Manuscript accepted on :04-10-2023
Published online on: 27-11-2023
Plagiarism Check: Yes
Reviewed by: Dr. Santoshi Naik and Dr. Ajit Kumar
Second Review by: Dr. Anji
Final Approval by: Dr. Patorn Piromchai
Ahmed Jihad Abdulkadhim1* , Nidhal Yousif Mohammed1
, Nidhal Yousif Mohammed1 and Murtadha Allawi Jebur2
and Murtadha Allawi Jebur2
1Department of Medical Lab Technology, College of Health and Medical Technology, Southern Technical University, Basra/Iraq.
2Al Basra Teaching Hospital in Iraq.
Corresponding Author E-mail: albasrawii180@gmail.com
DOI : https://dx.doi.org/10.13005/bpj/2822
Abstract
The coronavirus disease (COVID-19) is an infectious viral illness that leads to the development of acute respiratory syndrome. It exhibits a high level of contagiousness. The aforementioned virus is accountable for an incidence of pneumonia that transpired in early December 2019 in Wuhan, situated in the People's Republic of China. The global pandemic declaration on March 11, 2020, marked a significant turning point in the world's demography, as the virus had tragically claimed the lives of over 5.3 million individuals worldwide. The emergence of the Coronavirus (COVID-19) pandemic has presented an unparalleled catastrophe, resulting in the loss of many lives via several channels including social, psychological, physical, and economic dimensions. The danger associated with the virus originates from its heightened transmissibility and extensive mutational variability, as well as its impact on several bodily systems including the circulatory, neurological, renal, hepatic, nervous, and endocrine systems. The pathogenesis of Coronavirus disease 2019 (COVID-19) is intricate, and its clinical presentation is diverse, exhibiting various imaging findings that vary based on the severity of the illness and its progression through time. A general statistical comparison was made for the biochemical markers in the patients infected with only Coronavirus and patients infected with Coronavirus and complications of diabetes mellitus compared to the control group according to gender, in order to monitor the role of different biomarkers in causing a disease, with an evaluation of the difference in their levels, and the study aimed to investigate biomarkers and study the relationship between these biomarkers for COVID-19 patients with and without Diabetes Mellitus, to provide a dynamic approach to understanding the disease to diagnosis and follow-up, so as to improve the development of patients' treatment. The study performed a representative sample of (238) participants between the ages (25-80) year, of whom (81) were in a healthy control group, (78) were infected only with Coronavirus, (79) were infected with Coronavirus and had complications of diabetes mellitus, who visited Al-Basra Teaching Hospital and Allmwanei Hospital in Al-Basra province between October 2021 and February 2022. The age average for the study population was (25-80) years. Serum and blood levels of human CBC, ESR, CRP, Ferritin, D-Dimer, IL 6, Albumin, FBS, HbA1c, Troponin, Cholesterol, Triglyceride, HDL, LDL, VLDL, Creatinine, Urea, Uric acid and GFR were measured. The results show a highly significant increase in WBcs, ESR, CRP, Ferritin, D-Dimer, IL-6, Creatinine, Urea and Uric acid. , and a highly significant decrease in lymphocyte, albumin, HDL and GFR for patients compared to the control group as a total number and the number of males and females separately, While the results of comparing biochemical markers in the patients infected with Coronavirus and who had a diabetic complication a higher significant increase than patients without diabetic complication. The study of these biomarkers provides a dynamic approach to understanding the disease to diagnosis and follow-up, so as to improve the development of patients' treatment and study the relationship between these biomarkers for COVID-19 patients with and without Diabetes Mellitus.
Keywords
Biochemical indicators; Clinical Markers; COVID-19; Diabetes Mellitus; Inflammatory Markers
Download this article as:| Copy the following to cite this article: Abdulkadhim A. J, Mohammed N. Y, Jebur M. A. The correlation between biochemical indicators in COVID-19 patients with and without Diabetes Mellitus in Basra, Iraq. Biomed Pharmacol J 2023;16(4). |
| Copy the following to cite this URL: Abdulkadhim A. J, Mohammed N. Y, Jebur M. A. The correlation between biochemical indicators in COVID-19 patients with and without Diabetes Mellitus in Basra, Iraq. Biomed Pharmacol J 2023;16(4). Available from: https://bit.ly/47snDI0 |
Introduction
Coronavirus (COVID-19) will continue to be a major threat to public health. Understanding the pathophysiology and physiology of the organ function, that is targeted by the virus, was proven to be crucial for the rational creation of medications1. COVID-19 disease has been characterized by a complex pathophysiology, and heterogeneous clinical presentation, with a wide range of imaging findings, depending on both disease severity and time course(2). The pathogenesis of Coronavirus disease 2019 (COVID-19) is intricate, and its clinical presentation varies widely. The imaging results associated with the disease exhibit considerable diversity, influenced by the severity of the illness and its progression through time2.
The scientific community needs reliable biomarkers that indicate the development of The scientific community needs reliable biomarkers that indicate the development of coronavirus disease (COVID-19), these biomarkers are measurable biochemical that can be used to determine disease severity, these biomarkers can be physiological, anatomical, or biochemical, and can be objectively measured and evaluated. They also allow assessment of drug response and allow timely therapeutic intervention. Clinical symptoms can also be interpreted with greater confidence by using biochemical markers in order to classify patients at risk according to the speed and severity of disease progression. Also, These biomarkers are associated with an understanding of the mechanisms causing viral disease, as well as cellular damage, which are useful for clinical management and prevention of death risk3.
Biomedical markers in COVID-19 disease can be useful in several areas, including early detection of the disease, identifying and classifying the severity of the disease, the possibility of admission to the hospital and the formulation of standards for staying in the intensive care unit and determine the criteria for leaving the intensive care unit or hospital4.
Epidemiology, in fact, builds on clinical study, observation, and analysis, as well as screening and diagnosis. Changes in biochemical markers indicate changes in the composition of body fluids and tissues through which, it is possible to find a homogeneous classification of the disease and its associated risk factors. This in turn expands our basic information related to the early manifestations of the disease and up to the final stages of it5.
Numerous studies have demonstrated that diabetes mellitus could induce diverse complications, such as diabetes mellitus complications nephropathy, diabetes mellitus complications cardiovascular, diabetes mellitus complications neuropathy, and diabetes mellitus complications liver, and diabetes mellitus complications diabetic retinopathy which have been the major causes of its morbidity and mortality 6.
Biochemical Indicators and Inflammatory markers of COVID-19.
COVID-19 disease has been characterized by a complex pathophysiology, and heterogeneous clinical presentation, depending on both disease severity and time course. Accordingly, several factors which contribute to the early diagnosis of COVID-19 pneumonia have been identified, providing important information regarding the inflammatory process, organ damage, severity of the disease, the extent of stay in the stay in (ICU) and mortality, so in this research the evaluation of levels of different inflammatory and biochemical indicators in patients infected with Coronavirus with or without diabetes, such as:
Complete blood count (CBC) is a regular study for all patients that gives essential parameters that can help with clinical care, such as diagnosis, the presence of infection or inflammation, anaemia, therapy response, aetiology, and the stage of inflammatory disease. According to a study conducted in five nations throughout Asia, Africa, and the United States, (CBC) is the most widely used initial laboratory test7.
Erythrocytes Sediment Rate (ESR) is a laboratory indicator of inflammation that is typically only moderately increased in viral infections, studies have demonstrated that the host’s inflammatory reaction to COVID-19 can be substantial. This heightened response may result in a cytokine storm, which can contribute to additional disease complications and dysfunction in multiple organs8.
C-reactive protein (CRP) is a hepatically synthesized protein that serves as an early biomarker for the presence of infection and inflammation, the normal concentration of (CRP) in the blood is less than 10 mg/l; nevertheless, it rises rapidly within 6-8 hours and peaks 48 hours after the commencement of the disease (Marnell et al., 2005), and was identified as a key measure that changes considerably in severe COVID-19 patients9.
Interleukin-6 (IL-6) is a multifunctional proinflammatory cytokine that promotes the proliferation of myeloid progenitor cells, facilitates the growth and activation of leukocytes, and induces fever along with the synthesis of acute phase proteins, including C-reactive protein (CRP). The cytokine storm associated with COVID-19 is primarily characterized by the overexpression of interleukin-6 (IL-6) which is a cytokine of significant importance that is produced in response to Toll-like receptor 7 (TLR-7) signalling, activated by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2)10.
D-dimer which can specifically reflect secondary hyperfibrinolysis and a hypercoagulable condition in the body during coagulation function testing and serves as an index sensitive to reflecting thrombosis. Fibrinogen (FIB) levels can suggest a prethrombotic condition in the body11, 12.
Ferritin Hyperferritinemia, which is caused by infection-induced inflammation, is linked to Intensive care unit (ICU) admission and high mortality, and it serves as a warning sign to identify high-risk patients and direct therapeutic action to decrease inflammation13.
Cardiac troponin I (cTnI): It has been used as a crucial biomarker for non-specific cardiac conditions, such as myocardial infarction and acute coronary syndrome. This advancement enables broader screening capabilities, facilitating the early detection and subsequent intervention of cardiac injury14. In the context of COVID-19, the levels of cardiac troponin I (cTnI) were notably elevated in individuals with severe manifestations of the disease (Lippi et al., 2020). However, because the troponin readings did not appear to presage the disease’s progression, it is impossible to say whether troponin is a ‘predictive’ sign for COVID-19 severe variants15.
Fasting Blood Sugar (FBS) is a rapid screening tool, with patients at high risk being assessed for more precise mortality indicators. During an epidemic, this method could be useful for triaging patients and ensuring that they are properly managed16.
Glycosylated haemoglobin (HbA1c) is a reliable indicator of long-term glucose control that gives an average of the previous three months’ values, it can be used to assess diabetes status and identify COVID-19 high-risk patients with low diabetes awareness17.
Renal functions test which include:
Blood Urea: Higher urea production is related to any illness associated with tissue breakdown. Less than 10% of the urea generated by the liver is removed through perspiration and the digestive system, but the bulk is transported via the circulation to the kidneys, where it is expelled as urine18.
Serum Creatinine: Plasma and/or serum creatinine are two of the chemicals that are most often analysed in clinical chemistry laboratories all around the world (Delanaye et al., 2014). Therefore, it has developed into an essential clinical tool for GFR measurement. In clinical settings, reduced GFR is measured by an increase in plasma and/or serum creatinine19.
Estimate Glomerular Filtration Rate (eGFR): The gold standard for evaluating kidney function is measured GFR (mGFR) utilizing urine or plasma clearance of exogenous filtration indicators, however, it is not commonly available due to the complexity of testing techniques. Serum creatinine is the most frequent indicator used to calculate GFR, and the MDRD Study equation is the gold standard for doing so20.
Uric Acid: The majority of research found that inflammation can cause an increase in (uric acid), especially when the virus infects the respiratory system 21. Serum uric acid on the other hand, tends to drop with a central nervous system illness22.
Lipid Profile: The lipid disorders in COVID-19 patients have lower total cholesterol (TC), low-density cholesterol (LDL-C), and high-density cholesterol (HDL-C) levels. The relationship between COVID-19 and triglyceride (TG) levels isn’t always clear according to some research (Feingold, 2000). Dyslipidaemia is linked to metabolic, vascular, and coagulation issues, thus this is important, COVID-19 sufferers may experience more severe symptoms as a result23.
Serum Albumin: Hypo-albuminemia is very frequently noticed in patients with conditions like diabetes, hypertension and chronic heart failure, and these patients are statistically most vulnerable to SARS-CoV-2 infection24.
Materials and Methods
Samples Collection
The study was conducted on (238) participants between the ages (25-80) years, of whom (81) were in a healthy control group, (78) infected only with Coronavirus. and (79) infected with Coronavirus and had a complications of diabetes mellitus. Patients diagnosed with COVID-19 who also have diabetes and associated comorbidities were categorized according to the severity of their diseases and their hospitalization status. Patients classified as moderate-risk were sent to hospital wards, and those deemed severe were assigned to intensive care units. In intensive care units classified patients according to with or without Positive Airway Pressure (CPAP) therapy. Between November 2021 and May 2022, all participants of the study conducted visits to Al-Basra Teaching Hospital and Allmwanei Hospital, both located in the AL Basra province, ethical approval ID=815 issued by the Basra Health Department dated 10-11-2021. The mean age of the study population ranged from 25 to 80 years. All participants in this research were assessed by hospital experts. The practical component of the research was conducted in the Department of Medical Laboratory Technology at Southern Technical University in Basra.
Blood samples were collected, extracting over 5 ml of blood from both the patients and controls. Subsequently, about 1.8 ml of the blood was transferred into anticoagulant tubes that contained sodium citrate. Subsequently, the specimen underwent centrifugation at a speed of 3000 revolutions per minute for a duration of 15 minutes. Following this, the plasma was extracted and preserved at a sub-zero temperature of -20 °C till its utilisation for analytical purposes. In addition, there are Erythrocyte Sedimentation Rate (ESR) test tubes and tubes containing EDTA as an anticoagulant that may be used. The plasma and serum of each patient were allocated into Eppendorf tubes and afterwards subjected to freezing. The laboratory examination will commence after the necessary quantity has been attained. A significant number of individuals were excluded from the study due to their failure to meet the specified inclusion criteria. These criteria encompassed patients with comorbid conditions, such as hypertension, as well as patients with hormonal imbalances. also, investigated verify the patient’s information, age, gender, height, weight, vaccination or not, and the severity of the injury.
Statistical Analysis
The Statistical Package for the Social Sciences (SPSS) version 22 was used in order to carry out the statistical analyses. For the purpose of data representation, means and standard deviations were used. The analysis of variance (ANOVA) was carried out in order to determine whether or not there was a statistically significant difference in the mean of normally distributed variables., P-values (P≤ 0.05) are significant.
Results
The complete informationis shown in table (1).
Table 1: Basic characteristics of the participants, according to the number and disease complications.
|
Study Groups/ Age (year) |
Groups number |
Complication as a total number |
|||||
|
Gender |
Total number |
Severity |
Severe = 35 |
||||
|
Male |
Female |
Moderate |
Severe |
With CPAP |
Without CPAP |
||
|
Control group (Healthy) Age = (30-80) |
41 |
40 |
81 |
——- |
——- |
——- |
——- |
|
Covid-19 patients without diabetes Age = (30-80) |
40 |
38 |
78 |
——- |
——- |
——- |
——- |
|
Covid-19 patients with diabetes Age = (38-80) |
40 |
39 |
79 |
44 |
35 |
18 Aged (55-80) |
17 |
The results show by the statistical comparison between the biomarkers in the patients infected with Coronavirus and the control group a highly significant increase in WBCs, ESR, CRP, Ferritin, D-Dimer, IL-6, Creatinine & Urea and Uric acid for patients compared to the control group as a total number and as a (males and females) number, While, the results show a highly significant decrease in lymphocyte, albumin, HDL and Glomerular filtration rate (GFR) for patients compared to the control group as a total number and the number of males and females separately, as show in table (2)
A general statistical comparison was made for the biochemical markers in the patients infected with Coronavirus and who had a diabetic complication compared to the control group according to gender and as a total number of (79) patients, the results showed that people with diabetes significantly increased biomarkers than patients without diabetes minutes, as shown in the statistical Table (3).
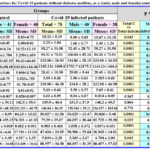 |
Table 2: Statistical analysis of biomarkers for Covid-19 patients without diabetes mellitus, as a (total, male and female) number compared to the control group. |
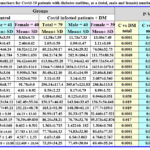 |
Table 3: Statistical analysis of biomarkers for Covid-19 patients with diabetes mellitus, as a (total, male and female) number compared to the control group. |
Discussion
The study of these biomarkers provides a dynamic approach to understanding the disease to diagnosis and follow-up, so as to improve the development of patients’ treatment. The results show a highly significant increase in WBcs, ESR, CRP, Ferritin, D-Dimer, IL-6, Creatinine & Urea and Uric acid. While, the results show a highly significant decrease in lymphocyte, albumin, HDL and Glomerular filtration rate (GFR) for COVID-19 patients compared to the control group as a total number and the number of males and females separately
This is consistent with what has been confirmed by another study25. Also, other studies showed that death and disease severity in COVID-19 were associated with a higher WBC count accompanied by lower lymphocyte levels. The resistance against infectious diseases is activated through the immune system, Studies have found that angiotensin-converting enzyme (ACE) is an effector and plays a strong role in recruiting inflammatory cells to tissues26, 27. Circulating lymphocytes throughout the body produce proteins and antibodies to fight off pathogens and help the immune system fight infection. B cells attack viruses while T cells produce cytokines and destroy virus-damaged cells. Lymphocytes take in the virus as they contain about 1000 molecules of ACE2 which leads to a decrease in these cells through programmed death as a result of infection with the virus28, and this confirms our study.
Other studies that align with the findings of our research, in one study that targeted the diagnostic and warning role of (CRP) in COVID-19 patients, which included 85 patients, it was found that the (CRP) levels were much higher than the normal rate. Where the increase in (CRP) levels of more than 53 mg / L is associated with a 10 times higher risk for disease progression. Increasing serum ferritin levels is an important marker in the acute phase of viral infections, including COVID-19. Hyperferritin contributes to the severity of COVID-19, through inflammation, hyperproteinemia, hypercoagulability, and immune dysfunction29, it was found that there is a strong significant correlation between ferritin level with the severity of the injury in the clinical results obtained30. In a cross-sectional study of a large number of COVID-19 patients, D-dimer was elevated, and its levels were associated with disease severity. Thus, it can be considered a reliable predictive biomarker for the mortality of patients in hospitals31. The measurement of D-Dimer levels along with coagulation parameters is very useful in controlling and managing the disease in the early stage32. And that align with the findings of our research, this agrees with the results of our study.
Regarding IL-6 other studies agree with the results of our study, as across-sectional study, IL-6 levels were estimated for COVID-19 patients in intensive care units and acute respiratory distress syndrome (ARDS). It was found an increase in (IL-6) levels compared to the healthy group. This proves the sensitivity of this inflammatory marker as an indicator in infection control and diagnosis. In the same study, it was found that the value (20.92 pg/ml) is an indicator of long-term injury33. In another clinical study correlating (COVID-19 with IL-6), (366) patients were included as moderate cases, (411) as serious cases and (124) as critical cases. Clinical data reported a higher level of (IL-6) for patients compared to the control group, with a high statistically significant relationship. The study also revealed that (IL-6) remained high in critical patients even after the recovery stage, and its value was (37.65 pg/ml), and this predicts the possibility of death inside the hospital34.
Studies indicated hypoalbuminemia was common in patients with (COVID-19), and that its levels are associated with the severity of the disease, which is consistent with our study. Therefore, dynamic monitoring of albumin levels is necessary and should be followed up during the treatment of patients and used as a tool for evaluation and diagnosis of infection35, It was found that low albumin levels could predict the outcome of disease on admission to patients independently of other biochemical indicators36, 37. This is consistent with previous studies reporting lower blood albumin, which is associated with acute kidney injury and the severity of respiratory distress syndrome. In another study, it was found that 17.7% of COVID-19 patients had hypoalbuminemia during the analysis of 3 consecutive time points during one week38. In a large statistical study in which (2623) COVID patients were hospitalized with hypoalbuminemia as follows: (38.2%) of them were in non-critical condition and (71.2%) suffered from serious diseases. The hypoalbuminemia was related to cytokine release, which was also associated with age, comorbidities, length of hospitalization and death35.
With regard to blood sugar indicators, studies confirmed consistent with the results of our research, in one of these studies there were nine cross-sectional studies, involving approximately (40) million participants worldwide. The results indicated that the incidence of diabetes was (15.53) per (1000) person after recovery. Also, the relative risk of contracting diabetes after the end of infection increased by (1.7), and there was a high positive significant association between infection with corona and the risk of developing type 2 diabetes for all ages and genders after recovery39. COVID-19 is sometimes associated with the inflammation of the pancreas. The virus can be found in the pancreas cells that are responsible for producing insulin. This raised some concerns about COVID-19 causing diabetes. Where Miao et al. reported pancreatitis in some patients with COVID-19 without respiratory symptoms40.
COVID-19 infection was associated with a mild elevation in cardiac indices41. Elevated levels of cardiac troponin (26.9%) were found. These levels were significantly associated with disease severity and mortality. Thus, early measurement of cardiac troponin is useful in risk classification in COVID-1942. Coronavirus infection causes an increase in inflammatory cytokines, and this may lead to alter the lipid profile of patients. Recent research indicates that low levels of high-density lipoprotein cholesterol are associated with mortality and the severity of disease, as it plays a role in controlling infectious diseases and modulating the immune system through its association with pathogenic fats43. A similar study included 75 cases, (50) of them were infected with coronavirus and(25) were healthy people, the statistical results showed, lower levels of high-density lipoprotein cholesterol compared to healthy subjects 44, that is agrees with the results of our study.
Regarding renal function indicators, it was found in a study conducted on (59) patients infected with COVID-19 that (27%) of them had elevated levels of urea nitrogen with a high level of creatinine in the blood45. Another study also conducted on (710) patients with (COVID-19) showed that (26.9%) had simple hematuria, (44%) had proteinuria, (14.1%) had elevated levels of urea nitrogen and (5.5%) had elevated serum creatinine46. Kidneys act as filters that filter out toxins and body waste, so small clots formed in the bloodstream can block the small blood vessels of people with COVID-19, impairing kidney function47. And that aligns with the findings of our research.
In one study it agrees with the results of our study, include (1800) patients aged (73-86) years, of whom 55% were males, were included. The estimated glomerular filtration rate was in the range (45-59). Thus, the death rate for (28) days was (42.3%). It is concluded from this, that the eGFR rate upon hospital admission is an independent predictor of mortality in elderly patients infected with COVID-1948. Most evidence indicates a negative impact of COVID-19 on a decreased glomerular filtration rate, with an increased risk of patients being admitted to the intensive care unit (ICU) and dying49, 50.
Regarding about comparison made for the biochemical markers in the patients infected with Coronavirus and who have a diabetic complication compared to the control group, the results showed that people with diabetes significantly increased biomarkers than patients without diabetes minutes likely to suffer serious complications when infected with COVID-19. In general, people with diabetes are more susceptible to complications and more severe when infected with any virus51. Diabetes is considered a risk factor for the severity of COVID-19. Coronavirus usually triggers the body to produce cytokines, which are inflammatory factors that make insulin resistance worse and, as a consequence raise blood sugar. When blood sugar is high, the ability of the white blood cells of the body to fight infection is reduced, which again, puts a diabetic at greater risk52.
Studies confirmed that the Coronavirus caused a greater decrease in the number of lymphocytes in patients with diabetes53, 54, the number of white blood cells is significantly associated with death in patients with COVID-19. Therefore, higher (WBC) levels should be given more attention in the treatment of COVID-1925. In a study that included (63) patients with coronavirus, of whom (16) had diabetes and (47) did not, it was found that the diabetic group had a lower number of lymphocytes and reached the minimum level. In summary, diabetics with COVID-19 have fewer lymphocytes with a longer hospital stay55. These studies agree with the results of our research.
In a series of articles (29) that included (15,282) patients, of whom (4,733) had diabetes and (10,549) did not have diabetes. The pooled result of these studies showed that serum (CRP and D-dimer) was significantly higher in patients with COVID-19 diabetes and significantly higher than in non-diabetic patients56. Recent studies found a strong correlation between serum ferritin and blood glucose levels in patients with diabetes (type 2). In a study that included (172) patients, (84) of them had type-2 diabetes and (88) formed a control group. Serum ferritin, (HbA1c), (CRP) and uric acid levels were compared between groups. The results showed increased levels of ferritin for diabetes patients with significantly increased levels of (HbA1c) and a positive correlation was found between them in the blood. This indicates the possibility of using (CRP) and serum ferritin levels as a screening tool for the early diagnosis of diabetes57. It was found that the severity of COVID-19 disease depends primarily on cytokine storm syndrome. Consequently, people with diabetes show elevated levels of ferritin in the blood and face the possibility of developing serious complications58. and all these studies agree with our research.
Regarding IL-6 In one study which agrees with our research, that included (59) patients with COVID-19, Interleukin-6 and D-dimer levels were assessed, and their levels were significantly higher in the diabetic group than in the normal group (P < 0.001). Although all patients received standard treatment for COVID-19 infection, (D-dimer and IL-6) levels were higher in patients with diabetes59. Interleukin-6 is a multifunctional pro-inflammatory cytokine that stimulates the development of inflammation, insulin resistance and the pathogenesis of diabetes type-260. About albumin the results show a highly significant decrease in albumin for diabetes patients infected with COVID-19 compared to the control group. A study was conducted to analyze hypoalbuminemia as an indicator of mortality in patients with COVID-19, and the results of the study indicated that checking serum albumin upon admission of Corona patients to the hospital may help in identifying patients at risk of infection, which determines life and death61.
For kidney biomarkers, the results show a highly significant increase in (creatinine, urea, and uric acid), with a significant decrease in (eGFR), for diabetes patients infected with COVID-19. In one study that investigated (819) patients with COVID-19 who were admitted to the hospital, the results of clinical analyses revealed patients with high sugar and blood pressure, in addition to kidney disease. The high level of creatinine in the blood was one of the most important factors associated with deaths, which underscores the importance of renal function for COVID-19 patients and the importance of careful management of these patients62, and that aligns with the findings of our research.
Also, confirmed the results of our research through many studies regarding COVID-19 patients who had diabetes Mellitus, such as, in a study of (193) patients with severe symptoms of COVID-19 disease, (48) had diabetes. The results showed that diabetic patients had higher levels of white blood cell count, (CRP), ferritin, D-dimer, and interleukin (IL-6). The non-surviving patients were reported to have a severe inflammatory response, thrombosis, and (hepatic & renal) impairment. In short, diabetes may contribute to an increased risk of death63. In a study conducted on (466) patients who were hospitalized with severe symptoms of COVID-19 disease. Most of them had diabetes. In this study, (168) of the patients who survived had a heart attack. The results showed that myocardial injury is a common outcome in patients with COVID-19, and an elevated troponin level was an independent predictor of mortality64. In a large observational study involving (51, 919) COVID-positive participants and two uninfected groups. They found an increase in total cholesterol, triglycerides, and (LDL) cholesterol with a decrease in (HDL) cholesterol. The results also confirmed that the degree of dyslipidaemia was greater for those with infection who needed intensive care admission. Dyslipidaemia was attributed to behavioural factors during the recovery period, such as decreased physical activity after the virus, or binge eating after the return of taste65.
Conclusion
Diabetes is responsible for the slow destruction of the immune response and is responsible for the severity of the infection with COVID-19. So, a statistical study for chemical biomarkers in patients with type 2 diabetes mullets, according to the complication of infection severity, and evaluating of the levels of different biochemical markers in patients infected with Coronavirus with or without diabetes, such as (CBC, ESR, CRP, Ferritin, Albumin, D-Dimer, IL-6, FBS, HbA1C, eGFR, uric acid, urea v creatinine and lipid profile). Where, the clinical symptoms associated with the severity of the infection and diabetes complication are illustrated, through the elevated levels of the inflammatory biochemical markers. The results showed all biomarkers tend to have high sensitivity and specificity for COVID-19 with Diabetes Mellitus patients. Here, we find that the blood characteristics of those infected with COVID-19 changed, which led to the activation of inflammatory reactions, cytokine storms, and the stimulation of hypercoagulation. This, in turn, gave a more accurate interpretation of the severity of the disease and risk classification to distinguish moderate and severe cases.
Acknowledgments
The authors express their gratitude to M.Sc. Muntadher A Hassan and M.Sc. Zeina M Mubarak for their valuable support and exceptional technical assistance.
Conflict of Interest
The authors do not report any financial or personal connections with other persons or organizations, which might negatively affect the contents of this publication and/or claim authorship rights to this publication.
Funding source
The funding is of a personal nature.
References
- Gentzsch M, Rossier BC. A pathophysiological model for COVID-19: critical importance of transepithelial sodium transport upon airway infection. Function. 2020;1(2):zqaa024.
CrossRef - Carubbi F, Salvati L, Alunno A, Maggi F, Borghi E, Mariani R, et al. Ferritin is associated with the severity of lung involvement but not with worse prognosis in patients with COVID-19: data from two Italian COVID-19 units. Sci Rep [Internet]. 2021;11(1):1–11. Available from: https://doi.org/10.1038/s41598-021-83831-8
CrossRef - Ponti G, Maccaferri M, Ruini C, Tomasi A, Ozben T. Biomarkers associated with COVID-19 disease progression. Crit Rev Clin Lab Sci. 2020;57(6):389–99.
CrossRef - Samprathi M, Jayashree M. Biomarkers in COVID-19: an up-to-date review. Front Pediatr. 2021;8:607647.
CrossRef - Jain KK, Jain KK. Role of biomarkers in health care. Handb Biomarkers. 2010;115–88.
CrossRef - Guariguata L, Whiting DR, Hambleton I, Beagley J, Linnenkamp U, Shaw JE. Global estimates of diabetes prevalence for 2013 and projections for 2035. Diabetes research and clinical practice. 2014 Feb 1;103(2):137-49.
CrossRef - Horton S, Sullivan R, Flanigan J, Fleming KA, Kuti MA, Looi LM, et al. Delivering modern, high-quality, affordable pathology and laboratory medicine to low-income and middle-income countries: a call to action. Lancet [Internet]. 2018;391(10133):1953–64. Available from: http://dx.doi.org/10.1016/S0140-6736(18)30460-4
CrossRef - Simon D, Tascilar K, Kleyer A, Fagni F, Krönke G, Meder C, et al. Impact of cytokine inhibitor therapy on the prevalence, seroconversion rate and longevity of the humoral immune response against SARS‐CoV ‐2 in an unvaccinated cohort . Arthritis Rheumatol. 2021;0–3.
CrossRef - Marnell L, Mold C, Du Clos TW. C-reactive protein: Ligands, receptors and role in inflammation. Clin Immunol. 2005;117(2):104–11.
CrossRef - Wang G, Wu C, Zhang Q, Wu F, Yu B, Lv J, et al. C-reactive protein level may predict the risk of COVID-19 aggravation. Open Forum Infect Dis. 2020;7(5):1–5.
CrossRef - Velazquez-Salinas L, Verdugo-Rodriguez A, Rodriguez LL, Borca M V. The role of interleukin 6 during viral infections. Front Microbiol. 2019;10(MAY):6–11.
CrossRef - Matuleviciene-Anängen V, Rosengren A, Svensson AM, Pivodic A, Gudbjörnsdottir S, Wedel H, et al. Glycaemic control and excess risk of major coronary events in persons with type 1 diabetes. Heart. 2017;103(21):1687–95.
CrossRef - Pangaribuan JP, M. Aron Pase. Correlation between HbA1C and D-dimer in Type 2 Diabetic with COVID-19 Patients. J Endocrinol Trop Med Infect Dis. 2021;3(4):145–51.
CrossRef - Kernan KF, Carcillo JA. Hyperferritinemia and inflammation. Int Immunol. 2017;29(9):401–9.
CrossRef - Fitzgerald G, Kerley RN, Kiernan TJ. High-sensitivity troponin assays: development and utility in a modern health-care system. Expert Rev Cardiovasc Ther [Internet]. 2019;17(10):763–70. Available from: https://doi.org/10.1080/14779072.2019.1675514
CrossRef - Lippi G, Lavie CJ, Sanchis-Gomar F. Cardiac troponin I in patients with coronavirus disease 2019 (COVID-19): Evidence from a meta-analysis. Prog Cardiovasc Dis [Internet]. 2020;63(3):390–1. Available from: https://doi.org/10.1016/j.pcad.2020.03.001
CrossRef - Bhandari, Shaktawat AS, Tak A, Patel B, Shukla J, Singhal S, et al. Logistic regression analysis to predict mortality risk in COVID-19 patients from routine hematologic parameters. Ibnosina J Med Biomed Sci. 2020;12(2):123.
CrossRef - Wang Z, Du Z, Zhu F. Glycosylated hemoglobin is associated with systemic inflammation, hypercoagulability, and prognosis of COVID-19 patients. Diabetes Res Clin Pract [Internet]. 2020;164:108214. Available from: https://doi.org/10.1016/j.diabres.2020.108214
CrossRef - Weiner ID, Mitch WE, Sands JM. Urea and ammonia metabolism and the control of renal nitrogen excretion. Clin J Am Soc Nephrol. 2015;10(8):1444–58.
CrossRef - Uchino S, Bellomo R, Goldsmith D. The meaning of the blood urea nitrogen/creatinine ratio in acute kidney injury. Clin Kidney J. 2012;5(2):187–91.
CrossRef - Miller WG. Reporting Estimated GFR: A Laboratory Perspective. Am J Kidney Dis. 2008;52(4):645–8.
CrossRef - Su Z, Chen Z, Xiang Y, Wang B, Huang Y, Yang D, et al. Low serum levels of uric acid and albumin in patients with Guillain-Barre syndrome. Med (United States). 2017;96(15):1–5.
CrossRef - Cao X, Yin R, Albrecht H, Fan D, Tan W. Cholesterol: A new game player accelerating vasculopathy caused by SARS-CoV-2? Am J Physiol – Endocrinol Metab. 2020;319(1):E197–202.
CrossRef - Rabbani G, Ahn SN. Review: Roles of human serum albumin in prediction, diagnoses and treatment of COVID-19. Int J Biol Macromol [Internet]. 2021;193(PA):948–55. Available from: https://doi.org/10.1016/j.ijbiomac.2021.10.095
CrossRef - Zhu B, Feng X, Jiang C, Mi S, Yang L, Zhao Z, et al. Correlation between white blood cell count at admission and mortality in COVID-19 patients: a retrospective study. BMC Infect Dis. 2021;21:1–5.
CrossRef - Han H, Xu Z, Cheng X, Zhong Y, Yuan L, Wang F, et al. Descriptive, retrospective study of the clinical characteristics of asymptomatic COVID-19 patients. MSphere. 2020;5(5):10–1128.
CrossRef - Cao D, Saito S, Veiras LC, Okwan-duodu D, Bernstein EA, Giani JF, et al. Role of angiotensin-converting enzyme in myeloid cell immune responses. 2020;
CrossRef - Zhang Z. COVID-19 virus: the immune reaction to vaccines. In: Second International Conference on Biological Engineering and Medical Science (ICBioMed 2022). SPIE; 2023. p. 494–501.
CrossRef - Papamanoli A, Kalogeropoulos AP, Hotelling J, Yoo J, Grewal P, Predun W, et al. Association of serum ferritin levels and methylprednisolone treatment with outcomes in nonintubated patients with severe COVID-19 pneumonia. JAMA Netw Open. 2021;4(10):e2127172–e2127172.
CrossRef - Hulkoti VS, Acharya S, Kumar S, Talwar D, Khanna S, Annadatha A, et al. Association of serum ferritin with COVID-19 in a cross-sectional study of 200 intensive care unit patients in a rural hospital: Is ferritin the forgotten biomarker of mortality in severe COVID-19? J Fam Med Prim Care. 2022;11(5):2045.
CrossRef - Yao Y, Cao J, Wang Q, Shi Q, Liu K, Luo Z, et al. D-dimer as a biomarker for disease severity and mortality in COVID-19 patients: a case control study. J intensive care. 2020;8:1–11.
CrossRef - Katsoularis I, Fonseca-Rodríguez O, Farrington P, Jerndal H, Lundevaller EH, Sund M, et al. Risks of deep vein thrombosis, pulmonary embolism, and bleeding after covid-19: nationwide self-controlled cases series and matched cohort study. BMJ. 2022;377:e069590.
CrossRef - Yin JX, Agbana YL, Sun ZS, Fei SW, Zhao HQ, Zhou XN, et al. Increased interleukin-6 is associated with long COVID-19: a systematic review and meta-analysis. Infect Dis Poverty [Internet]. 2023;12(1):1–14. Available from: https://doi.org/10.1186/s40249-023-01086-z
CrossRef - Zhang J, Hao Y, Ou W, Ming F, Liang G, Qian Y, et al. Serum interleukin-6 is an indicator for severity in 901 patients with SARS-CoV-2 infection: a cohort study. J Transl Med. 2020;18(1):1–8.
CrossRef - Xu Y, Yang H, Wang J, Li X, Xue C, Niu C, et al. Serum albumin levels are a predictor of COVID-19 patient prognosis: Evidence from a single cohort in Chongqing, China. Int J Gen Med. 2021;2785–97.
CrossRef - Xie H, Zhao J, Lian N, Lin S, Xie Q, Zhuo H. Clinical characteristics of non‐ICU hospitalized patients with coronavirus disease 2019 and liver injury: a retrospective study. Liver Int. 2020;40(6):1321–6.
CrossRef - Guan W, Liang W, Zhao Y, Liang H, Chen Z, Li Y, et al. Comorbidity and its impact on 1590 patients with COVID-19 in China: a nationwide analysis. Eur Respir J. 2020;55(5).
CrossRef - Huang J, Cheng A, Kumar R, Fang Y, Chen G, Zhu Y, et al. Hypoalbuminemia predicts the outcome of COVID-19 independent of age and co-morbidity. J Med Virol. 2020;92(10):2152–8.
CrossRef - Zhang T, Mei Q, Zhang Z, Walline JH, Liu Y, Zhu H, et al. Risk for newly diagnosed diabetes after COVID-19: a systematic review and meta-analysis. BMC Med. 2022;20(1):1–10.
CrossRef - Balthazar JA, Chehter EZ. Acute pancreatitis and COVID-19: a new target for infection? Einstein (Sao Paulo). 2022;20(8):eRW6667.
CrossRef - Keefe JA, Avadhanula V, Nicholson EG, Devaraj S, Piedra PA, Bozkurt B, et al. Abnormalities in cardiac and inflammatory biomarkers in ambulatory subjects after COVID-19 infection. IJC Hear Vasc. 2022;43:101144.
CrossRef - García de Guadiana‐Romualdo L, Morell‐García D, Rodríguez‐Fraga O, Morales‐Indiano C, María Lourdes Padilla Jiménez A, Gutiérrez Revilla JI, et al. Cardiac troponin and COVID‐19 severity: results from BIOCOVID study. Eur J Clin Invest. 2021;51(6):e13532.
CrossRef - Shahab, Sarvazad Hc, Barghi M, Sajadi E, Sadeghian MH, Roozbahani NE. Lipid profile changes in patients with COVID-19 referred to medical centers in Kermanshah, Iran; a case–control study. J Int Med Res. 2022;50(2):03000605221078699.
CrossRef - Zhao T, Wang C, Duan B, Yang P, Wu J, Zhang Q. Altered lipid profile in COVID-19 patients and metabolic reprogramming. Front Microbiol. 2022;13:863802.
CrossRef - Guzik TJ, Mohiddin SA, Dimarco A, Patel V, Savvatis K, Marelli-Berg FM, et al. COVID-19 and the cardiovascular system: implications for risk assessment, diagnosis, and treatment options. Cardiovasc Res. 2020;116(10):1666–87.
CrossRef - Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395(10223):507–13.
CrossRef - Ramada DL, de Vries J, Vollenbroek J, Noor N, Ter Beek O, Mihăilă SM, et al. Portable, wearable and implantable artificial kidney systems: needs, opportunities and challenges. Nat Rev Nephrol. 2023;1–10.
CrossRef - Carter B, Ramsay EA, Short R, Goodison S, Lumsden J, Khan A, et al. Prognostic value of estimated glomerular filtration rate in hospitalised older patients (over 65) with COVID-19: a multicentre, European, observational cohort study. BMC Geriatr. 2022;22(1):1–8.
CrossRef - Mikami T, Miyashita H, Yamada T, Harrington M, Steinberg D, Dunn A, et al. Risk factors for mortality in patients with COVID-19 in New York City. J Gen Intern Med. 2021;36(1):17–26.
CrossRef - Gok M, Cetinkaya H, Kandemir T, Karahan E, Tuncer İB, Bukrek C, et al. Chronic kidney disease predicts poor outcomes of COVID-19 patients. Int Urol Nephrol. 2021;53(9):1891–8.
CrossRef - Gęca T, Wojtowicz K, Guzik P, Góra T. Increased risk of COVID-19 in patients with diabetes mellitus—Current challenges in pathophysiology, treatment and prevention. Int J Environ Res Public Health. 2022;19(11):6555.
CrossRef - Rajpal A, Rahimi L, Ismail‐Beigi F. Factors leading to high morbidity and mortality of COVID‐19 in patients with type 2 diabetes. J Diabetes. 2020;12(12):895–908.
CrossRef - Adane T, Asrie F, Getaneh Z, Getawa S. White blood cells and platelet profiles of diabetic patients at University of Gondar specialized referral hospital: A comparative cross‐sectional study. J Clin Lab Anal. 2021;35(6):e23808.
CrossRef - Gattinger P, Borochova K, Dorofeeva Y, Henning R, Kiss R, Kratzer B, et al. Antibodies in serum of convalescent patients following mild COVID‐19 do not always prevent virus‐receptor binding. Allergy. 2021;76(3):878.
CrossRef - Wu D, Gao S. Analysis of the lymphocyte count in type 2 diabetic patients with coronavirus disease (COVID-19): A retrospective study in a centralized treatment center. diabetes Res Clin Pract. 2020;166:108340.
CrossRef - Cheng L, Li H, Li L, Liu C, Yan S, Chen H, et al. Ferritin in the coronavirus disease 2019 (COVID-19): A systematic review and meta-analysis. J Clin Lab Anal. 2020;34(10):1–18.
CrossRef - Son NE. Influence of ferritin levels and inflammatory markers on HbA1c in the Type 2 Diabetes mellitus patients. Pakistan J Med Sci. 2019;35(4):1030–5.
CrossRef - Terpos E, Ntanasis-Stathopoulos I, Elalamy I, Kastritis E, Sergentanis TN, Politou M, et al. Hematological findings and complications of COVID-19. Am J Hematol. 2020;95(7):834–47.
CrossRef - Sardu C, D’Onofrio N, Balestrieri ML, Barbieri M, Rizzo MR, Messina V, et al. Outcomes in Patients with Hyperglycemia Affected by COVID-19: Can We Do More on Glycemic Control? Diabetes Care. 2020 May 19;43:dc200723.
CrossRef - Rehman K, Akash MSH, Liaqat A, Kamal S, Qadir MI, Rasul A. Role of interleukin-6 in development of insulin resistance and type 2 diabetes mellitus. Crit Rev Eukaryot Gene Expr. 2017;27(3).
CrossRef - Viana-Llamas MC, Arroyo-Espliguero R, Silva-Obregón JA, Uribe-Heredia G, Núñez-Gil I, García-Magallón B, et al. Hypoalbuminemia on admission in COVID-19 infection: An early predictor of mortality and adverse events. A retrospective observational study. Med Clin (Barc). 2021;156(9):428–36.
CrossRef - Nader M, Zmerli O, Platt DE, Hamdan H, Hamdash S, Abi Tayeh R, et al. Creatinine levels on admission are main modulators of COVID-19 severity. 2022;
CrossRef - Huang I, Pranata R. Lymphopenia in severe coronavirus disease-2019 (COVID-19): Systematic review and meta-analysis. J Intensive Care. 2020;8(1):1–10.
CrossRef - Ali J, Khan FR, Ullah R, Hassan Z, Khattak S, Lakhta G, et al. Cardiac troponin i levels in hospitalized COVID-19 patients as a predictor of severity and outcome: a retrospective cohort study. Cureus. 2021;13(3).
CrossRef - Durrington P. Blood lipids after COVID-19 infection. Lancet Diabetes Endocrinol. 2023;11(2):68–9.
CrossRef







