Hemalathaa R1* , Suryapriya R1
, Suryapriya R1 , Divya N2
, Divya N2 , Keerthika E1
, Keerthika E1 , Tamil Selvi B3
, Tamil Selvi B3 , N Ananthi1
, N Ananthi1  and C S Brethis4
and C S Brethis4
1Department of Biochemistry, Saveetha Medical College, SIMATS, Thandalam, India.
2Department of Opthalmology, Saveetha Medical College, SIMATS, Thandalam, India
3Biomedical Science, Saveetha Medical College, SIMATS, Thandalam, India
4Department of Pharmacology, ACS Medical College, Chennai, India
Corresponding Author E-mail:hemalathaaramar@gmail.com
DOI : https://dx.doi.org/10.13005/bpj/2938
Abstract
Background: Night shift work is associated with several long-term health complications including metabolic syndrome and cardiovascular disease along with various adverse health effects. This study was planned and conducted to learn the impact of Interleukin-6 (IL-6), a chronic inflammatory cytokine among day and night shift health care workers, and to correlate the relationship between the serum and tear fluid IL 6. Aim and Objective: To correlate the relationship between serum and tear fluid Interleukin-6 (IL-6) in day and night shift healthcare workers at a tertiary care hospital. Materials and Methods: This is a Cross-Sectional study with 100 (fifty-day shift and fifty-night shift) participants including medical, paramedical students, and lab technicians. Blood and tear samples were collected from both groups. SPSS version 26.0 was used to analyze the data using Pearson’s correlation, chi-square test, and ROC. An Independent student’s t-test was used to examine the differences between the mean scores. p-value < 0.05 is considered significant. Results: Serum and tear IL-6 levels were significantly increased in night shift workers when compared to day shift workers with p-value < 0.0001. There was a positive correlation between tear and serum IL-6 levels (r value 0.732 and 0.624) among day and night shift workers respectively. A high prevalence of dry eye syndrome in night shift workers (40%) when compared to day shift workers (14%). In ROC analysis, tear IL-6 shows the highest area under the curve (0.935) compared to serum IL-6 (0.883) which reveals the superiority of tear fluid analysis and suggests that tear fluid can be used as a minimally invasive technique to analyze IL-6 alternative to serum IL-6 analysis. Conclusion: This study concludes that tear and serum Interleukin-6 (IL-6) is proportionately increased in night shift workers compared to day shift workers with a positive correlation. It also suggests that tear fluid can be used as a minimally invasive technique and a superior method to analyze IL-6.
Keywords
Chronic stress; Dry eye syndrome; Serum Interleukin-6; Shift work; Tear fluid Interleukin-6
Download this article as:| Copy the following to cite this article: Hemalathaa R, Suryapriya R, Divya N, Keerthika E, Selvi B. T, Ananthi N, Brethis C. S. Correlation Between Serum and Tear Fluid Interleukin 6 Levels in Day and Night Shift Health Care Workers. Biomed Pharmacol J 2024;17(2). |
| Copy the following to cite this URL: Hemalathaa R, Suryapriya R, Divya N, Keerthika E, Selvi B. T, Ananthi N, Brethis C. S. Correlation Between Serum and Tear Fluid Interleukin 6 Levels in Day and Night Shift Health Care Workers. Biomed Pharmacol J 2024;17(2). Available from: https://bit.ly/3PTMIVw |
Introduction
Working hours apart from 7.00 am to 6:00 pm is known as night shift work.1 Due to increased competition, business demands, and technological change in the modern world,2 shift work among working adults has become more common place.3,4 Many studies have suggested that both the short duration of sleep (< 5 hours at night),5 and a night of disturbed sleep due to sleep apnea and narcolepsy are associated with increased levels of Interleukin-6 (IL-6) and other cytokines.6-8
From the expression of the gene behavior, every single function (variability in heart rate, brain waves, body temperature, energy expenditure, hormone secretion, physical performance, cognitive abilities, and sleep propensity) in the human body is under the control of the circadian system.9 The suprachiasmatic nuclei (SCN) of the hypothalamus 10 control the circadian rhythmicity of biochemical, psychological, and physiological parameters.11 There are several molecular mechanisms postulated underlying these intrinsic intracellular circadian oscillations.12 The genes controlled by the circadian clock are acknowledged as the molecular output of the circadian rhythm. They are exhibited as observable rhythms in behaviors, metabolic functions of cells, and tissues in the body.9 The internal clock in the human body is adjusted and is directly proportional to the changes in the environmental brightness which is responsible for the normal functioning of the vital organs through neuronal and hormonal signals.13Night shift work disrupts the normal circadian rhythmicity giving rise to concerns regarding health issues,14-16 as the adjustment to the environmental brightness by the internal clock is lost.17 The above theory states that night shift health care workers are at risk of various systemic diseases, including metabolic syndrome and cardiovascular disease (CVD) 18,19 due to the prolonged disturbance in the circadian rhythm such as a sleep-wake cycle which leads to a higher incidence of morbidity 6,20-22 like behavioral changes, consciousness level, high blood pressure,8 high blood cortisol, and melatonin levels.23
IL-6 plays a major role in the acute phase response as it is produced at the site of inflammation. IL-6 along with its receptor (soluble)SIL-6Rα transforms from acute inflammation to chronic inflammation by altering the leucocyte infiltrate i.e, from PMN (polymorphonuclear) neutrophils to macrophages/monocyte by stimulatory effects on B and T-cells. Strategies targeting IL-6 and its signaling led to effective screening, diagnosis, treatment, and prevention of chronic inflammatory diseases.24
The National Institute of Health (NIH) defines a biomarker as, “a character that is objectively measured and evaluated as an indicator of normal biological processes, pathogenic processes, or pharmacologic responses to a therapeutic intervention”.25 The US Food and Drug Administration (FDA) defines a biomarker as, “any measurable diagnostic indicator that is used to assess the risk or presence of disease”.26 The advancements have led, to tear fluid can be used as a minimally invasive technique for the analysis of many biomarkers in the investigation of PPPM – Predictive, Preventive, and Personalised medicine.27
Despite sleep disturbances, short sleep, and deranged circadian rhythm amongst night shift health care workers,28 there is a dearth of studies related to the correlation between shift work and chronic inflammatory cytokines and their sequelae. So, this study is planned to correlate the relationship between the serum and tear fluid IL-6 and to create awareness regarding the complications of chronic stress on night shift workers.
Materials and Methods
Study Design& Population
A Cross-sectional study was conducted at Saveetha Medical College and Hospital, Thandalam, Kanchipuram District, Tamil Nadu between September 2021 – April 2022 (8 months) after obtaining clearance from the Institute Scientific and Ethical Committee. Detailed information about the study was explained to the patients. Informed and written consent was obtained from the patients. Healthy workers without any comorbidities and body mass index (BMI) < 30 Kg/m2, both males and females between 20 – 40 years were included in the study. Chronic diseases like systemic hypertension (SHT), and DM, history of smoking, drugs (or) alcohol abuse, participants with eye makeup, sleep disorders, and body mass index (BMI) >30 Kg/m2 were excluded from the study. BMI was calculated as, weight (in kg) / square of height in meters.
Sampling Technique and Sample Size
Non-probability convenience sampling technique opted. This study included 100 healthcare workers (hospital technicians, staff, nurses, medical/ para-medical students, and interns) according to the inclusion and exclusion criteria. 50- dayshift healthcare workers working between 7.30 am to 4 pm and 50- night shift healthcare workers working between 7.30 pm to 7.30 am.
Blood collection
Approximately 3 ml of peripheral venous blood was collected in a red-topped vacutainer without anticoagulant from 50 participants enrolled in the day shift and 50 participants enrolled in the night shift. The sample was incubated at room temperature for 20 minutes for clot formation. The serum was separated after centrifugation at 3500 rpm for 5 minutes. 80 µl of serum was taken for IL-6 assay in VITROS 5600 by CLIA method. Normal serum IL-6 is <6.65 pg/mL (according to the kit insert received from ortho clinical diagnostics).
Tear fluid collection
Tear fluid is obtained using Schirmer strips without anesthesia. Schirmer strip is a small piece of filter paper with printed graduations. Strips are bent at the tip (on the zero line) to an angle of 120 degrees and placed at the lower palpebral conjunctiva. The patient is asked to close the eyes for 5 mins.29 5 minutes later the strip is removed by the examiner and the length of the strip wetted by tears is measured. The wetting of the Schirmer strip less than 15 mm without anesthesia indicates dry eye syndrome.30 The moistened part of the Schirmer strip is cut and placed inside a 1.5 ml Eppendorf tube. 0.9% sodium chloride (NaCl), proportional to the volume of tear fluid collected is added along the soaked part of the Schirmer’s strip and incubated for 2 hours (if the distance soaked in the Schirmer’s strip is 10 mm, then the amount of tear secreted is 10 µl. To 10 µl of tear fluid, 10 µl of 0.9% NaCl is added, mixed diluted and, incubated for 2 hours).29 The Eppendorf is then centrifuged at 13000 rpm for 3 minutes.31 80 µl of the tear fluid is taken for IL-6 assay in VITROS 5600 by CLIA method. The assayed value is multiplied using the dilution factor to get an accurate result. The normal reflex tear fluid IL-6 range is < 13.3pg/ml.32
Statistical Analysis and Results
All the results were statistically analyzed using SPSS version 26.0 software. Normally distributed continuous data is expressed as mean + standard deviation. p-value < 0.05 is considered significant. Pearson’s correlation was performed to correlate the relationship between the serum and tear fluid IL-6 in both day and night shift workers. A Chi-square analysis was done to calculate the prevalence of dry eye syndrome in both groups. ROC curve analysis to find out cut-off points of serum and Tear fluid IL-6.
Characteristics of Study Participants
The study included 100 participants (50-day and 50-night shift workers). The comparison of demographic variables, serum and tear IL-6 levels between day and night shift workers is shown in Table 1. The day and night shift workers did not differ significantly in age, height, weight, BMI, systolic blood pressure (SBP), diastolic blood pressure (DBP), pulse rate, and distance traveled by tears in Schirmer strips. Serum and tear IL-6 levels were significantly elevated in night shift workers when compared with day shift workers (Serum IL-6 22.7 ± 11.9 vs 6.7 ± 5.1, p< 0.0001; Tear IL-6 53.6 ± 49 vs 13.6 ± 12.8, p< 0.0001). The duration taken to moisten 15 mm of Schirmer strips was significantly higher in night shift workers when compared with day shift workers (3.2 ± 1.4 vs 1.7 ± 1.3, p< 0.0001).
Table 1: Comparison of Demographic Variables and IL-6 Levels Between Day & Night Shift Workers
|
Variables |
Day shift workers n=50 |
Night shift workers n= 50 |
p-value |
|
Age |
28.6 ± 5.7 |
29.2 ± 6.3 |
0.654 |
|
Height (cm) |
160.6 ± 4.7 |
160.6 ± 1.6 |
0.932 |
|
Weight (kg) |
68.4 ± 6.0 |
70.9 ± 7.4 |
0.068 |
|
BMI (kg/m2) |
26.7 ± 2.7 |
27.6 ± 2.9 |
0.108 |
|
SBP (mm Hg) |
120 ± 6.0 |
120.8 ± 5.5 |
0.513 |
|
DBP (mm Hg) |
75.1 ± 4.8 |
76.7 ± 4.7 |
0.098 |
|
Pulse (rate/min) |
76.2 ± 4.3 |
76.8 ± 4.3 |
0.43 |
|
Serum IL-6 (pg/mL) |
6.7 ± 5.1 |
22.7 ± 11.9 |
< 0.0001* |
|
Tear IL-6 (pg/mL) |
13.6 ± 12.8 |
53.6 ± 49 |
< 0.0001* |
|
Distance traveled by the tear in Schirmer strip (mm) |
25.5 ± 12.2 |
25.9 ± 8.3 |
0.858 |
|
Duration of the distance traveled(min) |
1.7 ± 1.3 |
3.2 ± 1.4 |
< 0.0001* |
Data represented as mean ± SD and p-value < 0.05 is statistically significant
Correlation Between Tear IL-6 and Serum IL-6 in Day and Night Shift Workers
Tear IL-6 levels showed a significant positive correlation with serum IL-6 levels with r value 0.732 (p-value < 0.0001) and 0.624 (p-value < 0.0001) in day and night shift workers respectively (Table 2 and Figure 1).
Table 2: Correlation Between Tear and Serum IL-6 in Day and Night Shift Workers
|
Work schedule |
r value |
p-value |
|
Day shift workers |
0.732 |
<0.0001* |
|
Night shift workers |
0.624 |
<0.0001* |
*p value < 0.05 is statistically significant
 |
Figure 1: Correlation Between Tear IL-6 and Serum IL-6 in Day Shift Workers |
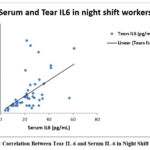 |
Figure 2: Correlation Between Tear IL-6 and Serum IL-6 in Night Shift Workers |
Prevalence of dry eye syndrome in day and night shift workers
A participant is diagnosed with dry eye syndrome if the duration taken to moisten the 15 mm Schirmer strips is more than 5 minutes. Among 50-day shift workers, 7 had dry eye syndrome (14%) and among 50-night shift workers, 24 had dry eye syndrome (40%). The Prevalence of dry eye syndrome was significantly higher in night shift workers when compared with day shift workers. (Table 3 and Figure 3).
Table 3: Prevalence Of Dry Eye Syndrome In Day And Night Shift Workers
|
Work schedule |
Dry Eye Syndrome |
Total |
|
|
Yes |
No |
||
|
Day shift workers |
7 |
43 |
50 |
|
Night shift workers |
24 |
26 |
50 |
|
Total |
31 |
69 |
100 |
*p value < 0.05 is statistically significant
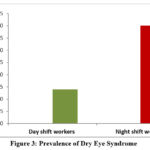 |
Figure 3: Prevalence of Dry Eye Syndrome |
ROC curve analysis to find out cut-off points of serum and Tear fluid IL-6
In ROC curve analysis, tear IL-6 levels showed the highest area under the curve (0.935) compared to serum IL-6 levels (0.883). The cut-off value for tear IL-6 was 38.9 pg/ml with 90.3% sensitivity and 97% specificity and the cut-off value for serum IL-6 was 16.6 pg/ml with 90.3% sensitivity and 87% specificity (Table 4 and Figure 4). This reveals that the patients are at higher risk of developing dry eye disease at a serum IL-6 level of 16.6 pg/ml and tear IL-6 level of 38.9 pg/ml. The analysis also shows the superiority of tear fluid analysis and suggests that tear fluid can be used as a minimally invasive technique to analyze IL-6 alternative to serum IL-6 analysis.
Table 4: ROC Curve Analysis, Cut-Off Points, Sensitivity and Specificity of Serum IL-6 and Tear Fluid IL-6
|
Variables |
Area under curve |
p-value |
Cut off point |
Sensitivity % |
1-Specificity % |
|
Serum IL-6 |
0.883 |
< 0.0001* |
16.6 |
90.3 |
87 |
|
Tear IL-6 |
0.935 |
< 0.0001* |
38.9 |
90.3 |
97 |
*p value < 0.05 is statistically significant
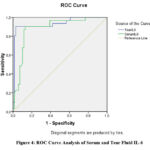 |
Figure 4: ROC Curve Analysis of Serum and Tear Fluid IL-6. |
Discussion
Around 10-30% of the working population do night shifts. Irregular hours from working night shifts lead to frequent alterations in the sleep pattern and awakening hours. This situation further paves the way for misalignment between the light-dark and sleep-wake cycles. The endogenous/oscillatory components of the circadian system are also affected. Various mental and physical health disorders are observed in this population, suggesting the risks of unfavorable circadian rhythms.IL-6 is usually secreted in a biphasic circadian pattern.32,33 In order to restrict this diurnal variation of secretion, we assayedIL-6 between 7 am and 8 am. Since the t ½ of IL-6 is approximately 60 minutes, a one-day wash-out period is sufficient. However, the carryover effect of IL-6 has been observed in several studies and thus leading to investigation of the further relationship between the shift work.34 There is a significant elevation of IL-6 in night shift workers when compared with day shift workers in several studies. The reason for the above statement may be due to insufficient sleep and disturbances in the circadian rhythm which leads to chronic stress.35In our study, we have also found that participants who worknight shifts frequently had significantly elevated IL-6 levels than those who had regular day shift work schedules supporting the above statement. We noted that there is no significant difference between height, weight, age, SBP, DBP, and pulse rate between day and night shift workers but the serum and tear IL-6 levels are significantly elevated in night shift workers compared to day shift workers with the p-value< 0.0001*. A positive correlation was also observed between serum and tear IL-6 between both groups in an earlier study.36 The night shift work was associated with the risk of obesity due to altered food intake at odd hours. Overeating in order to be awake favors a positive energy balance, and weight gain.37-39 The short sleep pattern and altered circadian rhythm lead to a reduction in leptin – a satiety hormone 38 and an increase in ghrelin – a hunger hormone that induces high energy intake.39 In contrast, our study revealed, that there is no significant difference in weight and BMI between the day and night shift groups with p-values of 0.068 and 0.108.
People working night shifts have high BP compared to day shift workers. A dip was observed in BP during sleeping hours which was attenuated at the beginning of the night shift.40,41 Sleep deprivation is associated with changes in the endocrine system and autonomic nervous system which leads to decreased parasympathetic tone, increased secretion of stress hormones like cortisol and nor-epinephrine and so increase in BP.42,43 In our study, we found no difference in the systolic and diastolic blood pressure between the day and night shift groups. Sleep deprivation can potentially impair tear secretion and can cause dry eye syndrome. The prevalence of dry eye syndrome was significantly high in night shift workers when compared with day shift workers.42,43 Similarly in our study also we found the same. Tear cytokine biomarkers provide critical information to fill the gaps between the mechanisms involved, etiopathogenesis, diagnosis, treatment, and response to treatment in dry eye syndrome.44 Our analysis also showed the superiority of tear fluid analysis and that tear fluid can be used as a minimally invasive technique to analyze IL-6 alternative to serum IL-6 analysis.
However, there are several disadvantages of tear fluid analysis like limited sample volume which will not be very suitable for sample extraction difficulties, evaporation of the tear fluid, and inter/intra-individual variations. Despite its less cost-effectiveness, the tear fluid-based analysis needs further deep understanding of its chemistry, composition, ease of sampling, and transport mechanisms as well as an established correlation between tear and blood concentrations of other analytes in further studies.45
Conclusion
The present study concluded that tear fluid and serum IL-6 are raised in night shift workers compared to day shift healthcare workers. Our study also proved that tear fluid can be used as a minimally invasive technique and a superior method to analyze IL-6. These findings help us to understand the etiology underlying the relationship between work schedule and inflammatory cytokines. The night shift work stress-induced systemic inflammation can lead to various systemic diseases including cardiovascular disorder (CVD) and insulin resistance syndrome/metabolic syndrome in the future if proper lifestyle modification and health awareness are not provided on time.
We had the Healthcare providers from various specialties from a single tertiary care hospital engaged and it was a Cross-sectional survey design, which helped us to identify causality between study variables which was our strength in this study. The study is limited to one tertiary care center with a limited number of participants and correlation between other inflammatory cytokines should be considered in future studies.
Acknowledgement
The authors wish to acknowledge the Management of Saveetha Medical College, SIMATS, Prof. Dr. N. Ananthi (HOD Clinical Biochemistry Department), Prof. Dr. G. S. R. Kedari (HOD Clinical Biochemistry Laboratory), Ortho Clinical Diagnostics, and all our Clinical Biochemistry Laboratory Technicians and Colleagues of Saveetha Medical College, SIMATS.
Conflict of Interest
The authors have no conflicts of interest.
Funding Source
There are no funding source
References
- Khosro S, Alireza S, Omid A, Forough S. Night work and inflammatory markers. Indian Journal of Occupational and Environmental Medicine. 2017 Jan;15(1):38.
CrossRef - Kogi K. Increasing flexibility in shiftwork arrangements. Work Stress 2015; 9: 211-218.
CrossRef - Smith L, McDonald I, Folkard S, Tucker P. Industrial shift systems. Appl Ergon 2018; 29: 273-280.
CrossRef - Kogi K, Thurman JE. Trends in approaches to night and shiftwork and new international standards. Ergonomics 2019; 36: 3-13.
CrossRef - Cappuccio FP, D’Elia L, Strazzullo P, Miller MA. Sleep duration and all-cause mortality: a systematic review and meta-analysis of prospective studies. Sleep. 2016 May 1;33(5):585-92.
CrossRef - Barton J, Spelten E, Totterdell P. The standard shift work index-a battery of questionnaires for assessing shift work-related problems. Work Stress 2017;9:4-30.
CrossRef - Monk TH. Shift work. In: Kupfer DJ, Roth T, Dent WC, editors. Principles and Practice of Sleep Medicine. Philadelphia: Saunders; 2012. p. 600-5.
- Akerstedt T. Adjustment of physiological and circadian rhythms and the sleep-wake cycle to shift work. In: Folkard S, Monk TH, editors. Hours of Work: Temporal Factors in Work Scheduling. Chichester, United Kingdom: John Wiley; 2015. p. 185-98.
- Boivin DB, Boudreau P, Kosmadopoulos A. Disturbance of the circadian system in shift work and its health impact. Journal of Biological Rhythms. 2022 Feb;37(1):3-28.
CrossRef - Hastings M. The brain, circadian rhythms and clock genes. Br Med J 2018; 317: 1704-1707.
CrossRef - Leproult R, Copinschi G, Buxton O, Cauter EV. Sleep loss results in anelevation of cortisol levels the next evening. Sleep. 2017;20:865e870.
- Young MW. Time travels: A 40‐year journey from Drosophila’s clock mutants to human circadian disorders (Nobel lecture). Angewandte Chemie International Edition. 2018 Sep 3;57(36):11532-9.
CrossRef - Leproult R, Copinschi G, Buxton O, Cauter EV. Sleep loss results in an elevation of cortisol levels the next evening. Sleep. 2020;20:865e870.
- Gordon NP, Cleary PD, Parker CE, Czeisler CA. The prevalence and health impact of shiftwork. Am J Public Health 2021; 76: 1225-1228.
CrossRef - Vener KJ, Szabo S, Moore JG. The effects of shift work on gastrointestinal (GI) function: a review. Chronobiofogia 2019; 16: 421-439.
- Weihrauch M, Wrbitzky R, Letzel S. Shift work in Bavaria — has this been affected by the new law regulating working hours? Arbeitsmedizin Sozialmedizin Umweltmedizin 2015; 32: 170-177.
- Makateb A, Torabifard H. Dry eye signs and symptoms in night-time workers. Journal of Current Ophthalmology. 2017 Dec 1;29(4):270-3.
CrossRef - Wang XS, Armstrong ME, Cairns BJ, Key TJ, Travis RC: Shift work and chronic disease: the epidemiological evidence. Occup Med, 2015; 61: 78-89.
CrossRef - Vetter C, Devore EE, Wegrzyn LR, Massa J, Speizer FE, Kawachi I, Rosner B, Stampfer MJ, Schernhammer ES: Association Between Rotating Night Shift Work and Risk of Coronary Heart Disease Among Women. JAMA, 2016; 315: 1726-1734.
CrossRef - Monk TH. Shift work. In: Kupfer DJ, Roth T, Dent WC, editors. Principles and Practice of Sleep Medicine. Philadelphia: Saunders; 2000. p. 600-5.
- Akerstedt T. Adjustment of physiological and circadian rhythms and the sleep-wake cycle to shift work. In: Folkard S, Monk TH, editors. Hours of Work: Temporal Factors in Work Scheduling. Chichester, United Kingdom: John Wiley; 2016. p. 185-98.
- Sparks K, Cooper CL, Fried Y. The effects of hours of work on health: A meta-analytic review. J Occup Organ Psychol 2009;70:391-408.
CrossRef - Foster RG, Kreitzman L. Rhythms of Life: The Biological Clocks thatControl the Daily Lives of Every Living Thing. London: Profile; 2014.
- Gabay C. Interleukin-6 and chronic inflammation. Arthritis research & therapy. 2018 Jul;8(2):1-6.
- Biomarkers Definitions Working Group. Biomarkers and surrogate endpoints: preferred definitions and conceptual framework. Clin Pharmacol Ther. 2018; 69(3):89–95.
CrossRef - Gutman S, Kessler LG. The US Food and Drug Administration perspective on cancer biomarker development. Nat Rev Cancer. 2016;6:565–71.
CrossRef - Hagan S, Martin E, Enríquez-de-Salamanca A. Tear fluid biomarkers in ocular and systemic disease: potential use for predictive, preventive and personalised medicine. Epma Journal. 2016 Dec;7(1):1-20.
CrossRef - Kecklund G, Axelsson J. Health consequences of shift work and insufficient sleep. BMJ. (2016) 355:i5210. doi:10.1136/bmj.i5210.
CrossRef - Bachhuber F, Huss A, Senel M, Tumani H. Diagnostic biomarkers in tear fluid: from sampling to preanalytical processing. Scientific reports. 2021 May 12;11(1):1-9.
CrossRef - Palay DA, Krachmer JH. Primary care ophthalmology. Mosby; 2015.
- Bjorvatn B, Axelsson J, Pallesen S, Waage S, Vedaa Ø, Blytt KM, Buchvold HV, Moen BE, Thun E. The association between shift work and immunological biomarkers in nurses. Frontiers in public health. 2020:415.
CrossRef - Nakamura Y, Sotozono C, Kinoshita S. Inflammatory cytokines in normal human tears. Current eye research. 2021 Jan 1;17(6):673-6.
CrossRef - Bredow S, Guha-Thakurta N, Taishi P, Obál F Jr, Krueger JM. Diurnal variations of tumor necrosis factor alpha mRNA and alpha-tubulin mRNA in rat brain. Neuroimmunomodulation 2000;4:84-90.
CrossRef - Khosro S, Alireza S, Omid A, Forough S. Night work and inflammatory markers. Indian Journal of Occupational and Environmental Medicine. 2011 Jan;15(1):38.
CrossRef - Grimaldi D, Carter JR, Van Cauter E, Leproult R:Adverse Impact of Sleep Restriction and Circadian Misalignmenton Autonomic Function in Healthy YoungAdults. Hypertension, 2016; 68: 243-2501.
CrossRef - Yilmaz PT, Atakan N, Bozkurt B, Irkec M, Mesci L, Aban D, Tezcan I. Determination of Tear and Serum Inflammatory Cytokines in Patients with Rosacea Using Luminex Technology. Investigative Ophthalmology & Visual Science. 2009 Apr 28;50(13):3592.
- Chen Y, Lauren S, Chang BP, Shechter A. Objective food intake in night and day shift workers: a laboratory study. Clocks Sleep. 2018; 1 (1): 42-9.
CrossRef - McHill, A.W.; Melanson, E.L.; Higgins, J.; Connick, E.; Moehlman, T.M.; Stothard, E.R.;Wright, K.P. Impact of circadian misalignment on energy metabolism during simulated nightshift work. Proc. Natl. Acad. Sci. USA 2014, 111, 17302–17307.
CrossRef - Buxton, O.M.; Cain, S.W.; O’connor, S.P.; Porter, J.H.; Duffy, J.F.; Wang, W.; Czeisler, C.A.; Shea, S.A. Adverse metabolic consequences in humans of prolonged sleep restriction combined with circadian disruption. Sci. Transl. Med. 2012, 4, 129ra43.
CrossRef - Chau NP, Mallion JM, de Gaudemaris R, Ruche E, Siche JP, Pelen O, Mathern G. Twenty-four-hour ambulatory blood pressure in shift workers. Circulation 1989; 80: 341–347.
CrossRef - Kitamura T, Onishi K, Dohi K, Okinaka T, Ito M, Isaka N, Nakano T. Circadian rhythm of blood pressure is transformed from dipper to a non-dipper pattern in shift workers with hypertension. J Hum Hypertens 2002; 16: 193–197.
CrossRef - Leproult R, Copinschi G, Buxton O, Cauter EV. Sleep loss results in an elevation of cortisol levels the next evening. Sleep. 1997;20:865e870.
- Boivin DB, Boudreau P, Kosmadopoulos A. Disturbance of the circadian system in shift work and its health impact. Journal of Biological Rhythms. 2022 Feb;37(1):3-28.
CrossRef - Wei Y, Gadaria-Rathod N, Epstein S, Asbell P. Tear cytokine profile as a noninvasive biomarker of inflammation for ocular surface diseases: standard operating procedures. Investigative ophthalmology & visual science. 2013 Dec 1;54(13):8327-36.
CrossRef - Brunauer A, Ates HC, Dincer C, Früh SM. Integrated paper-based sensing devices for diagnostic applications. InComprehensive Analytical Chemistry 2020 Jan 1 (Vol. 89, pp. 397-450). Elsevier.
CrossRef








