Prabhavathi K* , KalyaniPraba P
, KalyaniPraba P , Bhavsar Nikhil Rajendra
, Bhavsar Nikhil Rajendra , Ayyavoo Saravanan
, Ayyavoo Saravanan
Department of Physiology, SRM Medical College, Potheri, Chennai. Tamil Nadu India.
Corresponding Author E-mail:prabhashruti@gmail.com
DOI : https://dx.doi.org/10.13005/bpj/2782
Abstract
Background: Women with premenstrual syndrome are known to experience high negative emotions which is known to drastically affect cognition and psychomotor performance thereby impairing their executive function. Objective: To assess the relationship between cognition and psychomotor skill with self-reported symptoms of negative emotions like depression, anxiety and stress in women with different grades of premenstrual syndrome. Methodology: Study was conducted among 100 female nursing students in the age group 18 -20 years. Data collection tool included a questionnaire of demographic and menstruation characteristics, Menstrual Distress Questionnaire (MDQ), and Depression, Anxiety, and Stress Scale Questionnaire (DASS). Cognition and psychomotor performance were assessed based on reaction time (both visual & auditory) using PC1000Hz Reaction timer. The study received ethical approval from the Institutional Ethical Committee. Every participant gave their informed written consent before participating in the study. Results: Among the 100 female students, 50 each belonged to mild and moderate PMS category. Independent t test revealed a significantly high DASS scores and reaction time scores (both visual & auditory) in mild when compared to moderate PMS category. A favourable association between the severity of PMS and depression, anxiety and stress scores (DASS), and reaction time (RT) scores was discovered using the Pearson correlation test, with p significant at 0.01. Additionally, there was a substantial positive association between DASS scores and RT duration. This suggests that, as there is an increase in the severity of PMS, there was an increase in the negative emotional states scores and increase in the RT duration (both visual and auditory) thereby proving a decline in cognition and psychomotor execution. Conclusion: The results demonstrated that, woman with PMS had high negative emotion effects leading to decline in cognition and psychomotor execution which is a need of the hour to look into their lifestyle modification and treatment modality so as enhance the executive performance.
Keywords
Cognition; Negative Emotion; Premenstrual Syndrome; Psychomotor Performance
Download this article as:| Copy the following to cite this article: Prabhavathi K, KalyaniPraba P, Rajendra B. N, Saravanan A. Cognition and Psychomotor Performance in Premenstrual Syndrome with Negative Emotions. Biomed Pharmacol J 2023;16(4). |
| Copy the following to cite this URL: Prabhavathi K, KalyaniPraba P, Rajendra B. N, Saravanan A. Cognition and Psychomotor Performance in Premenstrual Syndrome with Negative Emotions. Biomed Pharmacol J 2023;16(4). Available from: https://bit.ly/3Qqajg9 |
Introduction
Premenstrual syndrome (PMS) is a collection of ill-defined symptoms and indicators that appear before menstruation and then disappear once menstruation begins. The most important reason quoted behind PMS in several studies is the physiological disturbances in the hormonal homeostasis occurring in the secretory phase of the menstrual cycle. The most common presentation of PMS 1 include irritability, mood swings, anxiety, depression, social isolation stress, fatigue 2 weight gain, sore breasts, low back ache, skin eruptions, palpitation, headache, nausea, vomiting, abdominal pain 3 . Most of the emotional symptoms were predominantly negative like depression, anxiety, stress, irritability, anger etc. The prevalence of PMS manifestation has been reported to be over 60% 4 and 23-67 percent 5 in other research. These unpleasant emotional states not only damage one’s quality of life, but they are also the leading cause of school absenteeism among adolescents and teenagers 6. Further menstruation indicators are more common in Asian countries than in Western countries, according to a World Health Organization (WHO) report 7 . Also, studies have proved that negative emotions affect the cognition and psychomotor performance thereby impairing their executive function.
Studies have revealed that hormone fluctuation that occurs throughout the menstrual cycle causes women to experience negative emotions, which in turn impacts their cognition and psychomotor performance 8 altering their executive function, a fact that has not been fully researched. Further the results from various studies shows inconsistent reporting, either no difference 9 or only subtle differences 10, 11. So, in this study, we looked into the co relation between the negative emotions (anxiety, depression, stress) and cognition in different grades of women with PMS. Reaction time test being a simple non-invasive tool that assess cognition as well as psychomotor performance 12, was used in this study.
Materials and Methods
The study was conducted on 100 female nursing students in the age group 18 -20 years. Questionnaire tool was used to collect data on demographic and menstruation characteristics, Menstrual Distress and Depression, Anxiety, and Stress (DASS). The menstrual misery was assessed using the Rudolf Moos questionnaire 13 . This questionnaire contains 16 questions in four dimensions [pain, control, autonomic reactions, and (water) weight gain and records menstrual signs a week before menstruation, during bleeding, and a week after menstruation in the previous year on a four-point Likert scale (no sign = 0, very severe = 4). Minor menstruation indications receive a score of 16, moderate menstruation signals receive a score of 32, and acute menstruation signs receive a score of 33. Scores of 49 or higher are considered severe menstrual symptoms 14 .
The DASS questionnaire was used to examine negative emotions such as depression, anxiety, and tension. This survey has 21 questions that assess depression, anxiety and stress with seven questions for each. The questions are graded on a four-point Likert scale ranging from “never” (zero) to “very much” (three). Questions 17, 16, 13, 10, 5, and 3 dealt with depression; questions 20, 19, 15, 9, 7, 4, and 2 dealt with anxiety; while questions 18, 14, 12, 11, 8, 6, and 1 dealt with stress. A score of 5-6 indicated light depression, 7-10 moderate depression, 11-13 acute depression, and over 14 indicated severe depression.
Minor anxiety received a score of 4-5, moderate 6-7, acute anxiety 8-9, and severe anxiety received a score of over 10. Minor stress was scored 8-9, moderate 10-12, acute 13-16, and extremely acute stress was scored beyond 17. Menstruation distress questionnaires and depression, anxiety, and stress scales are robust and trustworthy tools that have been utilised in Kordi (2011) and Mollahadi (2011) investigations (2010) 15. Cognition and psychomotor performance were assessed based on reaction time (both visual & auditory) using PC1000Hz Reaction timer. The study excluded students who had a history of hearing or vision loss, cardiovascular or respiratory problems, or were taking medication that affected their cognitive ability. The study received ethical approval from the Institutional Ethical Committee. Every subject gave their informed written consent before participating in the study. The PC1000Hz Reaction timer was used to measure auditory and visual reaction times.
1)Visual reaction time measurement: The Examiner hits the ‘start’ button in component (A) while the subject is told to press the ‘Stop’ button in component (B) with the right index finger first as soon as she sees the red light in the instrument. The data are analysed when the reaction time is recorded in audacity programme.
2) Auditory reaction time measurement: The Examiner clicks the start button (A), which is hidden from the subject’s view, while the subject is directed to press the stop button (B) as soon as she hears the sound (1000 hertz tone) through the headphone. The data are analysed when the reaction time is recorded using audacity programme.
All subjects must be right-handed and hit the switch to halt the equipment’ quartz clock using their right index finger. When each subject saw the light or heard the music, they were asked to press the switch. Both VRT and ART measurements require at least five trials. The final VRT and ART are determined from the minimum time recorded. The readings were taken in a quiet, secluded room between 10 a.m. and 12 p.m.
Statistical Analysis
In the current study, descriptive statistical analysis was used. Continuous measurement results are reported as Mean SD. The significance is determined at a 5% level of significance. Pearson correlation test was done between the severity of PMS and negative emotions like depression, anxiety and stress scores (DASS) and reaction time (RT) scores 16. Also, a correlation test was done between DASS and RT. Significance is assessed at 5% level of significance.
Results
Among the 100 female students, 50 each belonged to mild and moderate PMS category. Independent t test revealed a significant difference in the DASS scores and reaction time scores (both visual & auditory) in mild and moderate PMS category, i.e. the scores were higher in moderate category when compared to mild (table 1). The intensity of PMS and depression, anxiety and stress scores (DASS), and response time (RT) scores all showed a positive correlation with p significant at 0.01 in a Pearson correlation test (Fig 1). Figure 1 explains that as the intensity of premenstrual syndrome increases, the severity of depression, anxiety and stress also increases. Further as the severity of premenstrual syndrome increases, the auditory and visual reaction time score also increases indicating decreased reaction time thereby decreased cognition. In addition, there was a strong positive correlation between DASS scores and RT duration that is as severity of depression, anxiety and stress increased, there was an increase in reaction time duration (table 2 & 3). This suggests that, as there is an increase in the severity of PMS, there was an increase in the negative emotional states score which could have been the cause for increase in the RT duration (both visual and auditory) thereby proving a cognitive decline as the reaction time was used as a tool to assess cognition.
Table 1: DASS and RT scores in mild & moderate PMS
|
Moos |
N |
Mean |
SD |
correlation |
p value |
|
|
Depression |
1 |
50 |
4.36 |
4.08 |
0.632 |
0.001*** |
|
2 |
50 |
13.56 |
6.94 |
|||
|
Anxiety |
1 |
50 |
5.68 |
4.07 |
0.571 |
0.001*** |
|
2 |
50 |
13.76 |
7.24 |
|||
|
Stress |
1 |
50 |
6.66 |
4.36 |
0.577 |
0.001*** |
|
2 |
50 |
14.86 |
7.05 |
|||
|
VRT |
1 |
50 |
163.14 |
17.41 |
0.633 |
0.001*** |
|
2 |
50 |
203.60 |
30.74 |
|||
|
ART |
1 |
50 |
165.72 |
16.15 |
0.474 |
0.001*** |
|
2 |
50 |
191.46 |
30.11 |
*** – p ≤ 0.001 highly significant
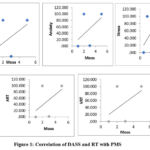 |
Figure 1: Correlation of DASS and RT with PMS. |
Table 2: Correlation of DASS with VRT scores
|
VRT |
Correlation |
p value |
|
|
Depression |
100 |
0.348 |
0.01** |
|
Anxiety |
100 |
0.369 |
0.01** |
|
Stress |
100 |
0.319 |
0.01** |
Table 3: Correlation of DASS with ART scores
|
ART |
Correlation |
p value |
|
|
Depression |
100 |
0.243 |
0.05* |
|
Anxiety |
100 |
0.188 |
NS |
|
Stress |
100 |
0.265 |
0.01** |
Discussion
Premenstrual syndrome is defined by a wide range of symptoms, mostly mood-related, but also embracing a wide range of other systems that occur in tandem within the two weeks preceding menstruation. It is inherited and lasts into adulthood 17. It is identified in 30–40% of females, with less than 10% of those who are severely affected 18. Further statistics reveal that girls are affected more than boys after puberty with anxiety and depression owing to premenstrual syndrome 19 . Thus, there is growing association of PMS with negative emotional states like depression, stress, anxiety 20. Accordingly, women were consistently more restless, irritable, fatigued, fearful, depressed and hypersensitive to various stimuli during the premenstrual period than during other phases of the menstrual cycle 21. During the luteal phase of menstrual cycle, women suffering from PMS reported significantly higher scores in depression, anxiety, and stress when compared to women without PMS 22, the results of which are comparable to our study as well. Also self-reported studies have evaluated predominantly negative emotions during premenstrual phase 23, 24 and it was found to be recurrent and noticeable in 95% cases 25 which is in par with our study too. Mid-cycle phase of menstrual cycle brings the highest levels of happiness and self-esteem, while premenstrual brings the most negative emotions (depression, anxiety, and stress) when oestrogen and progesterone levels fall. Hormone fluctuations promote unpleasant feelings in women and can alter mood management and stress sensitivity 26 which we did not evaluate in our study. Women, in particular, have greater stress responses before menstruation or during the luteal phase, which may raise the likelihood of unpleasant emotions or moods 27. Also, many research studies have confirmed increased risk of suicidal attempts during the premenstrual phase 28, 29. The authors of the above studies have reported that the cause could be due to low circulating levels of estrogenic and serotonergic mechanism 30. The autonomic nervous system may also play a role in mood cycling in women that is linked to hormonal changes, particularly during the premenstrual period 18 . Thus, an increased sympathetic nervous system activity may be responsible for negative emotions in women with premenstrual syndrome 31 . Women with PMS are most sensitive to changes in sex hormone levels 32. Variations in hormone levels during the menstrual cycle cause women to experience more negative feelings 8, 9, 33. Women, in particular, have greater stress responses before menstruation.
Estrogen receptors are found throughout the brain and have been shown to alter neurocognition 34. It directs and modulates neurotransmitter production and action, regulating electrical excitability and synaptic function, and changing the morphological properties of neuronal components involved in function 35. It has been shown to impact a variety of neurotransmitter systems, including dopaminergic, catecholaminergic, serotonergic, cholinergic, and gamma-aminobutyric acidergic 22, 36. Thus, decrease in estrogen levels during luteal phase in PMS alters neurocognition. Also, studies on postmenopausal women have shown that there is mood and behavioural disturbances with cognitive decline due to sudden estrogen withdrawal 37. However, experiments in postmenopausal women with estrogen replacement has shown to increase verbal IQ scores after one year of treatment. Further, studies have shown that estrogen administration after surgical menopause improved memory, abstract reasoning, and reaction times, while those patients who were given placebo had significant deterioration of cognitive function 34. Studies have shown that female performance on cognitive tasks vary significantly over time, scoring being less during mid-luteal phase of the menstrual cycle 38 Attention, concentration, semantic processing in word-matching tests , visual and verbal memory, speed and fine motor skills are decreased in premenstrual phase 39,40 . However in our study we have not evaluate the hormonal correlation, which is the future scope of our study. Further negative affective states such as depression, anxiety, stress appears to lead to poor decision making, executive function thereby affecting cognition and psychomotor skills. Thus, women with PMS are known to suffer from negative emotions thereby leading to cognitive decline and psychomotor skill.
Limitation of the study
Since hormonal fluctuation is found to be one of the main reason for negative emotions during PMS, their evaluation and correlation would be of much useful information and strength to this study which will be undertaken as a study in future. Also increased sympathetic activity during PMS leading to negative emotions thereby causing a decline in cognition will also assessed in future using tools like heart rate variability and autonomic function testing.
Conclusion
The present study concluded that the negative emotions were very much prevalent in the premenstrual syndrome. As the severity of PMS increased there was a significant increase in the negative emotional scoring. However, we had evaluated only two groups mild and moderate category as we didn’t get severe grade category, which is one of the limitations of the study. Another limitation of the study is that the cause of the PMS which is predominantly known to be hormonal fluctuation was not evaluated which otherwise would have increased the power of the study. Further the visual and auditory reaction time increased as the severity of PMS increased thereby proving a poor cognition and psychomotor performance. Thus, negative emotions predominantly depression, anxiety and stress which is prevalent in the PMS affects the cognition and psychomotor skill. This suggest that woman suffering from premenstrual syndrome should take appropriate steps to improve their lifestyle through diet, exercise, yoga and in severe cases medical assistance, so as maintain their executive function.
Acknowledgement
I am thankful to the first-year nursing students of SRM University, Potheri for their voluntary participation in the study. I am thankful to my colleague residents for helping me in my work.
Conflict of Interest
The authors report no conflicts of interest in this work.
References
- Flug D, Largo RH, Prader A. Menstrual patterns in adolescent swiss girls: A longitudinal study. Ann Hum Biol. 1984;11:495–508. [PubMed]
CrossRef - De Ronchi D, Ujkaj M, Boaron F, Muro A, Piselli M, Quartesan R. Symptoms of depression in late luteal phase dysphoric disorder: a variant of mood disorder? J. Affect. Disord 2005;86:169–174. [PubMed:15935236]
CrossRef - Thomas l, Narayanan G. Psycho-Social correlates of perimenstrual distress. The Indian Acade Appl Psychol. 2006;32:80–71.
- Lu Z. The relationship between menstrual attitudes and menstrual symptoms among Taiwanese women. J Adv Nurs. 2001;33:1–8. [PubMed]
CrossRef - Carr-Nangle R, Johnson W, Bergeron K, Nangle D. Body image changes over the menstrual cycle in normal women. Int J Eat Disord. 1994;16:267–73. [PubMed]
CrossRef - Wong LP. Premenstrual syndrome and dysmenorrhea: Urban-Rural and multiethnic differences in perception, impacts, and treatment seeking. J Pediatr Adolesc Gynecol. 2011;24:272–7. [PubMed]
CrossRef - Diener D, Greenstein FL, Turnbough PD. Cyclical variation in digit-span and visual-search performance in women differing in the severity of their premenstrual symptoms. Percept. Mot. Skills 1992;74:67–76. [PubMed: 1561042]
CrossRef - Rapkin AJ, Chang LC, Reading AE. Mood and cognitive style in premenstrual syndrome. Obstet. Gynecol 1989;74:644–649. [PubMed: 2797641]
- 10.Man MS, MacMillan I, Scott J, Young AH. Mood, neuropsychological function and cognitions in premenstrual dysphoric disorder. Psychol. Med 1999;29:727–733. [PubMed: 10405094]
CrossRef - Posthuma BW, Bass MH, Shelley BB, Nisker JA. Detecting changes in functional ability in women with premenstrual syndrome. Am. J. Obstet. Gynecol 1987;156:275–278. [PubMed: 3826160]
CrossRef - Mohan M, Thombre DP, Das AK, Subramanian N, Chandrasekar S. Reaction time in clinical diabetes mellitus. Indian J Physiol Pharmacol. 1984;28(4):311-4.
- Kordi M, Mohamadirizi S, Shakeri M-T, Salehi Fadardi JA, Hafizi L. The relationship between midwives’ work stress and perimenstrual distress. Iran J Obstet Gynecol Infertility. 2011;14:54–63.
- Mohamadirizi S, Kordi M, Shakeri MT. The Relationship between perimenstrual symptoms and menstrual attitude in high-school females in Mashhad city in the years 2011-2012. Iran J Obstet Gynecol Infertility. 2012;15:25–31.
- Mollahadi M, Tayyebi A, Ebadi A, Daneshmandi M. Comparison between anxiety, depression and stress in Hemodialysis and kidney transplantation patients. Iran J Crit Care Nurs. 2010;2:153–6.
- Zahra Aajami, 1 Leila kazazi, 2 Mahdi Toroski, 1 Malihe Bahrami, 3 and Vahidreza Borhaninejad 4 ,Relationship between Depression and Cognitive Impairment among Elderly: A Cross-sectional Study. J Caring Sci. 2020 Aug; 9(3): 148–153.
CrossRef - Halbreich U (1999) Premenstrual syndromes: closing the 20th century chapters. Curr Opin Obstet Gynecol 11:265–270.
CrossRef - Itsekson A, Lazarov A, Cordoba M et al (2004) Premenstrual syndrome and associated skin diseases related to hypersensitivity to female sex hormones. J Reprod Med 49:195–199.
- Vilko N (2001) Mood changes, caused by hormonal Xuctuations, helped by therapy. Available at: http://www.pacpubserver.com/ new/health/f-h/hm012801.html. Accessed 19 Jul 2007.
- Van Wingen GA, Ossewaarde L, Backstrom T, Hermans EJ, Fernandez G. Gonadal hormone regulation of the emotion circuitry in humans. Neuroscience. 2011; 191:38–45.
CrossRef - Benedek T, Rubenstein BB. The correlations between ovarian activity and psychodynamic processes. Psychosom Med. 1939 1:245–270.
CrossRef - Jana Hoyer , Inga Burmann, Marie-Luise Kieseler , Florian Vollrath , Lydia Hellrung , Katrin Arelin, Elisabeth Roggenhofer, Arno Villringer, Julia Sacher.Menstrual Cycle Phase Modulates Emotional Conflict Processing in Women with and without Premenstrual Syndrome (PMS) – A Pilot Study. April 2013 | Volume 8 | Issue 4 | e59780
CrossRef - Golub S (1985) (ed) Lifting the curse of menstruation. Harrington Park, New York
- Woods NF, Most A, Dery GK (1982) Prevalence of perimenstrual symptoms. Am J Public Health 72:1257–1264
CrossRef - NHS Direct (2007) Premenstrual syndrome. Available at: http://www.nhsdirect.nhs.uk/articles/article.aspx?articleId = 295. Accessed July 19, 2007.
- Olson KC, Carroll HA, Lustyk MK. Psychophysiological stress reactivity relationships across the menstrual cycle. J Horm. 2015; 2015:1–5.
CrossRef - Kischabaum C, Kudielka BM, Gaab J, Schommer NC, Hellhammer DH. Impact of gender, menstrual cycle phase, and oral contraceptives on the activity of the hypothalamus-pituitary-adrenal axis. Psychosom Med. 1999; 61(2):154–162.
CrossRef - Baca-García E, Sanchez-González A, González Diaz-Corralero P et al (1998) Menstrual cycle and proWles of suicidal behaviour. Acta Psychiatr Scand 97:32–35.
CrossRef - Baca-García E, Diaz-Sastre C, de Leon J et al (2000) The relationship between menstrual cycle phases and suicide attempts. Psychosom Med 62:50–60.
CrossRef - Saunders KEA, Hawton K (2006) Suicidal behaviour and the menstrual cycle. Psychol Med 36:901–912.
CrossRef - Sigmon ST, Dorhofer DM, Rohan KJ et al (2000) Psychophysiological, somatic, and affective changes across the menstrual cycle in women with panic disorder. J Consult Clin Psychol 68:425–431.
CrossRef - Yonkers KA, O’Brien PMS, Eriksson E. Premenstrual syndrome. Lancet. 2008;371(9619):1200–1210.
CrossRef - Olson KC, Carroll HA, Lustyk MK. Psychophysiological stress reactivity relationships across the menstrual cycle. J Horm. 2015;2015:1–5.
CrossRef - Sherwin BB (2003) Estrogen and cognitive functioning in women. Endocr Rev 24:133–151.
CrossRef - Genazzani AR, Pluchino N, Luisi S et al (2007) Estrogen, cognition and female ageing. Hum Reprod Update 13:175–187
CrossRef - McEwen B (2002) Estrogen actions throughout the brain. Recent Prog Horm Res 57:357–384.
CrossRef - Genazzani AR, Pluchino N, Luisi S (2007) Estrogen, cognition and female ageing. Hum Reprod Update 13:175–187.
CrossRef - Maki PM, Rich JB, Rosenbaum RS (2002) Implicit memory varies across the menstrual cycle: estrogen effects in young women. Neuropsychologia 40:518–529.
CrossRef - Lord T, Taylor K (1991) Monthly Xuctuation in task concentration in female college students. Percept Mot Skills 72:435–439.
CrossRef - Ussher JM, Wilding JM (1991) Performance and state changes during the menstrual cycle, conceptualised within a broad band testing framework. Soc Sci Med 32:525–534.
CrossRef
Abbreviations
PMS – Premenstrual syndrome
MDQ- Menstrual Distress Questionnaire
DASS – Depression, Anxiety, and Stress Scale Questionnaire
RT – Reaction time
WHO – World Health Organization
VRT- Visual reaction time
ART – Auditory reaction time







