Azzam Alarab* , Ibrahim Salhab
, Ibrahim Salhab , Dana Darawy, Maram Abu Aker, Raneen Al Naji, and Nabil Hroub
, Dana Darawy, Maram Abu Aker, Raneen Al Naji, and Nabil Hroub
Department of Physiotherapy, Faculty of Allied Medical Health, Palestine Ahliya University, Bethlehem, Palestine
Corresponding Author E-mail: azzam@paluniv.edu.ps
DOI : https://dx.doi.org/10.13005/bpj/2927
Abstract
Background: Low back pain (LBP) is one of the main causes that affect mechanical function in human bodies worldwide, 90% of the cases with non-specific LBP. Different options are available for the management of non-specific LBP. While Maitland mobilization and core stability exercises are usually utilized in clinical practice for managing Chronic Nonspecific Low Back Pain, there is now a lack of research examining their comparative effectiveness. Objective: The objective of this study is to assess and compare the efficiency of Maitland mobilization and core stability exercise as treatment modalities for adults suffering from chronic non-specific low back pain. Methods: A total of 36 Non-specific low back pain (NSLBP) patients with ages 18 to 45 years were inducted and given their Informed consent. Subjects were allocated into two groups through simple random sampling. Group A (N=18) received central posterior-anterior vertebral mobilization while group B (N=18) received core stability exercises. Pain and functional disability were assessed using the Visual Analogue scale (VAS) and Oswestry Disability Index (ODI) respectively. Pre & post-treatment scores were documented and compared to achieve the aim of this study. Results: T-test indicated that the results pre- and post-treatment were showed a statistically positive significant difference by applying Maitland mobilization technique with non-specific LBP to improve functional disability (ODI) and reduce pain intensity (VAS) with (p = 0.001), respectively. On the other hand, results for the application of core stability exercises in management NSLBP also showed positive signs in reducing VAS and improving ODI with (p= 0.001) respectively. The findings suggest that there was no statistically significant difference between the Maitland mobilization technique and core stability exercises in treating NSLBP for pain reduction with (p = 0.312) and improvement in ODI with (p = 0.055). For applying Maitland mobilization in NSLBP, Pearson correlation results indicated that there was no relationship between body mass index (KG/M2) and functional disability (ODI) with (p = 0.034) and pain severity (VAS) with (p = 0.808). For core stability exercises, the results of Pearson's correlation indicated that there was no relationship between body mass index (KG/M2) and functional disability (ODI) with (p = 0.959) and pain intensity (VAS) with (p = 0.987). By gender, the results showed there were no statistically significant role for Maitland mobilization and core stability exercises in improving function and reducing pain among patients with chronic non-specific low back pain. Conclusion: Both core stability exercises and Maitland method have demonstrated effectiveness in reducing pain and improving functional disability in patients with chronic nonspecific low back pain.
Keywords
Chronic nonspecific LBP; core stability exercises; Maitland mobilization; Oswestry disability index
Download this article as:| Copy the following to cite this article: Alarab A, Salhab I, Darawy D, Abu-Aker M, Al-Naji R, Hroub N. Maitland Mobilization Versus Core Stability Exercises in Management Chronic Nonspecific LBP. Biomed Pharmacol J 2024;17(2). |
| Copy the following to cite this URL: Alarab A, Salhab I, Darawy D, Abu-Aker M, Al-Naji R, Hroub N. Maitland Mobilization Versus Core Stability Exercises in Management Chronic Nonspecific LBP. Biomed Pharmacol J 2024;17(2). Available from: https://bit.ly/3RGUBhU |
Introduction
low back pain (LBP) is defined as pain below the costal margin and above the inferior gluteal folds with or without radiating to the leg. Chronic Nonspecific Low Back Pain is a highly widespread condition across the globe and is a leading cause of work-related impairment 1,2. It affects a significant portion of the population, with a prevalence rate of up to 70% among individuals aged 35-55 years old 1.
Low back pain (LBP) is normally categorized based on the duration of pain, which includes acute (lasting less than 6 weeks), sub-acute (lasting 6 to 12 weeks), or chronic (lasting more than 12 weeks). LBP can also be classified as specific pain, caused by identifiable pathophysiological mechanisms originating from either non-spinal or spinal sources, or nonspecific back pain without a clearly identifiable reason. Nonspecific back pain may arise from the complex interplay of biological, psychological, and social factors. It is important to note that nonspecific back pain accounts for approximately 80 to 90% of all reported cases of low back pain2.
Different treatment strategies are used to manage LBP including oral medications, Injection therapy at the lumbar region, surgery, Physical Therapy, Chiropractic and psychotherapy, and so on, in the case of physical therapy, active physical therapy management with an emphasis on exercise as a key component in the treatment of chronic LBP3.
Physical activity has a positive effect in reducing NSLBP. Using therapeutic exercises to energize and strengthen the core is named core stability exercises (CSE). CSE is an effective treatment for all CLBP patients (specific and non-specific) in improving pain, and disability4,
They are effective methods for treating pain for Chronic NSLBP patients5, and CSE is more effective than routine physiotherapy in terms of achieving a greater reduction in pain intensity with chronic NSLBP6, it provides a significant difference in improving endurance, function and reduction of pain compared to conventional exercise7. Also, CSE has a significant effect on the reduction of functional disability in patients with chronic LBP8. Furthermore, when it is compared to conventional physical therapy, it is significantly better in decreasing functional disability in chronic NSLP9.
On the other hand, Maitland mobilization is a manual technique that involves gentle and deliberate mobilization of the spinal joints, performed within the patient’s comfortable range of motion. The foundation of this approach lies in the understanding of the biomechanical and neurophysiological mechanisms, with a specific focus on enhancing joint motion. By improving the range of motion, reducing muscle spasms, and alleviating pain, this approach aims to address these aspects 3.
Maitland mobilization has a strong effect on reducing pain and disability in patients with LBP 1. It considers an alternative treatment for pain among patients with chronic NSLBP10.
PA mobilization was effective in reducing pain and improving function compared to thermotherapy in patients with NSLBP11. Also, PA mobilization resulted in a significant reduction of pain and functional disability compared with McKenzie press-up exercise in patients with NSLB12.
According to the literature, CSE showed no significant difference for chronic NSLBP versus manual therapy in general13, and even though Maitland mobilization combined with core stability exercise had a significant effect in improving functional disability in chronic LBP than conventional physical therapy protocol3, no study has been conducted yet to compare between PA mobilization and CSE in patients with chronic NSLP.
Thus, the current study aims to compare Maitland mobilization and core stability exercise in the management of pain and disability among adult patients with chronic NSLBP.
Methods and Materials
There are several methods of treating NSLBP. However, all the used methods vary among themselves in their effectiveness of treatment for this case. There is also a contradiction in some studies about the method of treating NSLBP as the final way, and this is what was previously clarified in the literature.
Study design
A random experimental study was carried out at the physiotherapy center at Palestine Ahliya University in West Bank from December 2022 to January 2022.
Population, Sample, and Subjects
Target population
All patients referred to the out-patient physiotherapy department at the Physiotherapy center at PAU, who are diagnosed with NSLBP by an orthopedic physician until NOV.2022.
Source population
Medical records of the orthopedic department at Health Care Center in West Bank
Sample population
A random sample of patients who are diagnosed with NSLBP and referred to physiotherapy.
Inclusion criteria
(A) Females and males with age 18-45 years. (B) LBP due to Nonspecific pathology. (C) The onset of LBP is more than 3 months. (D) Localized Pain with functional activities of daily living.
Exclusion criteria
(A) Individuals experiencing neurological deficits in their lower limbs, characterized by reduced muscle strength in specific muscle groups (myotomes) or diminished sensation in specific areas of the skin (dermatomes). (B) Individuals with systemic diseases or neurological disorders. (C) Any clinical condition that presents contraindications to mobilization. (D) Individuals with a history of spinal surgery or those who have received epidural injections. (F) Participants who have undergone physical therapy treatment for low back pain within the past six months.
Sampling method
Probability Simple randomized sampling was used in which patients were randomly distributed into two groups. An offsite randomization schedule to ensure allocation protection was used through by computer software program that generates the random sequence, it was generated a random allocation sequence to each group. Group A (Maitland mobilization): 18 patients were given 3 sessions per week for 2 weeks, and one mobilization technique was applied for 10 minutes. Group B (Core stability exercises): 18 patients were given 3 sessions per week for 2 weeks, and 4 core stability exercises were applied for almost 20 to 25 minutes, each exercise should be finished within 3 to 5 minutes, and 20 repetitions for each one with different holding periods for each exercise. A 2–3-minute break between each exercise is recommended.
Study Setting
The assessment of eligibility criteria, obtaining written informed consent, collecting data, and conducting statistical analysis were performed by researcher #1, who would be unaware of the group allocation. Participants were received both oral and written instructions regarding the potential risks and benefits of the research and provided written approval.
The eligible participants who provided written approval were randomly assigned to either the Maitland group or the core stability exercises group. The randomization schedule was prepared by an independent researcher who had no contact with the participants and was not involved in the recruitment, screening, assessment, enrollment, or treatment process. An independent physiotherapist #3, who was also unaware of the group allocation, conducted all Visual Analog Scale (VAS) and Oswestry Disability Index (ODI) assessments before treatment and after a 2-week period. To ensure the neutrality of the researchers, patients were instructed not to disclose their group affiliation before each evaluation. Additionally, all personal data was kept confidential by coding participants’ names before, during, and after the study. Another independent physiotherapy #4 was carried out for two groups.
Data collection
All patients with chronic NS-LBP will be referred by the orthopedic specialist to screen the study eligibility according to the inclusion and exclusion criteria. The physiotherapists who treat patients with chronic NS-LBP will use a standardized evaluation form that consists of a patient interview history, physical evaluation, and clinical notes history. The whole study will be explained to the participating patients. The study included 36 different patients complaining of Chronic NS-LBP to investigate the effectiveness of Maitland mobilization and core stability exercises in treating pain and improving disability among adult patients with Chronic NS-LBP. Patients were divided into two groups randomly, each group consisted 18 patients. The first group was treated with Maitland mobilization, while the second group was given core stability exercises. Both the Visual analogue scale (VAS) to assess pain and Oswestry Disability Index (ODI) to measure low back functional disability. It was used in both groups before and after 8 sessions, and then the results regarding pain and functional disability before and after between both groups were compared.
Instrumentation
Demographic data was collected for each patient, and individual evaluations were conducted. The Visual Analogue Scale (VAS) was utilized as a reliable and valid measurement of pain intensity experienced by individuals. This scale is sensitive to clinical changes in pain and ranges from 0 (indicating no pain) to 10 (representing the worst imaginable pain). Patients were asked to select the point on the scale that best correlated with their pain intensity14. Additionally, the Oswestry Low Back Pain Disability Index (ODI) was employed. This questionnaire consists of 60 items and assesses pain-related limitations across 10 domains: Pain Intensity, Personal Care, Lifting, Walking, Sitting, Standing, Sleeping, Sex Life, Social Life, and Traveling. Within each domain, patients were asked to indicate which of the six statements applied to them, with scores ranging from 0 (no impairment) to 5 (maximum impairment). The scores for each domain were summed and multiplied by 2 to yield a Disability Index Score percent15. In cases where participants did not complete all items, the score was pro-rated by averaging the completed items and multiplying by 10. The ODI was used to assess functional performance.
Interventions
Central P/A mobilization
Posterior-to-anterior (PA) mobilization technique is a cornerstone of Maitland vertebral mobilization. It can be defined as a passive oscillatory movement9. It can be used to treat pain distributed to both sides of the lumbar spine with careful and comprehensive examination before the application of the technique12.
When applying this technique, the patient should be relaxed and comfortable in a prone position with a pillow under the abdomen, the therapist should stand close to the patient, and the therapist’s sternum should be perpendicular to the selected mobilization segment when performing the technique. The Therapist should apply central PA pressure to the spinous process of each lumbar vertebra using small amplitude movements (grade I)12.
During the mobilization process, it is important to apply pressure that re-produces the discomfort felt while bending backward in a standing position. If grade 1 mobilization does not elicit any pain, higher grades (II-IV) will be utilized. After assessing each lumbar vertebra, the most painful segment will be treated with graded central PA oscillations. This involves applying three sets of 40-second oscillations to the segment, using an amplitude that the patient can tolerate. The therapist will then reassess the patient’s pain before moving on to treat another lumbar vertebra. Grade IV mobilization will be applied at the end range of stiffness segment, ensuring that the pain remains tolerable. The entire PA mobilization intervention typically takes approximately 10 minutes12.
 |
Figure 1: Central P/A mobilization |
Core stability exercise
Abdominal tightening exercise
The patient is asked to bring both hips together to feel the contraction of lower abdominal muscles, Patients will be asked to hold the position for 20 seconds, then return to the starting position .20 repetitions are needed 16.
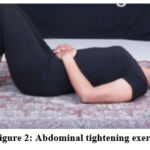 |
Figure 2: Abdominal tightening exercise |
Pelvic tilt exercises
This exercise will be done by keeping both hands behind the buttocks and pressing on them by flattening the spine and bending the pelvis up slightly, then holding for up to 10 seconds with 20 times of repetitions 16
 |
Figure 3: Pelvic tilt exercise |
Partial curl
The patient will be in a supine position with knee bent and arms behind the head, the feet slightly away from the buttocks, then patient raise the upper body from the ground approximately 30 to 40 degrees, the abdominal muscles begin to contract, then the upper body will be lower to the ground again, the whole movement approximately takes 3 to 4 seconds. It should be repeated 20 times 16.
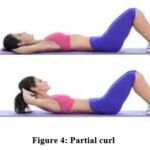 |
Figure 4: Partial curl |
Back extension exercise
The patient needs to lie in a prone position on a mat with legs straightening with a pronated forearm, then lift the upper back. Hips should be pressed into the mat with the head and neck in a neutral position. The patient should hold this position for 30 seconds, then lower again to starting position and repeat the exercise for 20 sets 16.
 |
Figure 5: Back extension exercise |
Statistical analysis
Following the collection of study data, the researchers conducted a thorough review in preparation for computer entry. The data was accurately entered into the computer system, utilizing specific numerical values. Statistical processing of the data involved extracting numbers and percentages. The hypotheses were examined at a significance level of α = 0.05, employing statistical tests such as the T-test and Pearson correlation. The computer software used for these analyses was the Statistical Package for the Social Sciences (SPSS).
Results
In the present study, a total of 36 subjects (16 males and 20 females) were selected to investigate the effectiveness of Maitland mobilization and core stability exercises in reducing pain intensity and improving functional disability in individuals with chronic nonspecific low back pain. These subjects were randomly assigned to two groups; Group A (consisting of 18 participants) and Group B (also consisting of 18 participants).
The findings showed significant differences in the effect of mobilization technique in the treatment of nonspecific LBP at α=0.05 for the level of Amount of functional disability (ODI) and decrease pain intensity (VAS) respectively. The differences in favor of the post-group with a mean (23.67), inverses of the pre-group with a mean (50.02), and the results indicated that there were significant differences at α=0.05 for the level of severity of pain (VAS). The differences in favor of the post-group with a mean (2.38), inverses of the pre-group with a mean (6.88). It means the Maitland mobilization technique has an effect on improving function and reducing pain for CNSLBP. These results are presented in Table 1.
Table 1: Effect of Maitland mobilization on VAS and ODI.
|
Mean |
Std. Deviation |
DF |
T |
Sig |
||
|
Amount of functional disability (ODI) |
Pre treatment |
50.02 |
6.33 |
14 |
9.609 |
0.001 |
|
Post Treatment |
23.67 |
4.47 |
||||
|
Severity of pain (VAS) |
Pre treatment |
6.88 |
0.99 |
14 |
8.768 |
0.001 |
The results showed significant differences in the effect of core stability exercises in the treatment of nonspecific LBP at α=0.05 for the level of Amount of functional disability (ODI) and decrease pain intensity (VAS) respectively. These differences are in favor of the post-group with a mean (16.2), inverses of the pre-group with a mean (51.5) and also the results indicated that there were significant differences at α=0.05 for the level of Severity of pain (VAS). The differences are in favor of the post-group with a mean (1.88), inverses of the pre-group with a mean (6.13). It means that the core stability exercises have a good effect on improving function and decreasing pain intensity for chronic nonspecific LBP. These findings are shown in Table 2.
Table 2: Impact of core stability exercises on VAS and ODI.
|
|
Mean |
Std. Deviation |
DF |
T |
Sig |
|
|
Amount of functional disability (ODI) |
Pre treatment |
51.5 |
17.0 |
14 |
5.220 |
0.001 |
|
Post Treatment |
16.2 |
8.64 |
||||
|
Severity of pain (VAS) |
Pre treatment |
6.13 |
1.35 |
14 |
7.549 |
0.001 |
|
Post Treatment |
1.88 |
0.83 |
||||
The results indicated that there were no significant differences at α=0.05 for the level of the Maitland mobilization and core stability exercises in decreasing pain and improving functional disability among patients with chronic nonspecific low back pain. This finding is shown in Table3.
Table 3: Maitland mobilization versus core stability exercises on VAS and ODI
|
Group |
Mean |
Std. Deviation |
DF |
T |
Sig |
|
|
Amount of functional disability (ODI) |
Therapeutic exercise (A) |
16.25 |
8.64 |
14 |
-2.157 |
0.055 |
|
Maitland mobilization (B) |
23.67 |
4.47 |
||||
|
Severity of pain (VAS) |
Therapeutic exercise (A) |
1.88 |
.83 |
14 |
-1.048 |
0.312 |
|
Maitland mobilization |
2.38 |
1.06 |
The Pearson correlation was used for the relationship between BMI (KG/ M2) Amount of functional disability (ODI), and Severity of pain (VAS) with Maitland mobilization. There was no relationship at α=0.05 between BMI (KG/ M2), Amount of functional disability (ODI), and Severity of pain (VAS) with Maitland mobilization. These results are shown in Table 4.
Table 4: Pearson correlation between BMI (KG/ M2) and Amount of functional disability (ODI), Severity of pain (VAS) with Maitland mobilization.
|
Maitland mobilization |
Pearson Correlation |
Sig |
|
BMI (KG/ M2) * functional disability (ODI) |
0.744* |
0.034 |
|
BMI (KG/ M2) * Severity of pain (VAS) |
0.103 |
0.808 |
It used Pearson correlation for the relationship between BMI (KG/ M2) and the amount of functional disability (ODI), The severity of pain (VAS) with core stability exercises. There was no relationship at α=0.05 between BMI (KG/ M2) and Amount of functional disability (ODI), Severity of pain (VAS) with core stability exercises. These results are presented in Table 5.
Table 5: Pearson correlation between BMI (KG/ M2) and Amount of functional disability (ODI), Severity of pain (VAS) with core stability exercises.
|
Core stability exercises |
Pearson Correlation |
Sig |
|
BMI (KG/ M2) * functional disability (ODI) |
0.022 |
0.959 |
|
BMI (KG/ M2) * Severity of pain (VAS) |
0.007 |
0.987 |
Discussion
LBP is one of the most common public health problems. NSLBP is low back pain without underlying specific causes and symptoms lasting over 12 weeks 4.
A pilot RCT was conducted to evaluate the effectiveness of Maitland manual mobilization versus core stability exercise in decreasing VAS and improving ODI with chronic NSLBP. Current study consisted 36 patients with chronic NSLBP.
The age of the group of participants was in the range of 18 to 45 years old with no serious pathology or any contraindication for the interventions, participants above 45 years old had not been included in the study as they might experience low back pain due to degenerative changes in the lumbar spine 12.
In this study, Pre &post analysis for VAS and ODI scores in the first group treated by Maitland mobilization and the second group treated by core stability exercises showed significant differences at the end of the sixth treatment sessions during two weeks, but there was no significant difference when comparing the effect of each intervention to each other.
There is no study yet comparing Maitland mobilization and core stability exercises as the best choice of intervention in treating chronic NSLBP among adult patients, but, Elbayomy, & Koura13 conducted a systematic review study regarding the effectiveness of Core strengthening for chronic NSLBP indicating that there was no clinically significant difference between core strengthening exercises and manual therapy in general13 . On the other hand, de Mèlo and his friends17 demonstrated an RCT study about using Maitland mobilization in improving pain and functionality in chronic lumbar pain of young adults, suggesting that patients who were treated with therapeutic exercises had a significant improvement over 6 weeks (p= 0.026) and 12 weeks (p= 0.018) post-treatment in Roland Morris Questionnaire (RMQ), that used to assess pain-related disability resulting from Lapthe same thing was observed in VAS score in relation to 6 weeks of follow-up (p= 0.018), and 12 weeks post-treatment (p= 0.017), while patients treated with Maitland mobilization has a constant result regarding VAS and RMQ throughout the treatment.
The compression in the previous study was between Maitland mobilization and general exercises, and not with specific core stability exercises. However, it investigated that the exercises had a superior effect on Maitland mobilization regarding the decreasing of pain and improving function in patients with CNSLBP, which doesn’t support our study result of having no significant effect between the Maitland mobilization and core stability exercises in relation of pain and functional disability.
Some factors may have influenced the previous findings including the higher BMI in the Maitland group, another thing that patients in this group reported mild pain according to VAS before the treatment (VAS <4), and they finished treatment without pain. However, the means to be considered to improve pain in VAS, the individual’s final score compared to the initial score should have a difference greater than 3.5, and therefore, the lower value was not clinically significant for VAS.
In the case of BMI, another contributing factor that might also affect the current study finding regarding no significant effect in ODI score between the Maitland technique and core stability exercises. There was a positive relationship between BMI (KG/ M2) and functional disability (ODI) (P value < 0.034) in the Maitland group, while there was no positive relationship in the core stability exercises ‘group, and whenever the score of the BMI increased in patients with chronic LBP, and the score of functional disability increased 18. Therefore, it’s important to maintain the body weight within the recommended range to reduce the risk of functional disability and mortality 19. However, the was no major contributing factor affecting the result of an average of pain as the VAS score in the Maitland group had shown no significant difference compared to the pain score in the core stability exercises. We should accept the issue that both treatments have great benefits, this is mentioned in the following paragraphs when comparing the impact of each treatment on the pain severity and function with the results of previous studies. Otherwise, preferring one technique over another one a matter should be addressed when following up the study with a larger sample and for a longer treatment period.
Corresobendically, The study’s findings of reduction in pain intensity and improvement in functional disability with the application of Maitland mobilization, are consistent with the findings of an RCT study reported by Shah, & Kage12 indicated that Posterior anterior mobilization (PA) provides a significant reduction in the average of pain severity, It was also measured with VAS scale and disability functional scores as measured by ODI scale compared with Mackenzie press up exercise in patients with NSLBP (P <0.05)
The current study results including the effectiveness of Maitland mobilization in minimizing pain and improving functional disability are also consistent with the findings of another RCT study demonstrated by Baig and his friends 11 determined that PA mobilization had a significant effect in alleviating pain and improving function compared to thermotherapy in participants complaining of NSLBP.
Moreover, a systematic review study demonstrated by Outeda and his colleagues1 about the impact of the Maitland techniques on LBP, suggested that there is an evidence that the manipulations and mobilizations described in the Maitland Concept reduce pain and disability in people with LBP when applied alone or in combination with other interventions. Those results were agreeing with our study’s findings, suggesting that Maitland mobilization provides a post-treatment significant reduction in VAS and ODI scores compared to treatment.
Maitland mobilization was shown to be significantly effective in reducing pain in patients with CLBD20, Phelan and his friends 10 supported the use of Maitland Spinal Mobilization as an effective method providing a significant difference in reducing pain in 90 patients complaining of NSLBP after four weeks of follow-up, three times per week. This finding indicated that manual therapy could be considered a preferable alternative intervention to conventional physiotherapy treatment in the management of NSLBP, which reinforced the current study’s result regarding the effectiveness of Maitland mobilization in minimizing the patients’ pain.
Meanwhile, The current study’s findings of reduction in pain intensity and improvement in functional disability with the application of core stability exercise, are also correlated with the results of a systematic review study accomplished by Frizziero and his colleagues4 suggested that core stability is an effective rehabilitation strategy for all CLBP patients (specific and non-specific) in improving pain, and disability regardless the duration of symptoms.
In terms of pain as a dependent outcome that is considered in the present study result, it is constant with the previous studies’ results that supported the application of core stability exercises in the management of pain in patients with NSLBP. Smrcina and his friends 4 demonstrated a systematic review study clarifying that core stabilization exercises can be considered a favorable method for treating pain in patients with chronic NSLBP and Salik Sengul and his friends7 accomplished an RCT study, signifying that Core stability exercises had been considered superior to conventional physiotherapy treatment, it offered a significant difference in improving pain during activity, endurance, and function (p < 0.05) compared to conventional exercise in patients with chronic NSLBP. Likewise, the therapeutic effects of core stabilization exercise program over six weeks are more effective in reducing pain, compared to routine physical therapy exercise in patients with chronic NSLBP(6).
In terms of functional disability, it is another dependent outcome sure being investigated in the present study result, it has a consistency with the previous studies that supported the use of core stability exercises in improving functional disability with chronic NSLBP. Kapetanovic and his colleagues 8 completed an RCT study, clarifying that patients with chronic LBP (without serious spinal pathology or specific diseases, with no signs of damage to the nerve roots) who performed the core stabilization exercises of three or five times a week had a significant difference in ODI score before and after two months of rehabilitation (p = 0.0001) corresponded to patients did not perform the exercises. Waseem and his friends(9) investigated an RCT study, indicating that the first group of patients with chronic NSLBP who were treated with core stability exercises and the second group of patients treated by routine physical therapy had a significant reduction in disability as measured by ODI at the end of the second, fourth, and sixth week of treatment (p < 0.05)., but there was a large reduction in disability being observed for patients (9).Maitland mobilization combined with core stability exercise was well understood in an RCT study conducted by Ahmed and his friends, which investigated that Maitland manual therapy combined with core stability exercise had a significant effect in reducing the disability related to Chronic LBP than conventional physical therapy protocol (p < 0.05).
LBP is a serious healthcare problem and was ranked as the greatest contributor to global disability4. Even though there is no significant difference in using Maitland mobilization as the best choice of treatment for pain and functional disability in patients with NSLBP compared to core stability exercises, there is a positive significant effect for each treatment technique in reducing pain and improving functional disability among patients with NSLBP. Thus, using both physiotherapy interventions or one of them will provide optimal benefits and greater treatment outcomes at low cost for physiotherapists and patients in the community.
Limitations
Several limitations of this study need to be addressed. The participants have followed up for only two weeks, and it should be a longer period to investigate the constant improvement due to both interventions. The study findings could only be generalized for only non-specific low back pain and not all patients with low back pain. These limitations need to be handled in future investigation.
Conclusion
This the first RCT study compared between PA mobilization and CSE in adult patients with chronic NSLBP, it concluded that the comparison between Maitland mobilization group and CSE group revealed no statistically significant differences regarding VAS and ODI. However, both treatments are effective for the alleviating pain and for the evolution of function among patients with chronic NSLBP.
It is important to continue this study, which will allow more participants with long term to follow up, and therefore to achieve greater results to verify which technique is an effective treatment. Also, it is necessary to investigate more RCT studies with further outcome measures to generalize results to have more accurate reliable and validated applicable results useful in the clinical settings.
Acknowledgement
I would like to express my sincere gratitude to all those who have contributed to the completion of this project. I would like to thank my supervisors for their guidance, support, and valuable insights throughout the research process. Their expertise and encouragement have been instrumental in shaping the direction of this study. Furthermore, I would like to extend my appreciation to the research team members who have contributed their time and effort to this project. Their collaboration and dedication have been invaluable in ensuring the smooth progress of the study.
Conflict of interest
No any conflict of the interest
Funding source
This research was conducted without any external funding sources.
References
- Outeda L. R, Cousiño L. A. J, Carrera I. D. C and caeiro E. M. L. Effect of the maitland concept techniques on low back pain: a systematic review. Coluna/Columna. 2022; Vol. 21(2).
CrossRef - Chiarotto A and Koes B. W. Nonspecific Low Back Pain. New England Journal of Medicine. 2022; 386(18), 1732-1740.
CrossRef - Ahmed F, Rahman M. U, Ullah K and Bhutta A. H. Combination of Core Stability Exercises and Maitland Manual Therapy is Better Alternative in the Management of Chronic Low Back Pain. Journal Riphah College of Rehabilitation Sciences.2020; 8(01), S24-S28.
CrossRef - Frizziero A, Pellizzon G, Vittadini F, Bigliardi D and Costantino C. Efficacy of core stability in non-specific chronic low back pain. Journal of functional morphology and kinesiology.2021; 6(2), 37.
CrossRef - Smrcina Z, Woelfel S and Burcal C. A Systematic Review of the Effectiveness of Core Stability Exercises in Patients with Non-Specific Low Back Pain. International Journal of Sports Physical Therapy. 2022; 17(5), 766.
CrossRef - Akhtar M. W, Karimi H and Gilani S. A. Effectiveness of core stabilization exercises and routine exercise therapy in management of pain in chronic non-specific low back pain: A randomized controlled clinical trial. Pakistan journal of medical sciences.2017; 33(4), 1002.
CrossRef - Salik S. Y, Yilmaz A, Kirmizi M, Kahraman T, and Kalemci O. Effects of stabilization exercises on disability, pain and core stability in patients with non-specific low back pain: A randomized controlled trial. Work, (Preprint).2021; 1-9.
- Kapetanovic A, Jerkovic S and Avdic D. Effect of core stabilization exercises on functional disability in patients with chronic low back pain. Journal of health sciences.2016; 6(1), 59-66.
CrossRef - Waseem M, Karimi H, Gilani S. A and Hassan Treatment of disability associated with chronic non-specific low back pain using core stabilization exercises in Pakistani population. Journal of Back and Musculoskeletal Rehabilitation.2019; 32(1), 149-154.
CrossRef - Phelan A, Phelan K and Foley M. Effectiveness of Maitland Spinal Mobilization Therapy in the Treatment of Non-Specific Low Back Pain – a prospective study of clients attending a single treatment center in the Republic of Ireland. Phys Ther Rehabil. 2020; 7:7.
CrossRef - Baig A. A. M, Ahmed S. I, Ali S. S, Rahmani A and Siddiqui F. Role of posterior-anterior vertebral mobilization versus thermotherapy in non-specific lower back pain. Pakistan Journal of Medical Sciences.2018; 34(2), 435.
CrossRef - Shah S. G and Kage V. Effect of seven sessions of posterior-to-anterior spinal mobilization versus prone press-ups in non-specific low back pain–randomized clinical trial. Journal of clinical and diagnostic research: JCDR.2016; 10(3), YC10.
CrossRef - Elbayomy M. A, Zaki L. A and Koura G. Core strengthening for chronic nonspecific low back pain: systematic review. Bioscience Research. 2018 15(4), 4506-19.
- Alarab A and Unver F. Stretching Exercise Versus Tissue Mobilization Technique in Piriformis Syndrome. European Journal of Medical and Health Sciences.2020; 2(6).
CrossRef - Wang Y. C, Lehman L. and Yen S. C. Comparison of a modified Oswestry low back pain disability questionnaire and the Oswestry disability index. Archives of Physical Medicine and Rehabilitation.2018; 99(10), e25.
CrossRef - Majeed A. S, TS A and Sugunan, A. The effectiveness of a simplified core stabilization program (TRICCS—Trivandrum Community-based Core Stabilization) for community-based intervention in chronic non-specific low back pain. Journal of orthopedic surgery and research.2019; 14(1), 1-8.
CrossRef - de Mèlo L. C, de Mendonça H. C. S, de Amorim Cabral K. D, Rodrigues F. T. M, do Nascimento L. S. G, Guerino M. R and de Araújo M. D. G. R. Maitland in chronic lumbar pain of young adults improves pain and functionality. Manual Therapy, Posturology& Rehabilitation Journal.2017; 1-7.
- Teck T. S, Prabowo T and Kurniani N. Correlation between body mass index and disability in patient with chronic low back pain. Althea Medical Journal.2016; 3(4), 624-648.
CrossRef - Tabara Y. Nakatani E and Miyachi Y. Body mass index, functional disability and all‐cause mortality in 330 000 older adults: The S hizuoka study. Geriatrics & Gerontology International.2021; 21(11), 1040-1046.
CrossRef - Samir, S. M, Zak Y. L. A and Soliman M. O. Mulligan versus Maitland mobilizations in patients with chronic low back dysfunction. Int J Pharm Tech Res.2016; 9(6), 92-99.








