Rose Awah Bih , Maropeng Charles Monyama
, Maropeng Charles Monyama and Sogolo Lucky Lebelo*
and Sogolo Lucky Lebelo*
Department of Life and Consumer Sciences, School of Agriculture and Life Sciences, University of South Africa, Private Bag X06, Florida, South Africa.
Corresponding Author e-mail: lebelol@unisa.ac.za
DOI : https://dx.doi.org/10.13005/bpj/2771
Abstract
Traditional medicine based on the use of medicinal plants plays an important role in the preservation of health and well-being of many people globally. Today herbal medicine application is progressively finding more significance especially with the acknowledgement of the challenges of antibiotic resistance. The aim of this review was to collect literature based on the traditional application of South African medicinal plant species used in South Africa to prevent and treat various pathogenic bacterial infections. The search was carried out using key electronic scientific databases including PubMed, Google Scholar, SpringerLink, ProQuest, Science Direct, Elsevier, BioMed Central. Other sources of literature included scientific articles, book chapters, dissertations, theses and websites. It was found that Bacillus spp., Escherichia coli, Staphylococcus aureus and Pseudomonas aeruginosa were the most frequently investigated bacterial pathogens which have developed resistance to most of the available standard antibiotics. Organic and aqueous extracts of many South African plants including Acacia karroo, Psidium guajava, Punica granatum, Eucomis autumnalis, Vernonia amygdalina and Cyathula uncinulata have demonstrated potent antibacterial efficacy against the aforementioned pathogens. This review exemplifies that South African medicinal plants have the potential to be considered as new leads for the development of antibacterial agents against resistant pathogens.
Keywords
Antibiotic resistance, Antimicrobials; Human bacterial infections; Medicinal plants; South Africa
Download this article as:| Copy the following to cite this article: Bih R. A, Monyama M. C, Lebelo S. L. South African Medicinal Plants Used in the Treatment of Human Bacterial Infections: An updated Review. Biomed Pharmacol J 2023;16(4). |
| Copy the following to cite this URL: Bih R. A, Monyama M. C, Lebelo S. L. South African Medicinal Plants Used in the Treatment of Human Bacterial Infections: An updated Review. Biomed Pharmacol J 2023;16(4). Available from: https://bit.ly/49Cdo5g |
Introduction
Medicinal plants play an important role in the preservation of health and well-being of many people and animals across the globe 1-2. In the past, many people have relied on indigenous herbs with remedial actions for the prevention and treatment of infectious diseases 3. There is a growing amount of literature on the use of medicinal plants and their benefits, across the world including South Africa 4-5.
According to ethnobotanical survey, South Africa has a strong history of traditional healing and anchors a rich biodiversity of more than 30 000 plant species 6-8. However, over 4000 species are recognised to have ethnobotanical importance, with more than 3000 plants used for medicinal purposes 9-10. Notably, more than 10% of the world’s higher plant species of medicinal value grow in South Africa 7-8. Furthermore, most of these plant species are native species while a few are exotic species which were accidentally or deliberately introduced to South Africa over the years 11.
The use of medicinal plants to treat vast diseases by inhabitants of Sub-Saharan Africa is enormous so that the traditional medicine has been understood as part of African culture 12. According to researchers, medicinal plants have a myriad of diverse bioactive compounds with complex chemical profiles that contributes to their massive usage in the treatment and prevention of many diseases 7, 13, 14.These diseases include, but not limited to, asthma, diabetes, cancer, food borne diseases, nosocomial infections, mental and gynaecological problems, hypertension as well as tuberculosis 4, 15, 16.
However, the majority of the diseases are caused by organisms of bacterial origin including but not limited to Staphylococcus aureus, Escherichia coli, Mycobacterium tuberculosis, bacillus spp., Klebsiella spp., Streptococcus spp. and Pseudomonas aeruginosa 15, 17. Many scientific investigators have reported these bacterial pathogens of being resistant to a majority of the mainstream antibiotics design to kill them including those of last resort such as carbapenems, colistin, and tigecycline 18-20. Due to this phenomenon, the frail are left with no other choice but to explore medicinal herbs as an alternative means to regain health 21-23. 16, have reported the potential incorporation of traditional medicine with the Western counterparts as part of its primary healthcare approach in South Africa.
Scientific studies depicted that plants growing in South Africa have been used to remedy many bacterial infections including but not limited to diarrhoea, dysentery, skin and wound diseases, tuberculosis and pneumonia 17, 24-26. Also, 10 recounts the historical systematic use of medicinal plants in South Africa to treat bacterial diseases and the progress that has been made which could lead to future exploration of these plants as new pharmaceuticals. Today, South Africa has a good documented record of medicinal plant use to cure infectious diseases including those of bacterial origin 17. Therefore, the aim of the study was to report on South African medicinal plant used in the treatment of human bacterial infections.
Materials and methods
The search was carried out using key electronic scientific databases including PubMed, Google Scholar, SpringerLink, ProQuest, Science Direct, Elsevier, BioMed Central. Other sources of literature included scientific articles, book chapters, dissertations, theses and websites. The key words such as “medicinal plants”, “antioxidants”, “bacterial infections”, “traditional medicines”, “bioactive compounds”, and “South Africa”, were used to get the trimmed searches.
Parts of medicinal plants frequently used
It has been reported that the herbal preparations used during various treatments comes either from whole plant or from parts including the leaves, flowers, tubers, stems, roots, fruits and barks 27-28 . However, the parts of plants reported as frequently used in traditional medicine practices in South Africa includes but not limited to the ones listed below:
Bark
Tree barks are made of a hard outer layer of actively dividing living cells which functions to transport nutrients, acts as a physical barrier and protects the plant 29-30. Some researchers have reported that the barks of most medicinal plants contain substantial amounts of bioactive substances necessary to prevent and cure a variety of infections 31-32. According to 33, more than 30% of the woody plant bark used in the Limpopo province in South Africa have been reported to have high medicinal values. In South Africa, more than one third of the plant materials used in traditional medicine comes from the bark of plants 32, 34.
Leaf
The leaf of a plant is an important structure as it manufactures food that the plant needs for its growth and survival through the process of photosynthesis 35. The leaf is also fused with green substances known as chlorophyll which absorbs sunlight that aids in the conversion of carbon dioxide and water to glucose needed for plant’s growth 35. However, some of the leaves used during traditional medicine practices are known to contain bioactive substances including the leaves of Burkea Africana, Lippia javanica and Leucaena leucocephala 36-38.
Root
Plants roots help to anchor the plant to a surface by creating resistance and helps to transport substances necessary for its growth from the soil to the rest of the plant 39. In traditional medicine, the application of plant roots either independently or in combination with other plant parts is common as reported by 40-41. Research has demonstrated that most roots of plants used in traditional medicine contains important phytochemicals 42-43. Some of the plants that have their roots used as medicine includes but not limited to devil’s claw root, stinging nettle root and ginseng 42, 44.
According to 41, most traditional healers are convinced that the roots and bulbs of plants or any part hidden beneath the earth contains higher healing powers than any other plant part. In line with this, a research by 40 found out that the roots and other under-ground parts of plants holds elevated concentrations of plant natural substances. According to an ethnobotanical survey conducted by 27-28, the roots and barks are the most used and preferred over other parts by the indigenous people. Furthermore 45, was in agreement with this and reported on similar findings that the bark and roots are the most favoured parts of plants used by the Tsonga people of Mpumalanga province in South Africa, as illustrated in Figure 1.
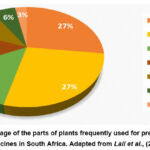 |
Figure 1: Percentage of the parts of plants frequently used for preparing traditional medicines in South Africa. Adapted from Lall et al., (2018). |
Antimicrobial ethno-medicinal plants used in South Africa
According to World Health Organisation, more than 60% of people depend on traditional medicine for the purpose of preventing and treating diseases 46. This includes 80% of the populations from underdeveloped and developing countries including South Africa 45, 47. The traditional application of medicinal plants as medicine is one of the key sources of health care in South Africa 16. Additionally, South Africa is reputable for traditional healing using medicinal plants and it is estimated that over 27 million people in both townships and the rural communities prefer and rely on traditional medicine for their primary health care 9, 45, 48. Of this, 16 reports that 72% of the population are the Black Africans including the Zulus, the Xhosa, the Bapedi, the Venda people, the Northern and the Southern Sotho people make use of traditional herbal medicine the most. A recent survey conducted by 16, on the use of natural plant products to treat human diseases in the Limpopo province of South Africa had similar findings. However, the remainder of the population including the Whites, mixed race, Indians and Chinese also use traditional medicine but at a lesser extent 49. Numerous ethnobotanical surveys done in South Africa revealed that a significant amount of plant species are used as medicine especially in regions including KwaZulu-Natal and Limpopo to relieve symptoms of bacterial, fungal and viral infections as shown in Table 2 5, 45, 50.
In addition, 27 reported on parts from one plant species frequently used during the preparation of natural product medicine than a mixture of species. However, it is logical to speculate that harvesting and using parts from one plant species especially the roots as medicine is not sustainable as the plant survival is endangered. This practice of overharvesting and exploitation can kill the plant resulting to devastating consequences including species extinction 51. This is particularly true for slow-growing and protected species 50.
Table 1 below shows the various plant species used to treat human ailments, parts, methods of preparation, parts of the plants that are commonly used, traditional therapeutic uses, and the distribution of plant in South Africa.
 |
Table 1: Plants commonly used for medicinal purposes in South Africa to treat human ailments. |
Bacterial diseases treated with indigenous medicinal plants in South Africa
It is not new that people use medicinal herbs to treat common health problems 16, 58, 92. Previously published ethnobotanical reports elucidates that some of the illnesses and/ infections commonly prevented or treated with local medicinal plants in South Africa includes, but not limited to, oral infections, heart and lung problems, sexually transmitted infections (STIs), diabetes mellitus, headaches, infertility, erectile disorder, skin problems, gastrointestinal infections including diarrhoea, Human Immunodeficiency Virus / Acquired Immune Deficiency Syndrome (HIV/AIDS) and related infections, wounds, cancer, cardiovascular diseases, respiratory ailments including coughs and tuberculosis (TB), just to name a few 12, 16, 25, 28, 32,57-58.
According to past and resent research, South Africa has an elevated level of infectious diseases burden notably from bacterial origin 5, 93; even though viral, protozoal and helminthic, as well as yeast infectious agents have also been reported 17, 94-96. This is in consistence with the research by 93, 95, 95, who reports that a larger proportion of the deaths in South Africa results from infectious diseases including tuberculosis, sexually transmitted infections (STIs) and diarrhoea.
Tuberculosis
The bacterium, Mycobacterium tuberculosis (TB) is the causative pathogen for tuberculosis which is problematic to the medical community and causes more than 1.5 million deaths in a year worldwide 89, 97. In South Africa it is estimated that 28% of TB infection burden is due to HIV it its population, thus ranking fourth largest globally 98. According to a review by 94, in the year 2013 alone South Africa recorded 860 TB cases per 100 000 people. It is worth noting that tuberculosis has been reported as the leading cause of death in South Africa 5, 65, 95.
A substantial number of studies have reported TB resistance to many pharmaceutical medications giving rise to multidrug-resistant TB (MDR-TB) and extensively drug-resistant TB (XDR-TB) 95, 99-100. However, plant natural material has been widely applied to treat TB infections due to the presence of its chemical constituents including alkaloids, glycosides, tannins, phenolics, xanthones, quinones, sterols and triterpenoids 30, 97, 101.
The Bapedi traditional healers in the Limpopo province use a variety of plants including Psiadia punctulata (DC.), Vatke and Xerophyta retinervis Baker to cure TB and its associated secondary infections 5. The Jongilanga local community in Mpumalanga also apply medicinal plants to remedy conditions of cancer, TB and acne 45. According to a research by 101, some herbs that are used by the inhabitants of the Free State Province to treat TB are active at very smaller concentrations and these includes Dicoma anomala (0.195 – 6.25 mg/ml), Hermannia depressa (0.78 – 1.56 mg/ml), Senecio harveianus (0.195 – 0.39 mg/ml) and Lotononis lanceolate (0.195 – 0.65 mg/ml).
Sexually transmitted infections (STIs)
Venereal diseases also called sexually transmitted infections (STIs) are mostly caused by bacterial pathogens including Treponema pallidum which causes syphilis, Neisseria gonorrhoeae which causes gonorrhoea and Chlamydia trachomatis which causes chlamydia infections 102-104. However viral and parasitic pathogens have been reported to also cause STIs 76, 104. It is estimated that in a year, in South Africa more than 11 million STI infections are recorded in the health registers 103, 105. The misconceptions and stigma attached to STIs in South Africa cause most of the people to favour traditional homemade remedies using medicinal plants over hospitals and local clinics visits 105. Apart from that, undesirable effects as well as resistance to most STI orthodox medications have been reported 103.
Many ethnobotanical surveys in South Africa have reported that most indigents apply a vast number of medicinal plants for the treatment of STIs including but not limited to Acacia karroo, Bidens pilosa, Carica papaya, Diospyros mespiliformis, Ficus abutilifolia, Rhoicissus tridentata subsp. cuneifolia, Ximenia caffra, Vachellia karroo, Trichilia dregeana, Terminalia sericea Cambess, Typha capensis Rohrb andZiziphus mucronata Wild. subsp. mucronata 28, 50, 68, 103-104. According to a research conducted by 104, the root extracts of Acacia karroo and Rhoicissus tridentata subsp. cuneifolia plantswere active against Neisseria gonorrhoeae with MIC value of 0.8 mg/ml and 0.4 mg/ml respectively.
Similarly, the aqueous extracts of Bidens Pilosa leaf (mean MIC 83.2 mg/ml) and Ximenia caffra root (mean MIC 62.1 mg/ml) showed inhibitory activity against Neisseria gonorrhoeae pathogen 104. Also, Trichilia dregeana produces a mean MIC of 2.0 mg/ml against Treponema pallidum 104. A review by 57, 105, agrees with this and reports on similar findings on the use of medicinal plants to treat STIs in South Africa.
Diarrhoea
According to 106, diarrhoea is a common symptom that is usually related with the disorders of the gastrointestinal tract and is typically characterised by increased in the regularity of bowel movement associated with watery stools. Infectious diarrhoea other gastrointestinal illnesses are frequently triggered by resistant strains of medically important bacteria including B. cereus, E. coli, S. aureus, Salmonella typhimurium (S. typhimurium), Proteus vulgaris (P. vulgaris), and Shigella spp., 107-108. Similarly, viral as well as parasitic diarrhoea has been reported 107. Diarrhoea has been reported as the major cause of death in low and middle income countries with over 6.9% death rate reported 108-109.
In South Africa, the indigents usually apply various medicinal plants to remedy gastrointestinal diseases and conditions associated with diarrhoea 12, 108. The pomegranate plant (Punica granatum), has been widely used to alleviate many health conditions including diarrhoea due to its rich phytochemical constituents such as flavonoids, alkaloids, saponins, tannins, phenols and anthocyanins 109-110. According to 132, the fruit peel extract of Punica granatum inhibits the growth of MRSA with zones of inhibition ranging from 22.0 mm to 11.3 mm. Similar research by 112 agrees with this and adds that the juice of pomegranate fruit shows inhibitory properties against B. cereus, E. coli, and S. aureus and produces 26.0 mm, 20.0 mm and 26.0 mm as diameter of inhibition respectively. Notwithstanding, the bark extract of Sclerocarya birrea shows activity against diarrhoeal pathogens with low MIC values including S. typhimurium (0.20 mg/ml), B. cereus (0.29 mg/ml), S. aureus (0.35 mg/ml), P. vulgaris (0.75 mg/ml) and E. coli (0.95 mg/ml) 108. On the other hand, the extract from the leaf of Psidium guajava (P. guajava) shows killing properties against B. cereus, S. typhimurium and S. aureus with MIC values of 0.34, 0.65 and 0.93 mg/ml respectively 108. Additionally, 25 had similar findings and reports on the MIC values of various medicinal plants in South Africa against diarrhoeal entero-pathogens including Aloe arborescence against S. aureus (0.018 mg/ml), Eucomis comosa against Enterococcus faecalis (0.078 mg/ml) and Acacia mearnsii against S. typhimurium (0.039 mg/ml). This is consistent with the research conducted by 113 on the use of indigenous herbal plants in South Africa to treat diarrhoea caused by enteropathogenic bacterial organisms.
In a majority of instances, reports showed that one plant can be useful in curing multiple conditions and/ diseases (mono-therapy), for example garlic scientifically known as Allium sativum, is used to treat throat infections, TB, asthma, stomach diseases 60, 62. Similarly, the cape aloe (Aloe ferox) is used in KwaZulu-Natal to remedy burns, sunburn, acne, insect bites, skin irritation, toothaches, stomach problems, sinusitis 7, 10.
Even though indigenous plants have proven very useful to mankind, however over-exploitation of these plants threatened some species to disappear or near disappear on earth 34. Due to this, the government of South Africa has introduced regulations and thus label some plants as endangered, and/or protected species including Curtisia dentata commonly called “assegai” in Afrikaans, Warburgia salutaris known as pepper-bark tree, and Zanthoxylum capense – a protected tree 34. It is interesting to note that, while some of the plants used as medicine are largely distributed in the wild or grown in gardens at home, a majority are indigenous 37. Of this, a smaller proportion are exotic and/ endemic in some parts in South Africa including Limpopo, Mpumalanga and KwaZulu Natal provinces 11.
Pathogenic bacterial infections
Infectious diseases are major cause of mortality and disability, and remain the second leading cause of death across the globe 3, 5, 114-115. This phenomenon is further exacerbated by the emergence of both old familiar and new unrecognised infectious disease pandemics 116-118. Microbial infectious diseases cause more than 50% of all the deaths that occur in the underdeveloped nations particularly African countries 3, 21, 100.
There is a rising amount of information to indicate that most of the diseases which are problematic to human health are said to be infectious and are mostly caused by pathogenic microorganisms including bacteria, viruses, parasites and fungi 95, 115, 119-120. It is of importance to note that infectious diseases occurring as a result of bacterial infections are reported to be the number one killer disease than any other category of disease globally 95, 114. These bacterial infections accounts for 43% mortality rate recorded in the underdeveloped countries whilst only 1% of the mortality rate is recorded in the developed countries 121.
The high level of infectious disease burden in a population with minimal health resources, comes with the associated ramifications including death. According to Stats 95, recorded deaths in South Africa for the period between 2014-2017 caused by infectious and parasitic diseases was 78 562 amounting to 17.2% demises. A substantial amount of health-care costs in South Africa has also been incurred as a result of infectious diseases 25.
Plants as alternative source of antimicrobials
Plants are generally known to be the biggest stores of naturally occurring biochemical compounds and are capable of manufacturing diverse natural chemical constituents including toxins and/ pheromones as a form of defence mechanism against other organisms or for pollination respectively 3, 122-123. These chemical substances are of course not placebo but are fused with low molecular weight potent bioactive constituents also known as secondary metabolites 124-125.
As early as the 1850s, plants’ secondary metabolites have received intense investigation 125-126. Currently, more than 12,000 bioactive compounds from plants have been isolated and are further classified based either on their chemical composition and structure, their biosynthetic origin or their solubility 124, 127. Due to this, the compounds were further segregated as alkaloids, terpenoids, phenolics, saponins, lipids and carbohydrates 128-129. These chemicals have promising therapeutic effects on which human beings rely on 14. The presence of these phytochemical constituents in plants perhaps explains their countless applications in traditional medicine 129-130.
The inhibitory properties of South African medicinal plants against bacterial pathogens
After unsuccessful attempts to eliminate pathogens with conventional medicines due to drug resistance, some plant secondary metabolites were considered. Numerous scientific studies have revealed significant antibacterial activities of some plants against multidrug-resistant pathogens of bacterial origin 128, 130-131 (Table 2).
According to 132; organic and aqueous extracts of Vernonia amygdalina shows antibacterial effect against Pseudomonas aeruginosa, Klebsiella spp., Streptococcus spp., Bacillus cereus, Bacillus pumilus, Bacillus subtilis, Enterobacter cloacaem, E. coli and Staphylococcus aureus. In a research conducted by 25, plant extracts from Psidium guajava, Eucomis autumnalis and Cyathula uncinulata showed promising antibacterial effect against S. aureus with minimum inhibitory concentration (MIC) values ranging from 0.018 mg/ml to 2.5 mg/ml. Correspondingly, 101 reported that the extracts from the leaves of Eucomis autumnalis was active against Bacillus pumilus, Escherichia coli and Staphylococcus aureus at a minimum inhibitory concentration (MIC) of 0.098 mg/ml, 0.130 mg/ml and 0.098 mg/ml respectively. This is in consistence with the research conducted by 105, in which the Bolusanthus speciosus bark used by the Veda indigents to treat venereal diseases showed good inhibitory activity against E. coli and S. aureus with ranges of MIC values between 0.012 mg/ml and 0.098 mg/ml. This validates the idea that plants could be used as alternative source of antibiotics.
Table 2: South African medicinal plants with promising antimicrobial activity against a variety of susceptible and resistant pathogenic strains.
|
Scientific name of Plant |
Common name of plant |
Type of extract |
Sensitive pathogen |
Reported biological ingredients |
References |
|
Allium sativum |
Garlic |
Aqueous, ethanol and chloroform extracts |
MDR-TB and XDR-TB, Escherichia coli, Salmonella typhi, Staphylococcus aureus, Streptococcus agalactiae, Klebsiella pneumoniae , Proteus mirabilis, Bacillus subtilis, Helicobacter pylori |
Allicin which is an alkaloid
|
133-134 |
|
Combretum imberbe |
Leadwood |
Acetone extract. Crude and organic extracts |
Candida albicans Cryptococcus neoformans, Schistosoma haematobium, Staphylococcus aureus, |
Triterpenoids including glycosidic derivatives of hydroxyimberbic acid, imberbic acid, glycosides based on imberbic acid |
135-137 |
|
Combretum molle |
Velvet bush willows |
Crude and organic extracts |
Bacillus cereus, Staphylococcus aureus, Escherichia coli, Pseudomonas aeruginosa |
Flavonoids Steroids Tannins Triterpenoids |
135, 138-139 |
|
Euclea divinorum |
Magic quarry |
Root-bark organic and aqueous extract
|
Bacillus subtilis, Escherichia coli, Staphylococcus aureus, Streptococcus sanguinis, Lactobacillus acidophilu |
Alkaloids Saponins Tannins Amino acids Flavonoids Phenols, Triterpenoids |
139-140 |
|
Hypericum perforatum L. |
St. John’s Wort |
Organic extract |
Staphylococcus aureus, Methicillin-resistant Staphylococcus aureus, Helicobacter pylori |
Hyperforin |
141 |
|
Punica granatum |
Pomegranate |
Peel, fruit skin and whole fruit-hot water and organic extract |
Staphylococcus aureus Escherichia coli Pseudomonas aeruginosa, Klebsiella pneumoniae, Saccharomyces cerevisiae, Salmonella typhimurium, Bacillus Subtilis, Yersinia enterocolitica. |
Polyphenols including ellagic tannins, ellagic acid, and gallic acid. Alkaloid, Flavonoid, Glycoside, Phenol, Condensed and hydrolysable tannins |
142-144 |
|
Pelargonium sidoides DC. |
Rose-scented Pelargonium OR Cape Pelargonium |
Root and leaf ethanolic and methanolic extracts |
Bacillus subtilis, Escherichia coli, Helicobacter pylori, Staphylococcus aureus, Streptococcus pneumoniae, Streptococcus epidermis, Mycobacterium tuberculosis, Mycobacterium smegmatis |
Coumarins, Flavonoids, Gallic acid, Hydroxycinnamic acid, Proanthocyanins, Phenolic acids including gallic acid |
7, 145 |
|
Schrebera alata |
Wild Jasmine |
Organic extract |
MRSA, Candida albicans, Multidrug-resistant, Pseudomonas aeruginosa, Bacillus cereus, Escherichia coli |
Flavonoids, Sterols, Alkaloids, Tannins, Quinones, Terpenoids, Saponins |
146-147 |
|
Terminalia sericea |
Silver clutter-leaf. Silver terminalia |
Organic root and leaf extracts |
Helicobacter pylori, Human immunodeficiency virus, Mycobacterium tuberculosis, Mycobacterium smegmatis, Pseudomonas aeruginosa, Staphylococcus aureus |
Alkaloids, Flavonoids, Tannins, Saponins, Phenolic acids, Lignans, Steroids, Glycosides
|
137, 148 |
|
Vernonia amygdalina |
Bitter leaf |
Organic and aqueous extracts |
Escherichia coli, Pseudomonas aeruginosa, Staphylococcus aureus |
Vernolide, Vernodalol, Vernodalin, Vernodalinol, Vernomygdin, hydrxyvernolide |
132 |
|
Ximenia caffra |
Sour-plum |
Leaf, root- organic and aqueous extract |
Neisseria gonorrhoeae, Escherichia coli Bacillus subtilis Staphylococcus aureus |
Flavonoids Tannins Polyphenols including gallic acid, catechin, quercetin and kaempferol |
105, 149-150 |
|
Zingiber officinale Roscoe |
Ginger |
Organic and aqueous extracts |
Acinetobacter baumannii, Bacillus subtilis, Bacillus cerus, Escherichia coli, Methicillin-resistant Staphylococcus aureus, |
Terpene including zingiberene, Phenols including gingerol, paradols, and shogaol |
151-152 |
Conclusion
The reviewed publications are focussed on biological activities, antioxidant and antimicrobial activities of South African plants used to treat human bacterial infections. Yet additional data and published clinical trials are still needed to confirm therapeutic properties of the researched medicinal plants. The practice of traditional medicine through the application of plant natural product still plays a vital role in fulfilling the rudimentary health care needs of the people of South Africa. Acacia karroo, Bidens pilosa, Diospyros mespiliformis and Ximenia caffra were the commonly applied herbs for the treatment of venereal diseases. On the other hand, diarrhoea and other stomach related ailments caused by pathogenic bacteria were remedied with Allium sativum, Eucomis comosa, Psidium guajava, Punica granatum and Aloe spp. Moreover, Aloe barbadensis, Cassia abbreviata, Helichrysum caespititium, Hypoxis colchicifolia and Sutherlandia frutescens were mostly used by HIV positive patients to alleviate opportunistic infections including TB, diarrhoea and skin infections. The leaves, bark and root were frequently used plant parts while the preferred methods of preparation were decoction and infusion. This study demonstrates the usefulness of plant natural product as medicine to prevent and treat human pathogenic infections caused by resistant bacteria in South Africa.
Acknowledgements
The authors would like to thank the staff members of the Department of Life and Consumer Sciences for their support in writing this paper.
Conflict of interest
The authors declare no conflict of interest.
References
- Medicinal plants: A review. J Plant Sci. 2015;3(1): 50-55.
- Azziz MA, Adnan M, Khan AH, Sufyan M, Khan SN T: Cross-cultural analysis of medicinal plants commonly used in ethnoveterinary practices at South Waziristan Agency and Bajaur Agency, Federally Administrated Tribal Areas (FATA), Pakistan. J Ethnopharmacol. 2018; 10 (21): 443-468.
- Abdallah EM. Plants: An alternative source for antimicrobials. J App Pharmaceutic Sci. 2011; 1(6):16-20.
- Prevalence and determinants of traditional, complementary and alternative medicine provider use among adults from 32 countries. Chin J Int Med. 2018;24(8): 584-590.
- Semenya SS, Maroyi A. Ethnobotanical survey of plants used by Bapedi traditional healers to treat tuberculosis and its opportunistic infections in the Limpopo Province, South Africa. S Afr J. Bot 2019; 122: 401-421.
- In vivo studies on antidiabetic plants used in South African herbal medicine. J Clin Bioc Nu. 2010; 47(2): 98-106.
- Street RA, Prinsloo G. Commercially important medicinal plants of South Africa: A review. J Chem. 2013; 1-16.
- Xego, S., Kambizi, L., Nchu, F. Threatened medicinal plants of South Africa: case of the family Hyacinthaceae. Afr J Trad Comp Alt Med. 2016; 13(3): 169-180.
- Turning folklore into an ethnomedicinal catalogue Medicinal Plants of South Africa, BE. van Wyk, B. van Oudtshoorn and N. Gericke: Book review. S Afr J Sci. 2009; 105(7): 250-250.
- van Wyk BE. The potential of South African plants in the development of new medicinal products. S Afr J Bot. 2011; 77(4): 812-829.
- Semenya SS, Maroyi A. Assessment of useful alien plant species cultivated and managed in rural home gardens of Limpopo Province, South Africa. Scientifica. 2020; 1: 3561306.
- Maroyi A. Treatment of diarrhoea using traditional medicines: contemporary research in South Africa and Zimbabwe. Afr J Trad Comp Alt Med. 2016; 13(6): 5-10
- Mahomoodally MF. Traditional Medicines in Africa: An appraisal of ten potent African medicinal plants. Evidence-based Comp Alt Med. 2013; 1:1-14.
- Alamgir ANM. 2017 Therapeutic use of medicinal plants and their extracts: Volume 1: Pharmacognosy (Vol.73). Springer International Publishing. ISBN978-3-319-63862-1 (eBook).
- Romha G, Admasu B, Aleme H, Gebru G. Antibacterial activities of five medicinal plants in Ethiopia against some human and animal pathogens. Evidence-based Comp Alt Med. 2018; 2950758-2950758.
- Mothibe ME, Sibanda M. African traditional medicine: South African perspective. In C Mordeniz (ed). Traditional and Complementary medicine 2019; 31-49 Intechopen.
- Cock IE, van Vuuren. The traditional use of southern African medicinal plants for the treatment of bacterial respiratory diseases: A review of the ethnobotany and scientific evaluations. J Ethnopharmacol. 2020; 263:113204-113204.
- AR, Halls G, Hu Y. Novel classes of antibiotics or more of the same? Brit J Pharmacol. 2011; 163(1):184-194.
- Laxminarayan R, Duse A, Wattal, C, Zaidi AK, Wertheim HF, Sumpradit N, Vlieghe E, Hara GL, Gould IM, Goossens, H et al. Antibiotic resistance—the need for global solutions. Lancet Infect Dis. 2013; 13(12): 1057-1098.
- Osei Sekyere J, Amoako DG. Carbonyl cyanide m-chlorophenylhydrazine (CCCP) reverses resistance to colistin, but not to carbapenems and tigecycline in multidrug-resistant Enterobacteriaceae. Frontiers Microb. 2017; 8:228-228.
- Chowdhury AN, Ashrafuzzaman M, Ali H, Liza LN, Zinnah KMA. Antimicrobial activity of some medicinal plants against multi drug resistant human pathogens. Adv Biosci Bioeng. 2013; 1(1): 1-24.
- Sani I. Application of medicinal plants to overcome antibiotic resistance in some selected multi-drug resistant clinical isolates. Res Rev J Pharmacog Phytochem. 2014; 2: 48-52.
- Sani I, Umar RA, Hassan SW. Potential alternatives for resolving bacterial antibiotic resistance. Eur J Pharmaceut Med Res. 2018; 5(6): 25-34.
- Bartolome, A.P., Villaseñor, I.M, Yang, W.C. Bidens pilosa L. (Asteraceae): Botanical Properties, Traditional Uses, Phytochemistry, and Pharmacology. Evidence based Comp Alt Med. 2013; 340215-340215
- Bisi-Johnson MA, Obi CL., Samuel BB, Eloff JN, Okoh AI. Antibacterial activity of crude extracts of some South African medicinal plants against multidrug resistant etiological agents of diarrhoea. BMC Comp Alt Med. 2017;17(1): 1-9.
- Maroyi A. Acacia karroo Hayne. Ethnomedicinal uses, phytochemistry and pharmacology of an important medicinal plant in southern Africa. Asian Pac J Trop Med. 2017a; 10(4):351-360.
- Semenya SS, Maroyi A. Medicinal plants used by the Bapedi traditional healers to treat diarrhoea in the Limpopo Province, South Africa. J Ethnopharmacol. 2012; 144: 395-401.
- Chauke MA, Shai LJ, Mogale MA, Tshisikhawe MP, Mokgotho MP. Medicinal plant use of villagers in the Mopani district, Limpopo province, South Africa. Afr J Trad Comp Alt Med. 2015;12(3): 9-26.
- AM, Barbosa FM, Moiane SF, Albano G, de Barros AIR. Bark Stripping from forest tree species in Madjadjane, Southern Mozambique: Medicinal uses and implications for conservation. Nat Resources.2014; 5(5): 192-199.
- Angyalossy V, Pace MR, Evert RF, Marcati CR, Oskolski AA, Terrazas T, Anochie PI, Ndingkokhar B, Bueno J, Anyiam FE et al. African medicinal plants that can control or cure tuberculosis. Int J Pharmaceut Sci Dev Res. 2018; 4(1): 001-008.
- Wintola OA, Afolayan AJ. Aspects of Medicinal Activities of the Stem Bark Extracts of Curtisia dentata (Burm. F.). Pharmacology. 2017; 13(3): 237-246.
- Khumalo GP, Sadgrove NJ, van Vuuren SF, van Wyk BE. An inventory of the most popular medicinal barks sold on Johannesburg muthi markets and the antimicrobial activity of selected extracts and isolated chemical compounds. S Afr J Bot. 2018; doi: 10.1016/j.sajb.2018.02.054.
- Tshisikhawe MP, van Rooyen MW, Bhat RB. An evaluation of the extent and threat of bark harvesting of medicinal plant species in the Venda Region, Limpopo Province, South Africa. Phyton (Buenos Aires) 2012; 81: 89-100.
- Grace OM, Prendergast H.D.V., Jäger, A.K., Van Staden, J., van Wyk, A.E. Bark medicines used in traditional healthcare in KwaZulu-Natal, South Africa: An inventory. S Afr J Bot. 2003; 69(3): 301-363.
- Yang Y, Tang M, Sulpice R, Chen H, Tian S, Ban Y. Arbuscular mycorrhizal fungi alter fractal dimension characteristics of Robinia pseudoacacia L. seedlings through regulating plant growth, leaf water status, photosynthesis, and nutrient concentration under drought stress. J Plant Growth. Reg 2014; 33(3): 612-625.
- Dzoyem JP, Eloff JN. Anti-inflammatory, anticholinesterase and antioxidant activity of leaf extracts of twelve plants used traditionally to alleviate pain and inflammation in South Africa. J Ethnopharmacol. 2015; 160:194-201.
- Asowata-Ayodele AM. Pharmacological studies of Foeniculum vulgare (mill.) and Lippia javanica (burm. F.) Spreng. used as spices in Nkonkobe Municipality of the Eastern Cape province, South Africa 2015; (Doctoral dissertation, University of Fort Hare).
- Oosthuizen CB, Gasa N, Hamilton CJ, Lall N. Inhibition of mycothione disulphide reductase and mycobacterial biofilm by selected South African plants. S Afr J Bot. 2019; 120:291-297.
- Lux A, Rost TL. Plant root research: the past, the present and the future. Ann Bot. 2012; 10(2): 201-204.
- Maroyi A. An ethnobotanical survey of medicinal plants used by the people in Nhema communal area, Zimbabwe. J Ethnopharmacol. 2011; 136 (2): 347-354.
- Masevhe NA, McGaw LJ, Eloff JN. The traditional use of plants to manage candidiasis and related infections in Venda, South Africa. J Ethnopharmacol. 2015; 168: 364-372.
- Mncwangi, N., Chen, W., Vermaak, I., Viljoen, A.M, Gericke, N. Devil’s Claw—A review of the ethnobotany, phytochemistry and biological activity of Harpagophytum procumbens. Journal of Ethnopharmacol. 2012; 143(3): 755-771.
- Masondo, N.A., Stafford, G.I., Aremu, A.O. Makunga, N.P. Acetylcholinesterase inhibitors from southern African plants: An overview of ethnobotanical, pharmacological potential and phytochemical research including and beyond Alzheimer’s disease treatment. S Afr J Bot. 2019; 120:39-64.
- Said, A.A.H., Otmani, I.S.E., Derfoufi, S, Benmoussa, A. Highlights on nutritional and therapeutic value of stinging nettle (Urtica dioica). Int J Pharmacy and Pharmaceut Sci. 2015; 7(10):8-14.
- Lall N, de Canha M, Reid A, Oosthuizen C, Langhansova L, Mahore J, Winterboer S, Hamilton C, Kumar V, Gasa N et al. Antibacterial and Anticancer Activity of Ethnomedicinal Plants Used in the Jongilanga Community, Mpumalanga. Int J Pharmacog Phytochem Res.2018; 10(1): 25-37.
- World Health Organization: Innovative care for chronic conditions: Building blocks for action. Global Report, Noncommunicable Diseases and Mental Health, World Health Organization Geneva, Switzerland 2002.
- Mintah SO, Asafo-Agyei T, Archer MA, Junior PAA, Boamah D, Kumadoh D, Appiah, A, Ocloo A, Boakye YD, Agyare C: Medicinal plants for treatment of prevalent diseases. In: Pharmacognosy-Medicinal Plants. IntechOpen. 2019. DOI: 10.5772/intechopen.82049. Available at: https://www.intechopen.com/books/pharmacognosy-medicinal-plants/medicinal-plants-for-treatment-of-prevalent-diseases
- Twilley, D., Rademan, S, Lall, N. A review on traditionally used South African medicinal plants, their secondary metabolites and their potential development into anticancer agents. J Ethnopharmacol. 2020; 261: 113101.
- Bhamra, S.K., Slater, A., Howard, C., Heinrich, M, Johnson, M.R. Health care professionals’ personal and professional views of herbal medicines in the United Kingdom. Phytotherapy Res. 2019; 33(9): 2360-2368.
- Semenya SS, Potgieter MJ, Erasmus LJC. Indigenous plant species used by Bapedi healers to treat sexually transmitted infections: Their distribution, harvesting, conservation and threats. S Afr J Bot. 2013b; 87: 66-75.
- van Wyk AS, Prinsloo G. Medicinal plant harvesting, sustainability and cultivation in South Africa. Biol. Conserv. 2018; 227: 335-342.
- Nortje JM. Medicinal ethnobotany of the Kamiesberg, Namaqualand, Northern Cape Province, South Africa (Doctoral dissertation, University of Johannesburg) 2012.
- Akhalwaya S, van Vuuren S, Patel M. An in vitro investigation of indigenous South African medicinal plants used to treat oral infections. J Ethnopharmacol. 2018; 210: 359-371.
- Balakumbahan R, Rajamani K, Kumanan K. Acorus calamus: An overview. J. Med Plants Res. 2010; 4(25): 2740-2745.
- Wojtasik EM. Richness and diversity of alien ethnomedicinal plant taxa used and sold for traditional medicine in South Africa (Doctoral dissertation, Witwatersrand University) 2014.
- Mthethwa NS. Antimicrobial activity testing of traditionally used plants for treating wounds and sores at Ongoye area KwaZulu-Natal, South Africa (Doctoral dissertation, University of Zululand) 2009.
- De Wet, H., Nzama, VN, van Vuuren, SF. Medicinal plants used for the treatment of sexually transmitted infections by lay people in northern Maputaland, KwaZulu–Natal Province, South Africa. S Afr J Bot. 2012; 78: 12-20.
- Maroyi, A. Albizia Adianthifolia: Botany, medicinal uses, phytochemistry, and pharmacological properties. Sci World J. 2018b: 7463584-4763602.
- Dyubeni L, Buwa LV. An ethnobotanical study of plants used for the treatment of ear, nose and throat (ENT) infections in Nkonkobe Municipality, South Africa. J. Med Plants Res. 2012; 6(14): 2721-2726.
- Famewo EB, Clarke AM, Afolayan AJ. Ethno-medicinal documentation of polyherbal medicines used for the treatment of tuberculosis in Amathole District Municipality of the Eastern Cape Province, South Africa. Pharmaceut Biol. 2017; 55(1): 696-700.
- Semenya SS, Maroyi A. Plants used by Bapedi traditional healers to treat asthma and related symptoms in Limpopo Province, South Africa. Evidence-based Comp Alt Med. 2018b: 2183705.
- Magwede K, van Wyk BE, van Wyk AE. An inventory of Vhavenḓa useful plants. S Afr J Bot. 2019; 122: 57-89.
- Sahu PK, Giri DD, Singh R, Pandey P, Gupta S, Shrivastava AK, Kumar A, Pandey KD. Therapeutic and medicinal uses of Aloe vera: A review. Pharmacol. Pharma. 2013; 4(8), 599-610.
- Klopper RR, Crouch NR, Smith GF, van Wyk AE. A synoptic review of the aloes (Asphodelaceae, Alooideae) of KwaZulu-Natal, an ecologically diverse province in eastern South Africa. PhytoKeys. 2020; 142(1):1-89.
- McCray T. The anti-mycobacterial properties of South African medicinal plants. (Doctoral dissertation, Cornell University) 2013.
- Arthur GD, Naidoo KK, Coopoosamy RM. Bidens pilosa L.: agricultural and pharmaceutical importance. J Med Plants Res. 2012; 6: 3282-3287.
- Cheesman L, Nair JJ, van Staden J. Antibacterial activity of crinane alkaloids from Boophone disticha (Amaryllidaceae). J Ethnopharmacol. 2012; 140(2): 405-408.
- Nair, J.J., Van Staden, J., Bonneta, S.L, Wilhelm, A. Distribution and Diversity of Usage of the Amaryllidaceae in the Traditional Remediation of Infectious Diseases. Nat Prod Comm. 2019; 12(4), pp.635-639.
- Mahwasane ST, Middleton L, Boaduo N. An ethnobotanical survey of indigenous knowledge on medicinal plants used by the traditional healers of the Lwamondo area, Limpopo province, South Africa. S Afr J Bot. 2013; 8: 69-75
- York T, de Wet H, van Vuuren SF. Plants used for treating respiratory infections in rural Maputaland, KwaZulu-Natal, South Africa. J Ethnopharmacol. 2011; 135(3): 696-710.
- Mabona U, van Vuuren SF. Southern African medicinal plants used to treat skin diseases. S Afr J Bot. 2013; 87:175-193.
- Lewu FB, Afolayan AJ. Ethnomedicine in South Africa: The role of weedy species. Afr J Biotech. 2009;8(6):929-934.
- Kudumela, R.G., McGaw, LJ, Masoko, P. Antibacterial interactions, anti-inflammatory and cytotoxic effects of four medicinal plant species. BMC Comp Alt Med. 2018; 18(1):1-7.
- Doughari HJ, Ndakidemi PA, Human IS, Benade S. Curtisia dentata: Ethnopharmacological application. J Med Pants Res. 2011;5(9):1606-1612
- Muhali MD. Environmental resource utilization: a case study of traditionally useful wild plant species in the Makhado Local Municipality (Doctoral dissertation, University of Johannesburg) 2017.
- Kudumela RG, Mazimba O, Masoko P. Isolation and characterisation of sesquiterpene lactones from Schkuhria pinnata and their antibacterial and anti-inflammatory activities. S Afr J Bot. 2019; 126(1): 340-344.
- Maroyi A. Dombeya rotundifolia (Hochst.) Planch.: review of its botany, medicinal uses, phytochemistry and biological activities. J Comp Med Res. 2018a; 9(3): 74-82.
- Shirinda H, Leonard C, Candy G, van Vuuren S. Antimicrobial activity and toxicity profile of selected southern African medicinal plants against neglected gut pathogens. S Afr J Sci. 2019; 115(11-12): 1-10.
- Mwihaki Ng’ang’a M, Hussain H, Chhabra S, Langat-Thoruwa C, Al-Harrasi A, Krohn K, Green IR. Eucleanal A and B: Two new napthalene derivatives from Euclea divinorum. Chin. Chem. Letters 2012);23(5): 576-578.
- Sharma R: Antibacterial and anti-inflammatory activity of Syzygium jambos and Leucosidea sericea in addressing acne vulgaris (Doctoral dissertation, University of Pretoria) 2014.
- Maroyi A. Review of ethnomedicinal uses, phytochemistry and pharmacological properties of Euclea natalensis A. DC. Molecules. 2017b; 22(12): 2128.
- Constant NL, Tshisikhawe MP. Hierarchies of knowledge: ethnobotanical knowledge, practices and beliefs of the Vhavenda in South Africa for biodiversity conservation. J Ethnobiol Ethnomed. 2018; 14(1): 56-56.
- Badgujar S., Pate VV, Bandivdekar AH, Mahajan RT. Traditional uses, phytochemistry and pharmacology of Ficus carica: A review. Pharmaceut. Biol 2014; 52(11): 1487-1503.
- Ng’uni T, Klaasen JA, Fielding BC. Acute toxicity studies of the South African medicinal plant Galenia africana. Toxicol Reports. 2018; 5: 813-818.
- Mugomeri E, Chatanga P, Chakane N. Medicinal herbs used by HIV-positive people in Lesotho. Afr J Trad Comp Alt Med. 2016;13(4):123-131.
- Dixit S, Tripathi A, Kumar P: Medicinal properties of Moringa oleifera: A review. Int J Ed Sci Res Rev. 2016; 3(2):173-185.
- Bassey K, Semenya A, Mabowe M, Mabuza M. South African Moringa oleifera Lam: A review of its phytochemistry, commercialization and quality control. Int J Med Plants Nat Prod. 2018; 4: 5-35.
- Gororo M, Chimponda T, Chirisa E, Mukanganyama S. Multiple cellular effects of leaf extracts from Parinari curatellifolia. BMC Comp Alt Med. 2016;16(1): 305-305.
- Madikizela B, Kambizi L, McGaw LJ. An ethnobotanical survey of plants used traditionally to treat tuberculosis in the eastern region of OR Tambo district, South Africa. S Afr J Bot. 2017; 109:231-236.
- Kamatou GPP, Viljoen AM, Steenkamp P. Antioxidant, anti-inflammatory activities and HPLC analysis of South African Salvia species. Food Chem. 2010; 119(2): 684-688.
- Naidoo D, Slavětínská LP, Aremu AO, Gruz J, Biba O, Doležal K, van Staden J, Finnie JF. Metabolite profiling and isolation of biologically active compounds from Scadoxus puniceus, a highly traded South African medicinal plant. Phytother Res. 2018; 32(4): 625-630.
- SY, Litscher G, Gao SH, Zhou SF, Yu ZL, Chen HQ, Zhang SF, Tang MK, Sun JN, Ko KM. Historical perspective of traditional indigenous medical practices: the current renaissance and conservation of herbal resources. Evidence-based Comp Alt Med 2014:525340.
- Roomaney RA, Pillay-van Wyk V, Awotiwon OF, Dhansay A, Groenewald P, Joubert JD, Nglazi MD, Nicol E, Bradshaw D. Epidemiology of lower respiratory infection and pneumonia in South Africa (1997–2015): A systematic review protocol. Brit Med J Open 2016; 6(9): e012154.
- McCarthy KM, Scott LE, Gous N, Tellie M, Venter WDF, Stevens WS, van Rie A. High incidence of latent tuberculous infection among South African health workers: an urgent call for action. Int J Tuber Lung Dis. 2015; 19(6): 647-653.
- Stats SA. Mortality and causes of death in South Africa, 2017: Findings from death notification 2017. Date of Accessed: 20 July 2020. Available at: http://www.statssa.gov.za/publications/P03093/P030932017.pdf
- Schwartz IS, Boyles TH, Kenyon CR, Hoving JC, Brown GD, Denning DW. The estimated burden of fungal disease in South Africa. S Afr Med J. 2019; 109(11): 885-892.
- Anochie PI, Ndigkokhar B, Bueno J, Anyiam FE, Ossai-Chidi LN, Onyeneke CC, Onyeozirilla AC. African medicinal plants that can control or cure tuberculosis. Int J Pharm Sci Dev Res. 2018; 4 (1): 001-008.
- Ismail NA, Mvusi L, Nanoo A, Dreyer A, Omar SV, Babatunde S, Molebatsi T, van der Walt M, Adelekan A, Deyde, V et al. Prevalence of drug-resistant tuberculosis and imputed burden in South Africa: a national and sub-national cross-sectional survey. Lancet Infect Dis. 2018; 18(7): 779-787.
- Palomino JC, Martin A. Drug resistance mechanisms in Mycobacterium tuberculosis. Antibiotics. 2014; 3(3): 317-340.
- A, Sifri Z, Cennimo D, Horng H. Global contributors to antibiotic resistance. J Global Infect Dis. 2019; 11(1): 36-42.
- Bioactivity of traditional medicinal plants used in the treatment of tuberculosis in the Free State, South Africa (Doctoral dissertation, University of the Free State (Qwaqwa Campus) 2016.
- van Vuuren SF, Naidoo D: An antimicrobial investigation of plants used traditionally in southern Africa to treat sexually transmitted infections. J Ethnopharmacol. 2010; 130(3): 552-558.
- Mamba PB: Bioactivity of selected medicinal plants used for the treatment of sexually transmitted diseases (Doctoral dissertation, University of Pretoria) 2017.
- M, Abbaszadeh S, Darvishi M, Kheirollahi A, Shahsavari S, Moghadasi M. The most important herbs used in the treatment of sexually transmitted infections in traditional medicine. Sudan J Med Sci. 2019; 14(2): 41-6.
- Govender L, Eche M. Health-seeking behaviour of people with sexually transmitted infections in the community of Nkomazi East, Mpumalanga: original research. S Afr J Epidemiol Iinfect. 2012; 27(4):195-198.
- World Health Organisation Factsheet: 2017 Diarrhoeal disease. http://www.who.int/news-room/fact-sheets/detail/diarrhoeal-disease. Date of Accessed: 08 October 2020.
- Kullin B, Meggersee R, D’Alton J, Galvao B, Rajabally N, Whitelaw A, Bamford C, Reid SJ, Abratt VR. Prevalence of gastrointestinal pathogenic bacteria in patients with diarrhoea attending Groote Schuur Hospital, Cape Town, South Africa. S Afr Med J. 2015; 105(2):121-125.
- van Vuuren, S.F., Nkwanyana, M, de Wet, H. Antimicrobial evaluation of plants used for the treatment of diarrhoea in a rural community in northern Maputaland, KwaZulu-Natal, South Africa. BMC Comp Alt Med. 2015; 15(1):53-53.
- World Health Organisation (WHO): Diarrhoea disease 2010. Available at: http://www.who.int/mediacentre/factsheets/fs330/en/. Date of Accessed: 10 November 2020.
- Jayaprakash A, Sangeetha R. Phytochemical screening of Punica granatum Linn. peel extracts. J Acad Ind Res. 2015;4(5): 160-162.
- Chebaibi A, Filali FR. Bactericidal activity and phytochemical screening of Moroccan pomegranate (Punica granatum Linn.) peel aqueous extracts. J Med Plants Res. 2013; 7(14): 887-891.
- Dahham SS, Ali MN, Tabassum H, Khan M. Studies on antibacterial and antifungal activity of pomegranate (Punica granatum L.). American-Eur J Agric Environ Sci. 2010; 9(3): 273-281.
- De Wet H, Nkwanyana MN, van Vuuren SF. Medicinal plants used for the treatment of diarrhoea in northern Maputaland, KwaZulu-Natal Province, South Africa. J Ethnopharmacol. 2010; 130(2):284-289
- Viswanathan, R. and Arafath, M.M: Study of Clinical Profile of Stroke in a Tertiary Care Centre–A Retrospective Study. Int J Scie Stu. 2021; 8(10): 182-185.
- Lindahl JF, Grace D. The consequences of human actions on risks for infectious diseases: a review. Infect Ecol Epidemiol. 2015; 5(1): 30048
- Nii-Trebi NI. Emerging and neglected infectious diseases: Insights, advances, and challenges. Biomed Res Int. 2017:5245021-5245021
- Sikandar S. Emergence and Re-Emergence of Infectious Diseases: Perpetual Threat to Public Health WorldWide. Lahore Garrison University J Life Sci2018; 2(3): 210-217
- Docea AO, Tsatsakis A, Albulescu D, Cristea O, Zlatian O, Vinceti M, Moschos SA, Tsoukalas D, Goumenou M, Drakoulis N et al. A new threat from an old enemy: Re‑emergence of coronavirus. Int J Mol Med. 2020; 45(6): 1631-1643
- Köhler JR, Casadevall A, Perfect J. The spectrum of fungi that infects humans. Cold Spring Harbor Perspectives Med. 2015; 5(1): a019273
- Oryan A, Akbari M. Worldwide risk factors in leishmaniasis. Asian Pac. J. Trop. Med. 2016; 9(10): 925-932
- 121. Kimutai N, Ogutu PA, Jeruto CMP. Ethnobotanical study of selected medicinal plants used against bacterial infections in Nandi county, Kenya. J Med Plants. 2019; 7(4):103-108
- Ramakrishna A, Ravishankar GA. Influence of abiotic stress signals on secondary metabolites in plants. Plant Signaling Behav. 2011; 6(11): 1720-1731
- Lara MV, Bonghi C, Famiani F, Vizzotto G, Walker RP, Drincovich MF. Stone fruit as biofactories of phytochemicals with potential roles in human nutrition and health. Frontiers Plant Sci. 2020; 11:1323
- Katz L, Baltz RH. Natural product discovery: past, present, and future. J Ind Microb Biotech.2016; 43(2-3): 155-176
- Anand U, Jacobo-Herrera N, Altemimi A, Lakhssassi N. A comprehensive review on medicinal plants as antimicrobial therapeutics, potential avenues of biocompatible drug discovery. Metabolites. 2019; 9 (11):258.
- Veeresham C. Natural products derived from plants as a source of drugs. J Adv Pharmaceut Tech Res. 2012; 3(4): 200-201
- O’Connor SE. Engineering of secondary metabolism. Ann Rev Gen. 2015; 49: 71-94.
- Jackueline I. Antimicrobial activity, acute toxicity and phytochemical composition of four medicinal plants traditionally used in Sotik Sub-county Kenya. (Doctoral dissertation, University of Nairobi. Kenya) 2015.
- RA, El-Anssary AA. Plants Secondary Metabolites: The Key Drivers of the Pharmacological Actions of Medicinal Plants. In. Herbal Medicine. IntechOpen 2018. DOI: 10.5772/intechopen.76139.
- Wink M. Modes of action of herbal medicines and plant secondary metabolites. Medicines. 2015; 2(3): 251-286.
- Hasan M, Ali Redha A, Mandeel Q. Phytochemical investigations of pomegranate (Punica granatum) rind and aril extracts and their antioxidant, antidiabetic and antibacterial activity. Nat Prod Chem Res. 2018: 6(4): 332-342.
- Adetunji CO, Olaniyi OO, Ogunkunle ATJ. Bacterial activity of crude extracts of Vernonia amygdalina on clinical isolates. J Microb Antimicrob. 2013; 5(6): 60-64.
- Hannan A, Ullah MI, Usman M, Hussain S, Absar M, Javed K. Anti-mycobacterial activity of garlic (Allium sativum) against multi-drug resistant and non-multi-drug resistant Mycobacterium tuberculosis. Pak J Pharmaceut Sci. 2011; 24(1): 81-85.
- Mikaili P, Maadirad S, Moloudizargari M, Aghajanshakeri S, Sarahroodi S. Therapeutic uses and pharmacological properties of garlic, shallot, and their biologically active compounds. Iranian J Bas Med Sci. 2013; 16(10):1031.
- A, Pierre S, Tsala DE, Habtemariam S. Phytochemical constituents of Combretum Lofl.(combretaceae). Pharmaceut. Crops 2013; 4: 38-59.
- Roy S, Gorai D, Acharya R, Roy R. Combretum (combretaceae): Biological activity and phytochemistry. Amer J Pharm Res. 2014; 4(11): 5266-5299.
- Mapiye S. Analysis of antibacterial activity of Terminalia Sericea and Combretum imberbe two combretaceae species from Namibia (Doctoral dissertation, University of Namibia) 2019.
- Diale MO, Ubomba-Jaswa E, Serepa-Dlamini MH. The antibacterial activity of bacterial endophytes isolated from Combretum molle. Afr J Biotech. 2018; 17(8): 255-262.
- Ngari FW, Gikonyo NK, Wanjau RN, Njagi EM. Safety and Antimicrobial Properties of Euclea divinorum Hiern, Chewing Sticks Used for Management of Oral Health in Nairobi County, Kenya. J Pharmaceut Biomed Sci. 2013; 3(3): 1-8.
- Nyambe MM, Hans R, Beukes M, Morris J, Kandawa-Schulz M. Phytochemical and antibacterial analysis of indigenous chewing sticks, Diospyros lyciodes and Euclea divinorum of Namibia. Biofarmasi J Nat Prod Bioc. 2018; 16:29-43.
- Özkan EE, Çelik BÖ, Afife MAT. Antimicrobial activities of five endemic Hypericum species from Anatolia compared with Hypericum perforatum. Marmara Pharmaceut J 2019; 23:114-119.
- Nuamsetti T, Dechayuenyong P, Tantipaibulvut S: Antibacterial activity of pomegranate fruit peels and arils. Sci Asia 2012; 38(3): 319-22.
- Rahmani AH, Alsahli MA, Almatroodi SA. Active constituents of pomegranates (Punica granatum) as potential candidates in the management of health through modulation of biological activities. Pharmacog J. 2017; 9(5): 689-695.
- Hanani ZN, Yee FC, Nor-Khaizura MAR. Effect of pomegranate (Punica granatum L.) peel powder on the antioxidant and antimicrobial properties of fish gelatin films as active packaging. Food Hydrocol. 2019; 89: 253-259.
- Kolodziej H. Antimicrobial, antiviral and immunomodulatory activity studies of Pelargonium sidoides (EPs® 7630) in the context of health promotion. Pharmaceuticals. 2011; 4(10): 1295-1314.
- Chola L, Michalow J, Tugendhaft A, Hofman K. Reducing diarrhoea deaths in South Africa: costs and effects of scaling up essential interventions to prevent and treat diarrhoea in under-five children. BioMed Central Pub Health. 2015; 15(1): 394-394.
- Mongalo NI, McGaw LJ, Segapelo TV, Finnie JF, van Staden J. Ethnobotany, phytochemistry, toxicology and pharmacological properties of Terminalia sericea Burch. ex DC. (Combretaceae)–A review. J Ethnopharmacol. 2016; 194:789-802.
- Nair JJ, Mulaudzi RB, Chukwujekwu JC, van Heerden FR, van Staden J. Antigonococcal activity of Ximenia caffra Sond.(Olacaceae) and identification of the active principle. S Afr J. Bot 2013; 86, 111-115.
- Zhen J, Guo Y, Villani T, Carr S, Brendler T, Mumbengegwi DR, Kong AN, Simon J, Wu Q. Phytochemical analysis and anti-inflammatory activity of the extracts of the african medicinal plant Ximenia caffra. J Analyt Met Chem. 2015: 948262.
- Prasad S, Tyagi AK. Ginger and its constituents: role in prevention and treatment of gastrointestinal cancer. Gastro Res Pract. 2015: 142979.
- Abdalla WE, Abdalla EM. Antibacterial activity of ginger (Zingiber officinale Rosc.) rhizome: A mini review. Int J Pharmacog Chin Med. 2018; 2(4): 1-8.







