D.Manoharan , Shreya Srinivasan
, Shreya Srinivasan , Vignesh NR*
, Vignesh NR* and Aswin Senthilvel
and Aswin Senthilvel
Department of Dermatology, Venereology and Leprosy, Sree Balaji Medical College and Hospital, Chennai, India
Corresponding Author E-mail:drvigneshnr@gmail.com
DOI : https://dx.doi.org/10.13005/bpj/2722
Abstract
The most frequently prescribed antibiotic class in dermatology is the tetracycline family, which has both antibacterial and anti-inflammatory characteristics. Tetracycline is a broad-spectrum polyketide antibiotic effective against gram-positive and gram-negative organisms. It has been accepted for the therapeutic use of various conditions in dermatology like Acne, Rosacea, Syphilis, Immuno-bullous dermatoses, Pyoderma gangrenosum and Hidradenitis Suppurativa to name a few. However, the use and efficacy of newly discovered tetracyclines like Sarecycline, Omadacycline and Tigecycline are still yet to be documented and researched. In this study, a short summary of the utilization of various tetracycline are being documented for their use in dermatology.
Keywords
Anti-Inflammatory; Doxycycline, Minocycline, Tetracycline
Download this article as:| Copy the following to cite this article: Manoharan D, Srinivasan S, Vignesh N R, Senthilvel A. Tetracyclines: The Old, the New and the Improved - A Short Review. Biomed Pharmacol J 2023;16(3). |
| Copy the following to cite this URL: Manoharan D, Srinivasan S, Vignesh N R, Senthilvel A. Tetracyclines: The Old, the New and the Improved - A Short Review. Biomed Pharmacol J 2023;16(3). Available from: https://bit.ly/3sI5feS |
Introduction
Chlortetracycline, originally known as aureomycin, was the first tetracycline discovered and was derived from the bacterium Streptomyces aureofaciens. By reversibly attaching to the bacterial 30S ribosomal subunit and preventing incoming aminoacyl tRNA from binding to the ribosome acceptor site, it has a bacteriostatic impact on bacteria. In the past 55 years, a wealth of information has been available, revealing both the advantageous and detrimental effects of tetracyclines, changing some indications, and offering new recommendations for dermatologists to take into account.1
Methods
Tetracyclines, their varied modes of action, uses, side effects, drug interactions, and contraindications were all well-researched in the literature. The search engines used for the literature searches were PubMed and Google Scholar. Tetracyclines, uses of tetracyclines in dermatology, recent advances in tetracyclines, Sarecycline, Omadacycline, Lymecycline, Minocycline, drug interactions of tetracyclines, contraindications of tetracyclines and side effects of tetracyclines were some of the keywords used to search for related articles. The analysis covers articles that were published since 2012. These studies’ results were combined to create a narrative review.
Chemical Composition
Tetracyclines (Tc) are built up of four-fused, six-membered rings that compose the fundamental structure originally generated from Streptomyces spp., but modern derivatives are semisynthetic.2
 |
Figure 1: Chemical composition of Tetracyclines3 |
Classifications of Tetracyclines
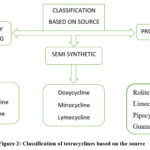 |
Figure 2: Classification of tetracyclines based on the source |
 |
Figure 3: Classification of tetracyclines based on the generation |
Pharmacokinetics and Pharmacodynamics
The oral absorption of most tetracyclines is insufficient. When taken intramuscularly, bioavailability is less than 40%, 100% intravenously, and 60-80% orally (fasting adults). Gastrointestinal absorption of oral formulations of tetracycline is reduced by 50% when taken with food/milk.4
As the dose is increased, the amount of medicine that is not absorbed increases. Absorption is hampered by the concurrent consumption of divalent and trivalent cations, such as Fe2+/3+, Al3+, Zn2+, Mg2+ and Ca2+. As a result, the absorption of tetracyclines can be hampered by dairy products, antacids, aluminum hydroxide gels, zinc or iron salts, magnesium, bismuth subsalicylate, calcium, and dietary zinc and iron supplements. The peak plasma concentration is obtained in 2-4 hours following a single oral dosage. The half-life varies between 6 and 12 hours, and are often taken two to four times each day. The presence of tetracycline in body fluids, including Cerebrospinal fluid (CSF), is widespread. All tetracyclines have a propensity to accumulate in the spleen, liver, tumors, bone, and teeth. Tetracyclines cross the placenta and get into the amniotic fluid and fetal circulation. Breast milk contains quite high amounts. With the exception of doxycycline, the kidney is the main organ via which most tetracyclines are removed, however, they are also concentrated in the liver, expelled in bile, and partially reabsorbed through enterohepatic recirculation. On the other hand, doxycycline is generally excreted via the bile and urine.
Mechanism of Action
Tetracyclines act through various mechanisms such as:
Antibacterial Effect
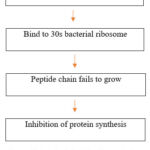 |
Figure 4: Flowchart depicting the mechanism of anti-bacterial action of tetracyclines |
Tetracyclines bind to the 30S bacterial ribosome and block aminoacyl tRNA from reaching the acceptor (A) site on the mRNA-ribosome complex, which inhibits the production of bacterial proteins. Both passive diffusion through channels created by porins in the outer cell membrane and active transport, which pumps tetracyclines across the cytoplasmic membrane, allow these medications to penetrate gram-negative bacteria.5
 |
Figure 5: Illustrated image depicting the mechanism of anti-bacterial action of tetracyclines 6 |
Anti-Inflammatory Effect
By preventing bacterial breakdown products, which trigger inflammatory processes, doses below the minimal inhibitory concentration indirectly affect inflammation. They suppress production of pro-inflammatory cytokines like tumor necrosis factor, interleukin-1, and IL-8. Leukocyte migration, which takes place in the initial phases of inflammation, is inhibited by them. By binding intracellular calcium, which is required for the development of microtubules that allow for cell movement, it prevents cell mobility. Tetracyclines suppress the activity of inducible nitric oxide synthase (iNOS), which lowers nitric oxide (NO). The highly cytotoxic peroxynitrite radical that iNOS ultimately produces is what inhibits collagen and proteoglycan synthesis and boosts matrix metalloproteinases (MMP) expression. Tetracyclines reduce peroxynitrite radicals, which prevent protein denaturation.
Inhibition of Matrix Metalloproteinases
The family of zinc-dependent proteases known as matrix metalloproteinases (MMPs) produced by connective tissue cells and inflammatory cells are involved in a wide range of physiological and pathological processes. In nearly all inflammatory human diseases, metalloproteinases are shown to be more active than normal. Tetracyclines block action of metalloproteinases by inhibiting them from binding to zinc or calcium ion.
Tetracyclines also block alpha-amylases, a member of the hydrolase group, and phospholipases in addition to metalloproteinases. A crucial enzyme in the manufacture of inflammatory mediators such as prostaglandins is phospholipase A2.
Antioxidant Effect
Tetracyclines also neutralize reactive oxygen species (ROS) and protect cell structures from oxidative damage. The retention of ROS by these compounds depends on the phenolic ring. A stable phenolic radical that is enclosed by the side groups of the phenolic ring and does not interact further is created when a free radical attaches to the phenolic ring.
Spectrum
 |
Figure 6: Spectrum of action of tetracyclines |
Recent Advances in Tetracycline
Tigecycline
Tigecycline, a glycylcycline group of antibiotics structurally related to minocycline, has a decreased susceptibility to resistance compared to other drugs in the tetracycline group and due to its limited oral absorption, it can only be used by intravenous route. It cannot be used to treat urinary tract infections, bacteremia, or meningitis because of its weak concentration in blood and urine. Tigecycline is effective against gram-positive and gram-negative organisms as well as anaerobes, in contrast to other tetracyclines. A pooled evaluation of tigecycline clinical trials found a modestly greater but statistically significant risk of death compared to active comparator antibiotics. Therefore, tigecycline should normally only be used for infections that are resistant.
Sarecycline
Sarecycline is a brand-new, once-daily, tetracycline-derived oral antibiotic that has received FDA approval in the US for the treatment of moderate-to-severe acne vulgaris in patients aged 9 years and above. It can be taken with or without meals. Sarecycline exhibits modest effect against enteric aerobic Gram-negative bacteria but has anti-inflammatory characteristics and powerful activity against Gram-positive bacteria, including activity against several strains of Cutibacterium acnes. Sarecycline was examined for chest and back acne, unlike many other research on acne. At 1.5 mg/kg/day of sarecycline, a substantial decrease in inflammatory lesions was observed at week 12, with statistically significant improvement visible as early as week 3. There were no complaints of phototoxicity, vertigo, pseudotumor cerebri, or lupus, but nausea and vaginal candidiasis of 1.2% and 1.2%, respectively, were reported.7
Omadacycline
Omadacycline (Nuzyra – Paratek), a semi-synthetic tetracycline derivative, has been approved by the FDA for the once-daily intravenous and oral treatment of acute bacterial skin and skin structure infections (ABSSSIs) and community-acquired bacterial pneumonia (CAP) in adults. Gram-positive, gram-negative, atypical, and anaerobic pathogens are all susceptible to omadacycline’s broad spectrum of activity.8
Lymecycline
Tetracyclines and L-lysine were combined to create the semi-synthetic tetracycline known as lymecycline. It differs from tetracycline in that it has higher serum levels, improved tissue penetration, and slower clearance rates.
Lymecycline is taken as a straightforward, once-daily regimen because it has the maximum oral absorption of all tetracyclines. It produces fewer side effects than earlier medications from this class.
A multicenter, randomized, blinded trial comparing the effectiveness, safety, and cost-efficiency of using lymecycline and minocycline found that both medications had a similar safety and efficacy profile, but that lymecycline had a 4-fold lower cost of treatment.9
Minocycline-Extended Release
After studies revealed that minocycline had a longer half-life (15–25 hours), lower risk for resistance, less GI side effects, and less influence on its action from dairy consumption, it became more widely used to treat acne. However, using minocycline has been linked to a higher incidence of side effects, such as drowsiness and lupus brought on by medication. The standard dosage for treating acne vulgaris using instant release minocycline hydrochloride 100mg twice daily, has been linked to these side effects. By allowing for a slower rise in serum levels and a lower maximum concentration, extended-release minocycline has the potential to lessen the risk of systemic side effects linked to greater serum levels of the drug.10
Resistance
Tetracycline resistance in cells is caused in three ways.
Tetracycline is actively pumped out of cells by a membrane protein that is encoded by the Efflux resistance gene.
Ribosomal defenses that prevent tetracycline from attaching to the ribosome.
The least common type of resistance is enzymatic, in which the medicine is rendered inactive by the addition of an acetyl group to the drug’s molecule.11
Topical Uses of Tetracyclines
Due to their chronic nature, potential for deformity, and psychological effects, rosacea and acne vulgaris pose therapeutic obstacles. Both disorders have significant inflammatory components despite having different pathophysiologic causes. Systemic antibiotics are therefore frequently recommended for months at a time as opposed to the days or weeks that are normal for infections. In response to the emergence of resistant bacterial strains, adverse events and compliance issues related to chronic systemic broad-spectrum antibiotic use, new treatment strategies have been developed, including the use of sub-antimicrobial doses, narrow-spectrum oral antibiotics and new formulations of topical minocycline. 4% of topical minocycline is used to treat acne vulgaris while 1.5% is used to treat rosacea.12
Indications in Dermatology
Table 1: Indications in Dermatology
|
Indications in Dermatology |
|
|
Based on Antibacterial effect |
Based on anti-inflammatory effect |
|
· Acne · Syphilis · Lyme borreliosis · Lymphogranuloma venereum · Granuloma inguinale · Rickettsia · Atypical Mycobacterial infections · Chlamydial non-specific urethritis/Endo cervicitis · Atypical Pneumonia · Cholera · Plague · Relapsing fever · Recurrent aphthous stomatitis · Acrodermatitis chronica atrophicans |
· Acne · Rosacea · Autoimmune bullous disorder · Neutrophilic disorders (Pyoderma gangrenosum, sweet’s syndrome) · Kaposi sarcoma · Granulomatous diseases (Sarcoidosis, Necrobiosis lipoidica) · Palmoplantar pustular psoriasis · Hidradenitis suppurativa · Oral lichen planus · Prurigo pigmentosa · Acne keloidalis nuchae |
Usage in Infectious Conditions
Syphilis
Doxycycline 100 mg BID orally for 2 weeks
Or Tetracycline 500mg QID orally for 2 weeks
It can be used as an alternate treatment for patients with primary, secondary, and early latent syphilis who are allergic to penicillin.
Doxycycline 100mg orally bid for 30 days
Or Tetracycline 500mg orally QID for 30 days
It can be given as alternative regimen for penicillin allergic patients in
late Latent syphilis
Leprosy
The only antibiotic in the tetracycline family to demonstrate notable activity against M. Leprae is minocycline, which could be attributed to cell wall penetration due to its lipophilic nature. Although the precise way that minocycline works to stop M. Leprae has not been confirmed, it is thought to be similar to other members of the tetracycline family that work by preventing protein synthesis. Minocycline has bactericidal action against M. Leprae, with a dose-dependent MIC (minimum inhibitory concentration) of 0.2 g/ml. Minocycline has proven to have an additive impact when used with rifampin, dapsone, and clarithromycin. Minocycline has also shown promising action when combined with another fluoroquinolones such as moxifloxacin and ofloxacin with combinations such as rifapentine + moxifloxacin + minocycline (PMM), or particularly rifampin + ofloxacin + minocycline (ROM). 13
Lyme Disease
Early Lyme illness can be effectively treated with Doxycycline 100 mg BD for 14 days, but relapsing, persistent Lyme disease does not seem to be curable with this medication.
Atypical Mycobacterial Infections
To stop the inducible resistance seen in several Mycobacteria spp., combination therapy is advised. Mycobacterium marinum infections have been successfully treated with immediate release formulations of minocycline (100-200 mg daily for 6–12 weeks) and doxycycline (100 mg twice day for 12–16 weeks).
Chlamydia Trachomatis
C. trachomatis, which infects 100 million individuals worldwide each year, is the most common STI bacterial agent. Doxycycline 100 mg twice daily for 7 days was effective in treating this infection.
Usage in Inflammatory Conditions
Acne Vulgaris
The most often prescribed oral antibiotics for the management of acne vulgaris have historically been tetracyclines.
Doxycycline is given at a dose of 50-100mg daily. It has been reported that a sub antimicrobial dose(40mg/kg) of doxycycline given for 6 months significantly reduces both non-inflammatory and inflammatory acne without any side effects. The primary mechanism of action of sub antimicrobial dose is anti-inflammatory mechanism.
Tetracycline is given at the dose of 1g/day on an empty stomach. The initial dose is followed by 250-500mg for several months
Minocycline has an advantage because of its high concentration in the pilosebaceous unit. Recommended dose is from 50-100mg twice daily.
Rosacea
Table 2: Tetracyclines in Rosacea
|
DRUGS |
EFFECTS ON BIOLOGICAL TARGETS OR ACTIVITIES |
CORRELATION WITH ROSACEA PATHOPHYSIOLOGY |
|
Tetracycline, Minocycline |
Inhibit neutrophil migration and chemotaxis |
Inflammation and oxidative stress |
|
Minocycline, Doxycycline |
Inhibit expression of respirator oxygen or oxidative burst from neutrophils |
Inflammation, Dermal destruction |
|
Chemically Modified Tetracycline, Minocycline, Doxycycline |
Inhibit expression, production or activity of matrix metalloproteinases |
Abnormal vasculature, Dermal destruction |
Erythema Nodosum
Tetracycline suppresses fat necrosis and lipolysis. Reactive oxygen species have been suggested to be involved in the pathogenesis of EN. Tetracyclines have the ability to remove reactive oxygen species from the environment. This could be one of the reasons why patient’s condition improved after taking tetracycline.
Bullous Pemphigoid
By inhibiting neutrophil chemotaxis and inflammatory mediators in this bullous illness, tetracyclines in combination with niacinamide decrease the inflammatory response mediated by complement at the basement membrane zone.
Pyoderma Gangrenosum
Tetracycline treats pyoderma gangrenosum using both anti-inflammatory and anti-chemotactic drugs rather than merely antibacterial ones. The typical dose is 100 mg daily, however in many cases larger doses of 300 mg four times daily have been needed.
Hidradenitis Suppurativa
Tetracyclines taken orally are utilized as first-line oral therapy by 75% of dermatologists in the UK, according to a recent survey.
Confluent Reticulate Papillomatosis (Crp)
Some studies on CRP conducted in recent years have concentrated on the pathogenesis of bacteria in causing the disease. This notion is supported by the positive response to antibiotics like azithromycin and minocycline in clinical settings. Additionally, tetracycline groups inhibit metalloproteinase, hydrolase, phospholipase A2, tumor necrosis factor alpha, interleukin (IL)-1, and IL-6 as well as reduce IL-8 and neutrophil oxidative burst and hence have both antibacterial and anti-inflammatory effects.14
CMT-3 (Chemically Modified Tetracycline) in Kaposi Sarcoma
The CMTs are successful in treating metastasis, which is responsible for more than 90% of cancer-related mortality, according to recent reports. An imbalance between the damaging enzymes and their inhibitors results from tumor cells producing too much serine proteinase and matrix-degrading MMPs. By causing cell cycle arrest and apoptosis, they suppress cell proliferation in addition to the invasive potential and MMP activity. By producing hydroxyl free radicals that penetrate and depolarize mitochondria, CMTs destroy tumor cells. Additionally, they accelerate caspase-mediated apoptosis and slow down angiogenesis. 15
Recurrent Aphthous Stomatitis
The, size, pain and duration of the ulcers are significantly reduced with treatment of tetracycline. Doxycycline 100 mg in 10 ml water used as a mouthwash for 2-4 minutes, 4 times daily for 3 days, has shown promising effects in treating ulcers in the UK, according to a clinical investigation. 16
Oral Lichen Planus
In the literature, there is a report of significant improvement in patients following one week of rinsing with a tetracycline solution (0,25%) for 2-4 minutes, three times per day. 17
Acne Keloidalis Nuchae
Tetracycline derivatives with antibacterial and anti-inflammatory properties, including doxycycline, minocycline, and tetracycline, are frequently used oral antibiotics. These medications are effective at reducing infection-related symptoms like inflammation. Although the fibrotic lesions may still be present, the vertex lesions tend to react more quickly and experience less pain and bleeding.
Contraindications
After prolonged usage of tetracyclines during pregnancy, there may be a risk of Tc-associated fatty liver. Due to Tc’s propensity to deposit in calcified tissues, which can lead to bone distortion and growth retardation, it is not recommended that Tc be administered to children aged less than 8 years. Using minocycline while lactating results in the development of black galactorrhea.
Tetracyclines in Pregnancy and Lactation
Tetracyclines are prohibited during pregnancy because they are on the list of known human teratogens. It is a medication which belongs to pregnancy category D. The fetus is known to be at established teratogenic risk when exposed to tetracyclines and their derivatives, such as oxytetracycline. They are linked to greater risks of cleft palate, neural tube anomalies, and other serious congenital abnormalities (MCAs). Tetracyclines are excreted in breast milk in significant amounts, but are found in extremely low levels in breastfed newborns, which is a result of calcium-mediated chelation. However, unless the advantages clearly outweigh the hazards, tetracyclines should be avoided during lactation. 18
Tetracyclines in Paediatrics
Because tetracyclines can cause yellowish staining of the teeth and also adversely affect the development of bone, they are contraindicated in children under 9 years of age.
Tetracyclines in Morphea
There are two school of thoughts regarding the role of tetracyclines in morphea. Tetracyclines are used in the treatment of morphea due to its antibacterial effect against Borrelia which is one of the causes of morphea whereas recent research has also shown that tetracyclines, such as minocycline, may reduce angiogenesis, rendering this and MMP inhibition as additional intriguing potential pathways by which minocycline may cause or aggravate morphea. 19
Side Effects
Table 3: Side Effects of Tetracyclines
|
1. |
PHOTOSENSITIVITY |
When Tetracycline is exposed to sunlight for a lengthy period of time, a photosensitive reaction occurs. Doxycycline has dose-related phototoxicity, but minocycline has low photosensitivity. |
|
2. |
SKIN PIGMENTATION
|
Minocycline is an antibiotic that is often used to treat acne. Only a small percentage of persons who use it for a long time develop dark pigmentation. Taking larger dosages of minocycline increases your chances of developing hyperpigmentation. If you are exposed to the sun, your chances of developing darker pigmentation increase as well. Tetracycline-induced skin pigmentation normally diminishes once you stop taking the medicine.
There are four types of skin pigmentation caused by tetracyclines: Type I refers to blue-black or grey pigmentation that is restricted to acne-related scarring or inflammation on the face (which often heals slowly) and stains for iron.
Type II refers to blue-grey pigmentation of normal skin on the lower thighs and the forearms, which normally fades slowly and stains for both iron and melanin.
Type III refers to normal skin that is discoloured and muddy brown in colour, mainly in sun-exposed skin (tends to last); stains only with melanin.
Type IV is a seldom seen type that manifests as restricted blue-grey pigmentation in acne scars on the back (the long-term course is unknown). This pigment is calcium-containing but iron-free.
|
|
3. |
SYSTEMIC LUPUS ERYTHEMATOSUS (SLE) |
Tc have been suggested as potential agents linked to drug-induced SLE, however there is no evidence to support this. They probably cause photosensitivity or a latent SLE flare-up. However, recent findings suggest that minocycline may be a medication that both clinically and serologically precipitates SLE. |
|
4. |
PSORIASIS |
Tc may cause the beginning of psoriasis or worsen an already present condition. Exacerbation is indicated by the development of new plaques, a propensity for rapid confluence, and itching. |
|
5. |
GASTROINTESTINAL |
Diarrhea, Nausea, vomiting and unexplained digestive difficulties are some common gastrointestinal side effects |
|
6. |
NEUROLOGICAL |
Tinnitus, labyrinthine dysfunction, ataxia, vertigo, vestibular disturbance, including lightheadedness, dizziness, and unsteadiness, can all be brought on by minocycline. |
|
7. |
RENAL |
Acute interstitial nephritis, azotemia, and Fanconi syndrome are listed as potential adverse effects. |
|
8. |
BENIGN INTRACRANIAL HYPERTENSION
|
The condition known as benign intracranial hypertension (BIH), sometimes known as pseudotumor cerebri, is an infrequent idiopathic response to TCNs. To enable early detection of BIH, a high index of suspicion when a patient presents with headache, visual abnormalities, and nausea and/or vomiting is essential. Persistence of this illness can result in significant vision loss that may be irreversible. If BIH is suspected, it is advised to stop using the suspected agent and to seek early ophthalmologic evaluation to check for papilledema. |
|
9. |
SEGAL’S TRIAD |
Characterized by photosensitivity, nail discoloration and onycholysis. |
Monitoring
Periodic laboratory evaluations of organ systems, including hematopoietic, renal, and hepatic investigations, should be carried out in long-term therapy. However, the requirement for baseline testing is not mentioned, and no explicit recommendations are made regarding the nature, timing, or frequency of “periodic laboratory tests”. Importantly, thorough evaluations on the long-term management of rosacea and acne vulgaris do not outline precise laboratory monitoring guidelines.
Toxicity
Liver damage: Jaundice and fatty liver are occasionally seen. In this aspect, oxytetracycline and tetracycline are safer. Tetracyclines provide a risk to unborn babies because they can cause acute hepatic necrosis, which can be deadly. 20
Renal damage: This risk only exists in cases where kidney disease is already present. Except for doxycycline, all tetracyclines build up in the body and worsen renal failure. Outdated tetracyclines can cause a disease similar to Fanconi syndrome that is reversible. Epitetracycline, anhydrotetracycline, and epianhydrotetracycline are the degradation products that harm proximal tubules. Such deterioration is favored by heat, moisture, and acidic pH.
Phototoxicity: Some people get a severe skin reaction on exposed portions that resembles a sunburn. Demeclocycline and doxycycline have been associated with an increased incidence. Sometimes nails may be distorted.
Tetracyclines have a chelating effect on teeth and bones. Calcium-tetracycline chelate is deposited in growing bone and teeth. The deciduous teeth are impacted between mid-pregnancy and five months after birth, resulting in brown discoloration and malformed, more cariogenic teeth. Tetracyclines have an impact on the crown of permanent anterior dentition, when taken between 3 months and 6 years of age. Tetracyclines taken in late pregnancy or during childhood may temporarily decrease bone development. The final impact on stature is largely negligible, but with continued use, abnormalities and height loss are possible.
Anti-Anabolic effect: Tetracyclines have a catabolic impact and decrease protein synthesis. They can raise blood urea and cause a negative nitrogen balance.
Vestibular toxicity: Ataxia, vertigo, and nystagmus are common side effects of minocycline which subside on stopping the drug.
Drug Interactions
Table 4: Drug Interactions of Tetracyclines
|
Drug category |
Drug examples |
Comments |
|
Retinoids |
Isotretinoin > acitretin |
Increases the risk of pseudotumor cerebri |
|
Ionotropic agents |
Digoxin |
May increase the level of digoxin in about 10% of individuals |
|
Xanthine bronchodilators |
Theophylline |
May increase the levels of theophylline and toxicity including CNS adverse effects |
|
Anticoagulants |
Warfarin |
May increase the levels/ anticoagulant effect |
|
Antacids, Food |
Milk |
Decreases the absorption of tetracyclines |
|
Other chelating agents |
Bismuth salts, iron, zinc |
Chelation with these drugs may decrease the absorption of tetracyclines |
Conclusion
Tetracyclines are a steadily expanding class of antibiotics that are widely employed in dermatology. In this article, the antibacterial and anti-inflammatory properties of tetracyclines are discussed in relation to cutaneous illnesses that have been treated with them. Recent advances in this group of drugs have led to newer tetracyclines which have umpteen number of benefits over conventional tetracyclines. To conclude, our article highlights the latest advances in tetracyclines which have enabled their use in various dermatological conditions.
Acknowledgements
None
Conflict of Interest
There is no conflict of interest.
Funding Sources
There are no funding sources
References
- Uma A, Mercy AA, Marx KK. Chemotherapy and Aquatic Therapeutics. CRC Press; 2020 Nov 1.
- Li G, Lou M, Qi X. A brief overview of classical natural product drug synthesis and bioactivity. Org Chem Front. 2022;9:517-71.
CrossRef - Tsankov N, Broshtilova V, Kazandjieva J. Tetracyclines in dermatology. Clin Dermatol. 2003;21:33-9.
- Noreddin A. Readings in advanced pharmacokinetics-theory, methods and applications. InTech; 2012.
- Anandabaskar N. Protein synthesis inhibitors. Introduction to Basics of Pharmacology and Toxicology: Volume 2: Essentials of Systemic Pharmacology: From Principles to Practice. 2021:835-68.
- Graber EM. Treating acne with the tetracycline class of antibiotics: A review. Dermatol Rev. 2021;2:321-30.
- Moore AY, Charles JE, Moore S. Sarecycline: a narrow spectrum tetracycline for the treatment of moderate-to-severe acne vulgaris. Future Microbiol. 2019;14:1235-42.
CrossRef - Omadacycline (Nuzyra) – A New Tetracycline Antibiotic. JAMA. 2019;322:457-458.
CrossRef - Orylska-Ratynska M, Placek W, Owczarczyk-Saczonek A. Tetracyclines—An Important Therapeutic Tool for Dermatologists. Int J Environ Res Public Health. 2022;19:7246.
CrossRef - Krout CO, Lio PA. Tetracyclines: history and current formulation review from a dermatology perspective. Pract Dermatol. 2015;2:51-4.
- Varela MF, Stephen J, Lekshmi M, Ojha M, Wenzel N, Sanford LM, et al. Bacterial Resistance to Antimicrobial Agents. Antibiotics (Basel). 2021;10:593.
CrossRef - Martins AM, Marto JM, Johnson JL, Graber EM. A review of systemic minocycline side effects and topical minocycline as a safer alternative for treating acne and rosacea. Antibiotics (Basel). 2021;10:757.
CrossRef - Cambau E, Williams DL. Anti-leprosy drugs: modes of action and mechanisms of resistance in Mycobacterium leprae. International textbook on leprosy 2019.
- Ataş H, Keseroğlu HÖ, Gönül M, Khurami FA. Successful treatment of confluent and reticulated papillomatosis with tetracycline and mupirocin. Turkderm-Turk Arch Dermatol Venereol. 2018;52:64-66
- Suchetha A, Suprabhan S, Sapna, et al. Chemically Modified Tetracyclines: A Review. World J Pharm Res. 2020;9:485-95.
- Noor S, Menzel A, Gasmi A. Oral Aphthous: Pathophysiology, Clinical Aspects and Medical Treatment. Arch Razi Inst. 2021;76:1155.
- Bagan J, Compilato D, Paderni C, Campisi G, Panzarella V, Picciotti M, et al. Topical therapies for oral lichen planus management and their efficacy: a narrative review. Curr Pharm Des. 2012;18:5470-80.
- Cross R, Ling C, Day NP, McGready R, Paris DH. Revisiting doxycycline in pregnancy and early childhood–time to rebuild its reputation? Expert Opin Drug Saf. 2016;15:367-82.
CrossRef - Pettit C, Mosser-Goldfarb J. A Case of Minocycline-induced Linear Morphea Reactivation. J Clin Aesthet Dermatol. 2021;14:44.
- Kleiner, D. Drugs and Toxins. Macsween’s Pathology of the Liver (Seventh Edition); Burt, A.; Ferrell, L.; Hübscher, S.; Elsevier, 2018;673-779.








