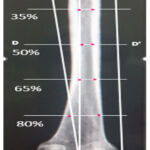 |
Figure 1: AP radiograph shows the method drawing the anatomical axis of the femur and digitizing the points (red) and software measure the distance between these points to calculate the femoral medullary canal widths at 20%, 35%, 50%, 65% and 80% of the length of the femur. |
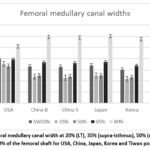 |
Figure 2: Femoral medullary canal width at 20% (LT), 35% (supra-isthmus), 50% (mid-isthmus), 65% and 80% of the femoral shaft for USA, China, Japan, Korea and Tiwan populations.
|
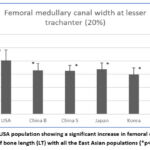 |
Figure 3: The USA population showing a significant increase in femoral canal width at 20% of bone length (LT) with all the East Asian populations (*p<0.05).
|
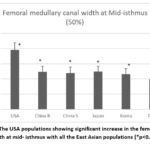 |
Figure 4: The USA populations showing significant increase in the femoral canal width at mid- isthmus with all the East Asian populations (*p<0.05).
|
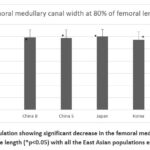 |
Figure 5: USA population showing significant decrease in the femoral medullary canal width at 80% of bone length (*p<0.05) with all the East Asian populations except Taiwan.
|
Discussion
Significant differences were observed between the US and East Asian populations in the femoral medullary diameters at the lesser trochanter (20%), supra-isthmus (35), mid-isthmus (50%), 65% and 80% of the femoral bone length studied. Our tested hypothesis that the femoral medullary canal width at different femoral bone lengths is different in the US and East Asian populations is affirmed.
The US femoral canal widths were significantly wider at all the levels of femoral bone length studied expect at 80% of the bone length where it was significantly narrower. The lesser trochanter and mid-isthmus levels are extremely important for the fixation of the femoral stem while the distal end of the femoral (80%) houses the lower end of the intertrochanteric nail in cases of femoral shaft fractures.
Femoral Canal Mid-isthmus Diameter
Summary of the mid-isthmus femoral medullary canal diameters for Western and East Asian countries reported in literature is given in Table 2.
Table 2: Summary of the results of the femoral canal mid-isthmus width reported in literature
|
|
Author |
Year |
Country |
Subject |
Methods |
Diameter (mean ±SD mm) |
Diameter (Present study) |
|
1 |
Onoue et al (23) Bo et al (24) |
1979
1997 |
Japan
Japan |
Patients
Patients |
AP Radiograph 3D reconstruction |
10.9±1.9
10.40±2.60 |
12.45±1.7 |
|
2 |
Nobel et al. (6) Darius et al (5) |
1988
2022 |
Caucasian
Caucasian |
Cadavers
Patients |
Radiograph
3D CT Scan |
16.9±3.5
10.71±2.2 |
19.52±2.4 |
|
4 |
Khang et al.(25) |
2003 |
Korean |
Volunteers |
3D reconstruction |
12.6±2,3 |
11.62±1.8 |
|
5 |
Wang et al. (26) |
2009 |
Chinese |
Cadavers |
Canal cast mold |
14.67±1.52 |
12.39±1.8 |
|
6 |
Xiu-yun Su et al (13) |
2015 |
Chinese |
Patients |
3D reconstruction |
10.49±1.52 |
11.93±2.0 |
|
7 |
Laine et al. (27) |
2000 |
Finnish |
Cadavers |
3D reconstruction |
14.09±2.81 |
|
|
8 |
Massin et al. (28) |
2000 |
French |
Patients |
AP radiograph |
12.40±2.30 |
|
USA vs East Asian Populations
Studies using 3D-CT scans have reported Caucasian populations generally showing narrow isthmus diameters compared to Asian populations5, 14. Darius conducted a similar study on 1189 Asian and Caucasian cohorts and using a 3D-CT scan reported a significantly narrow isthmus in Caucasians (10.6 ±2.3 mm) as compared to this study where the USA mid-isthmus diameter was 16.64 mm. Darius data was a mix data including 67% Caucasians and 30% Asians; this Caucasian data was collected from a German company Stryker Trauma GmbH so it constituted of German population and not the US population5. This study revealed significant wider in the femoral canal diameter in USA population when compared with the East Asian populations. East Asian populations from this study reported a range from 12.39 mm to 9.93 mm, with an average of 11.00±1.90mm for mid-isthmus diameter, with is similar reported by Daruis which was 11.93±2.0 mm5. Finish and French mid-isthmus width revealed slightly narrower in the size as compared to the US diameter observed in this study 21,22. No significant difference was reported between the male and female cohorts5.
East Asian Population
Chinese Populations
Xiu-Yun Su also reported an isthmus diameter of an average of 10.49±1.52 mm at mid-isthmus, Lin Wang reported an isthmus diameter of 10.58 mm in Chinese population13,21. Su XY in a study of 204 healthy Chinese by using a 3D CT scan, an average isthmus diameter of 10.49±1.52 (10.68 in males vs 10.05 in females) 13. Another study conducted by Zhang Yang in Chinese population and using CT scan in 80 healthy young individuals (20-45 years) reported isthmus diameter of 11.34 ±1.68 mm which is in close agreement with the Chinese population in this study15. This study reported isthmus diameter of Chinese population was 12.39 mm from Beijing and 11.93 mm from Shanghai cohorts. This study revealed similar results, however, the technique was different. Wang et al. reported 14.6 mm but used canal mold technique23. This demonstrates that radiographs are good enough to give the required measurement if taken properly. The gender difference is also not significant. This study revealed a significant wider femoral canal width in Chinese population when compared with Tiawan population.
Japanese Populations
Japanese femoral width reported average of 12.45 mm in this study which is close to data published in the literature. Others also reported an average of 10 mm mid-isthmus diameters in Japanese population 24,25. Japanese population were significantly wider than Tawan population.
Korean Populations
Khang et al reported an average of 12.6 mm mid-isthmus diameter in Korean population as compared to 11.62 mm reported in this study 26.
Proximal Femur Medullary Canal Diameter
Proximal femoral medullary canal diameters also revealed significant differences among the Caucasian and east Asian populations. Marked differences in the geometry of the femur of the Japanese and the US population were reported in literature11, 17.
Nitesh in his study reported medullary canal width (50 mm below the lesser trochanter) was 17.63±3.73 in Non-Asians (Australian, European) using radiographs which agrees with the US data in this study (17.64 mm)16.
Wang reported 18.07 mm medullary diameter 20 mm below the lesser trochanter in the Chinese population14. Our study reported 16.47 mm. Slight variation might be due to the difference in the part of the femur where the measurement was taken.
This study revealed different patterns of femoral canal diameters in the USA and East Asian populations. In the American population, the femoral medullary canal diameter gradually decreases from 20% to 50%; then gradually increases to 80% of femoral bone length. On the other hand, in the East Asian population medullary canal diameter decreases from 20% of bone length to 35% and remains the same at 50%, then size increases to 65% and again increases sharply to its maximum at 80% of the length of the bone (Figure 2). The USA population exhibits significant smaller medullar canal (p<0.05) at the 80% of the bone length (Figure 2,3,4,5,6 7).
Radiographs Versus CT Scan
The data reported in this paper was collected on plain radiographs which is comparable with the CT scan data. A study reported a better correlation of the actual bone measurements with the CT than radiographs10. Correlation of the CT and radiographs was almost the same at the isthmus part of the bone (0.867 for radiographs and 0.818 for CT). This means that radiographs may almost be used at places where CT scan is not available. It was reported that CT scan images may show errors in real measurements due to 2-5 mm of thickness of the slices and 10 mm of slice spacing4, 18.
Tailoring prosthetic implants to fit the specific anatomical characteristics of different ethnic groups is crucial for achieving optimal stability and load transfer in THA6, 18. Optimum clinical results in cementless THA can only be achieved if the prosthesis is designed according to the shape of the femur. Metaphyseal fit to achieve physiologic-like implant-bone load transfer and minimizing stress shielding and bone remodeling was reported by several studies6,19. Femoral stem micromotion due to miss-fit results in torsional motion thus ending up in loosening20. Hence endosteal geometry of the femur is of utmost importance for good clinical results specially for different races. The femoral component must match the shape of the femur. The stem width must be narrow enough to pass the narrowest part of the isthmus. On the other hand, in the Asians the width of the shaft at calcar is less than Caucasian, then decrease to becomes the same at mid isthmus and mid isthmus. Accurate preoperative planning is essential, particularly in selecting implant sizes that match the narrower dimensions of the femoral canal in Oriental populations at critical points such as the isthmus.
Limitation of this study was that the age and sex of the femora which were not available. It is reported that the height and sex did not correlate with the femoral shaft diameter3, 12, 27, 28. Milligan observed that increase in femoral canal diameter in males from 40 to 80 years was only 0.6mm and showing a poor correlation (r=0.071) with increasing of age 12. However, in females the increase is 3.2 mm (r=0.31), which is due to the menopause and hormonal changes at old age. In this paper we observed a significant change in shape of the medullary canal among the Caucasians and the Asians population which may not change with increase in the age. Preoperative planning in older women after menopause should be done more carefully and perhaps cemented femoral prosthesis would be a better choice. Furthermore, the measurements of the width of the medullary canal in this study and reported in literature are almost similar. This study determines different pattern of decrease or increase in size of the medullary canal in the two cohorts. Exact measurements for prosthesis replacement or intertrochanteric nail may be done on the patients for exact size and press fit.
Conclusions
This report revealed significant differences in the femoral medullary canal widths at the lesser trochanter (20%), supra-isthmus (35%) mid-isthmus (50%) and 80% length of the femoral bone among the American and East Asian populations; first three levels are significant points on the femur medullary canal length with respect to femoral prosthesis fixation. These findings underscore the importance of ethnic-specific considerations in orthopedic implant design and surgical planning, ultimately aiming to improve clinical outcomes in diverse patient populations. This data may be used to improve the design of femoral prosthesis in different east Asian populations. In particular for the East Asian population, the design should be according to their femoral geometry and should not be based on Caucasian femoral geometry which show differences.
Acknowledgments
We collaborators with the following universities, without their support this research would never have been completed. Prof. Akio Inoue from department of Orthopedic Surgery, Kurume University School of Medicine, Japan, Prof. T.K. Lui, Department of Orthopedic Surgery, National Taiwan University, Taiwan, Prof. Young-Min Kim, and Prof. Myung-Sang Moon, Department of Orthopedic Surgery, Seoul National University, and Catholic University Medical College, Korea, Prof. Xian-Zheng Luo, Department of Orthopedic Surgery, Beijing Friendship Hospital, China, Prof. Kerong Dai, Department of Orthopedic Surgery, Shanghai Second Medical University, China. We are also thankful to Dr. Zhenyu Wang and Dr. Ai Guo from China, Dr. Jinn Lin and Gau-Tan Lin from Taiwan, Dr. Young-Koo Kang from Korea and Dr. Naoto Shiba and Dr. Kenichiro Miyazaki from Japan.
We are also grateful for Ilka Lorenzen-Schmidt, Stephen Kraker and Veronika Bonin from Germany who were summer students and devoted their time to this project.
Conflict of Interest
The author(s) do not have any conflict of interest
Funding Sources
The author(s) received no financial support for the research, authorship, and/or publication of this article
Data Availability Statement
This statement does not apply to this article.
Ethics Statement
This research did not involve human participants, animal subjects, or any material that requires ethical approval.
Informed Consent Statement
This study did not involve human participants, and therefore, informed consent was not required.
Authors’ Contribution
Dr Najam Siddiqi: Wrote the proposal and identified the parameters to be measured on femur, visited China and Japan to collect the bones, took the radiographs, brought them back to the Biomechanics lab at Johns Hopkins University, and measured the femoral medullary canal by using a digitizer. Helped the IT people to develop the software for the digitizer and methodology to measure on the radiographs. The data was collected on a hard disc, analyzed, followed by writing the paper.
Prof. Edmond Chao: As the Director of the Biomechanics Lab, he wrote the initial proposal, developed a jig to hold the bone for taking radiographs of the femur, supervised the overall writing of this research project. He made collaborations with the hospitals and medical colleges in East Asian countries for collection of the femora, visited Korea and Taiwan and got the radiographs of the bones and brought them back to the Biomechanics lab at Johns Hopkins University. With the IT people, he developed a custom made software for measuring the bone parameters. He also supervised the data analysis.
References
- Lachiewicz PF, Soileau ES, Bryant P. Second-generation proximally coated titanium femoral component: minimum 7-year results. Clin Orthop Relat Res 2007; 465:117-21.
CrossRef - Engh CA, Bobyn JD, Glassman AH. Porous-coated hip replacement. The factors governing bone ingrowth, stress shielding, and clinical results. J Bone Joint Surg Br 1987; 69(1):45-55.
CrossRef - Vresilovic EJ, Hozack WJ, Rothman RH. Radiographic assessment of cementless femoral components. Correlation with intraoperative mechanical stability. J Arthroplasty 1994; 9(2):137-41.
CrossRef - Kim JT, Yoo JJ. Implant Design in Cementless Hip Arthroplasty Hip Pelvis. 2016; 28(2):65-75.
CrossRef - Darius M. Thiesen et al. A comparison between Asians and Caucasians in the dimensions of the femoral isthmus based on a 3D-CT analysis of 1189 adult femurs European J Trauma and Emergency Surgery 2022; 48: 2379-2386.
CrossRef - Noble PC, Alexander JW, Lindahl LJ, Yew DT, Granberry WM, Tullos HS. The anatomic basis of femoral component design. Clin Orthop Relat Res 1988; 235:148-65.
CrossRef - Hoaglund FT. Low WD. Anatomy of the Femoral Neck and Head, with Comparative Data from Caucasians and Hong Kong Chinese Clinical Orthopedics and Related Research 1980; 152: 10-16.
CrossRef - Kokubo Yasuo, Kenzo Uchida, Hisashi Oki, Kohei Negoro, Kouki Nagamune, Shogo Kawaguchi, Kenichi Takeno, Takafumi Yayama, Hideaki Nakajima, Daisuke Sugita, Ai Yoshida, Hisatoshi Baba. Modified Metaphyseal-Loading Anterolaterally Flared Anatomic Femoral Stem: Five- to Nine-Year Prospective Follow-Up Evaluation and Results of Three-Dimensional Finite Element Analysis Artificial organs 2012; 37: 175-182.
CrossRef - Kamath SU, Agarwal S, Austine J. Morphology of Proximal Femur in South-West Coast of India. Malays Orthop J 2020; 14(3):143-150.
CrossRef - Sen RK, Tripathy SK, Kumar R, Kumar A, Dhatt S, Dhillon MS, Nagi ON, Gulati M. Proximal femoral medullary canal diameters in Indians: correlation between anatomic, radiographic, and computed tomographic measurements. J Orthop Surg (Hong Kong). 2010; 8(2):189-94.
CrossRef - Siddiqi N, Valdevit, A. & Chao EYS. Differences in femoral morphology among the Orientals and Caucasians: a comparative study using plain radiographs. Anat Sci Int 2019; 94: 58–66.
CrossRef - Milligan DJ, O’Brien S, Bennett D, Hill JC, Beverland DE. The effects of age and gender on the diameter of the femoral canal in patients who undergo total hip replacement. Bone Joint J 2013; 95-B(3):339-42
CrossRef - Su XY, Zhao JX, Zhao Z, Zhang LC, Li C, Li JT, Zhou JF, Zhang LH, Tang PF. Three-Dimensional Analysis of the Characteristics of the Femoral Canal Isthmus: An Anatomical Study. Biomed Res Int 2015; 2015:459-612.
CrossRef - Lin Wang, Kaijin Guo, Hong Zhu, Kunjin He, Weizhong Geng. Morphological Analysis of Medullary Cavity for Designing Personalized Femoral Stem, Research Square, Research Square, 2021
CrossRef - Zhang Yang, Wang Jian, Li Zhi-han, Xiao Jun, Zhao Liang, Yang E, Shi Zhan-Jun. The geometry of the bone structure associated with total hip arthroplasty. PLoS ONE, 2014; 9(3): e91058.
CrossRef - Nitesh D Dhanekula, Gareth Crouch, Karen Byth, Sue Lynn Lau, Albert Kim, Edward Graham, Andrew Ellis, Roderick J Clifton Bligh, Christian M Girgis. Asian Ethnicity and Femoral Geometry in Atypical Femur Fractures: Independent or Interdependent Risk Factors? JBMR Plus, 6:2022, e10607.
CrossRef - Yasuto Nakanishi, Vincent Nethery, Anthropometric comparison between Japanese and Caucasian American male university students. Appl Human Sci 1999; 18: 9-11.
CrossRef - Rahmati Sadegh, Abbaszadeh Farid, Farahmand Farzam, An improved methodology for design of custom made hip prostheses to be fabricated using additive manufacturing technologies, Rapid prototyping journal 2012; 18:389 – 400.
CrossRef - Huiskes R, Van Rierbergen B. Preclinical testing of total hip stems: the effects of coating placement. Clin Orthop Relat Res 1995; 319:64-76.
CrossRef - Hua J, Walker P.S. Relative motion of hip stems under load. An in vitro study of symmetrical, asymmetrical, and custom asymmetrical designs. J Bone Joint Surg Am 1994; 76:95-103.
CrossRef - H.-J. Laine, M.U.K. Lehto, T. Moilanen, Diversity of proximal femoral medullary canal, The Journal of Arthroplasty, Volume 15, Issue 1, 2000, Pages 86-92,
CrossRef - Philippe Massin, Laurent Geais, Eric Astoin, Marc Simondi, François Lavaste, The anatomic basis for the concept of lateralized femoral stems: A frontal plane radiographic study of the proximal femur, The Journal of Arthroplasty, 2000; 15: 93-101.
CrossRef - Wang Y, Hu Y, Xu Z, Zhao Y, Wu J, An intramedullary nail with multifunctional interlocking for all types of fracture in both femurs, Orthopedic Surgery 2009;1: 121–126
CrossRef - Onoue, Y., Sunami, Y., Fujiwara, H. et al. Treatment of the femoral shaft fracture with a curved heat-treated COP clover-leaf nail. International Orthopaedics 1979; 3: 203–210.
CrossRef - Akihiko B, Shinichi I, Hironori O, Yasuhiro O, Masao A, Hisatoshi B, Patrick W, Al Z, Fit and fill analysis of a newly designed femoral stem in cementless total hip arthroplasty for patients with secondary osteoarthritis, Journal of Orthopedic Science, 1997; 2:301-312.
CrossRef - Khang G, Choi K, Kim CS, Yang JS, Bae TS. A study of Korean femoral geometry. Clinical Orthopedics and Related Research 2003; 406:116-122.
CrossRef - Pi Y, Zhao Y, Wang W, He Z, Mao X., Measurement of proximal femoral morphology and analysis of 500 cases in Hunan Province. Zhong Nan Da Xue Xue Bao Yi Xue Ban. 2013; 38:925-30.
- Tucker D, Surup T, Petersik A, Kelly M. Full circle: 3D femoral mapping demonstrates age-related changes that influence femoral implant positioning. Injury. 2015; 47:471-7.
CrossRef








