Rashmi Hullalli * , M R Gudadinni
, M R Gudadinni  and Rohith M
and Rohith M
Department of Community Medicine, Shri B M Patil Medical College, Vijayapura Karnataka, India.
Corresponding Author E-mail:drrohith88@gmail.com
DOI : https://dx.doi.org/10.13005/bpj/2755
Abstract
Background and Objectives: Tuberculosis (TB) and Diabetes Mellitus (DM) co-morbidity are of rising public health problems. There is growing evidence that DM is an important risk factor for TB. This study was carried out to know the prevalence of DM among newly detected sputum-positive pulmonary TB patients registered in the District Tuberculosis Centre and also to assess the risk factors of DM among TB patients. Methods: In a cross-sectional study newly detected sputum-positive pulmonary TB patients were screened for DM (those having symptoms of DM). Further, they were diagnosed by doing random blood glucose levels (≥200 mg/dl.). Mean, standard deviation (SD), Chi-square and Freeman-Halton Fisher exact test were used to know the significant association. p value less than 0.05 was considered statistically significant. Results: A total of 215 TB patients were included in the study. The prevalence of DM among TB patients was found to be 23.7% (2.8% known and 97.8% new cases). Significant associations were found between age (>46 years), educational status, smoking habits, alcohol consumption, physical activity, presence of symptoms of DM and family H/o DM. Interpretation and Conclusion:Routine screening for DM is mandatory because of the increasing prevalence which may help in early diagnosis and also reduce the complication by proper management which in turn helps in the successful outcome of TB treatment.
Keywords
Diabetes mellitus; Prevalence; Poor outcome; Risk factors; Tuberculosis
Download this article as:| Copy the following to cite this article: Hullalli R, Gudadinni M. R, Rohith M. Prevalence of Diabetes Mellitus Among Newly Detected Sputum Positive Pulmonary Tuberculosis Patients and Associated Risk Factors. Biomed Pharmacol J 2023;16(3). |
| Copy the following to cite this URL: Hullalli R, Gudadinni M. R, Rohith M. Prevalence of Diabetes Mellitus Among Newly Detected Sputum Positive Pulmonary Tuberculosis Patients and Associated Risk Factors. Biomed Pharmacol J 2023;16(3). Available from: https://bit.ly/3PWBwbr |
Introduction
With urbanization as well as social and economic development, there has been a rapidly growing prevalence of DM. People with a weak immune system such as diabetes, are at a higher risk of progressing from latent to active disease. So people with DM have a 2-3 times higher risk of getting TB when compared to people without DM.2 About 10% of TB cases in the world are linked to DM.1 A large proportion of people living with DM as well as TB are not diagnosed or diagnosed too late. Therefore, early detection can help improve the care and effective control of both diseases.
DM can increase the time taken to sputum culture conversion and thus it leads to the development of drug resistance if a 4 drug regimen in the intensive phase is changed to 2 drug regimen after 2 months in the presence of culture-positive time1 People living with DMTB have a higher risk of death during treatment and risk of TB relapse after completing treatment. DM is complicated by the presence of infectious diseases, including TB. It has also been observed that good glycaemic control in TB patients can improve treatment outcomes. Recent studies have shown that DM accounts for 20% of smear-positive TB and have indicated that an increase in DM prevalence in India has been an important obstacle to reducing TB prevalence2
There is a lack of literature regarding this comorbidity in our area. Therefore, this study was conducted to know the prevalence of DM among TB patients in Vijayapura taluk. And to study the socio-demographic profile of tuberculosis patients with diabetes mellitus and also to identify the risk factors.
Material and methods
Ethical clearance was obtained from the Institutional Ethical Committee of Shri B M Patil Medical College, BLDE University (Certificate No – 65/21-10-17). The present study was a cross-sectional study done at Vijayapura TU. It covers 14 primary health centres, 4 urban health centres and 2 medical colleges. A tuberculosis register was used to approach the TB patients. More than 18 years of age sputum positive TB cases of Vijayapura taluk registered from January 1st to December 31st 2016 were included. Patients who are critically ill, not willing to participate, and pregnant and lactating women were not included in the study. Considering the prevalence of diabetes mellitus among tuberculosis patients to be 30.6%3, at a 95% confidence level and at 20% allowable error, the sample size is calculated by using the formula
Apparently, non-diabetic patients were screened for DM by examining blood glucose levels in capillary blood using a finger-prick glucometer. Those found positive and having symptoms of DM were further evaluated by doing random blood glucose levels. Health workers/ASHAs were involved in the study. Objectives were explained to them. The TB patients were approached at their homes/DOTS centres/PHCs with the help of the Senior Treatment Supervisor. The Procedure included 3 parts i.e., an interview through semi structured questionnaire, anthropometric measurements and blood glucose estimation. Classification of DM was done using American Diabetic Association. The detected DM patient’s house was revisited and health education was given. The data was compiled in a Microsoft Excelworksheet sheet and analysed using Statistical Package for Social Sciences (SPSS) version 16.0 software. The data was presented in the form of tables and graphs wherever necessary. All characteristics were summarized descriptively. For continuous variables, the summary statistics of n, mean, and standard deviation about the arithmetic mean (SD) were used. For categorical data, the number and percentage were used in the data summarized. Chi-square test will be used to know the significant association. P-value less than 0.05 will be considered statistically significant.
Table 1: Distribution of sociodemographic characteristics of study participants (n=215)
|
Study variable |
Number (n) |
Percentage (%) |
|
Age (yrs.) |
|
|
|
15-25 |
32 |
14.9 |
|
26-35 |
58 |
27.0 |
|
36-45 |
45 |
20.9 |
|
46-55 |
47 |
21.9 |
|
56-65 |
26 |
12.0 |
|
>65 |
7 |
3.3 |
|
Sex |
|
|
|
Male |
138 |
64.2 |
|
Female |
77 |
35.8 |
|
Place |
|
|
|
Rural |
190 |
88.0 |
|
Urban |
25 |
12.0 |
|
Marital status |
|
|
|
Married |
193 |
89.8 |
|
Unmarried |
17 |
7.9 |
|
Widowed |
5 |
2.3 |
|
Religion |
|
|
|
Hindu |
189 |
87.9 |
|
Muslim |
26 |
12.1 |
|
Education |
|
|
|
Illiterate |
32 |
14.9 |
|
Primary |
117 |
54.4 |
|
Secondary |
51 |
23.7 |
|
PUC |
14 |
6.5 |
|
Graduate |
1 |
0.5 |
|
Type of Family |
|
|
|
Nuclear |
187 |
87.0 |
|
Joint |
28 |
13.0 |
|
Socioeconomic class |
|
|
|
Upper class |
4 |
1.9 |
|
Upper middle class |
8 |
3.7 |
|
Middle class |
55 |
25.6 |
|
Lower middle class |
43 |
20.0 |
|
Lower class |
105 |
48.8 |
The above table – 1 shows that out of 215 study participants, majority (27%) of them belonged to age group of 26-35 yrs followed by 46-55 yrs (21.9%) and 36-45 yrs (20.9%). This shows that most of the study participants were in reproductive age 36 group. In our study males were predominant i.e. 64.2% (138) and females constituted 35.8% (77). 88% of the tuberculosis patients were from rural background. 89.8% of the study participants were married and only 7.9% were unmarried and there were about 2.3 % widowed participants in the study. 87.9% of study participants belonged to Hindu religion and rest of them i.e. 12.1% belonged to Muslim community. More than half (54.4%) of the study participants studied up to primary school followed by secondary school (23.7%) and there were 14.9% of illiterates in the study. In this study 87% (187) of the participants belonged to nuclear family while 13% (28) were from the joint family. In our study 48.8% of the participants belonged to lower class according to modified B G Prasad’s classification followed by 25.6% to middle class and 20% to lower middle class.
 |
Figure 1: Distribution of cases according to IP/CP (n= 215) |
In Figure 1- Out of 215 study participants, 74% (159) were in the continuation phase of the TB treatment and 26% (56) were in the intensive phase.
Table 2: Distribution of cases according to Treatment Adherence (n=215)
|
Treatment Adherence |
N |
Percent |
|
No |
23 |
10.6 |
|
Yes |
192 |
89.4 |
|
Total |
215 |
100.0 |
The above table- 2 details the prevalence of Anti-TB treatment adherence. It was found that nearly 10.6% of the study participants were non-adherent to the treatment course.
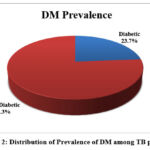 |
Figure 2: Distribution of Prevalence of DM among TB patients. |
In Figure – 2 Out of 215 study participants the prevalence of diabetes mellitus was 23.7% (51).
Table 3: Distribution of behavioural patterns among participants with DM (n=51).
|
Study variable |
Number(n) |
Percentage (%) |
|
Food Habits |
|
|
|
Vegetarian |
25 |
49 |
|
Mixed |
26 |
51 |
|
Smoking |
|
|
|
Current smoker |
22 |
43.1 |
|
Ex-Smoker |
26 |
51 |
|
Non-Smoker |
3 |
5.9 |
|
Alcohol Consumption |
|
|
|
Alcoholic |
15 |
29.4 |
|
Non-Alcoholic |
36 |
70.6 |
|
Occupation |
|
|
|
Non-Government |
39 |
76.5 |
|
Government |
4 |
7.8 |
|
Housewife |
7 |
13.7 |
|
Student |
1 |
2 |
|
Physical Activity |
|
|
|
Sedentary |
2 |
3.9 |
|
Moderate |
46 |
90.2 |
|
Heavy |
3 |
5.9 |
Table -3 details are as follows; When looking at the food habits of the study participants 49 % were vegetarians and 51% used to consume both vegetarian and non-vegetarian food items. 43.1% of the study participants were current smokers and 51s% were ex-smokers; however, 5.9% were non-smokers. A majority (70.6%) of the study participants were non-alcoholic and about 29.4 % used to consume alcohol. Most (90.2%) of the study participants were engaged in moderate activity followed by 3.9% and 5.9% in sedentary and heavy work respectively.
Discussion
Our study showed that the majority of the tuberculosis patients were in the age group of 26-35 years (27%). Similar results were found in a study done4 in Addis Ababa Ethiopia where the majority of the patients were 25- 44 years of age. A study done5 in Kerala revealed that most of the patients were 45-54 years of age. Few other studies done6 in Patiala Punjab and in Ahemdabad7 reported 40-60 years’ age group as most commonly involved. This difference in an age group may be due to the different locations of the study and study design setting. The mean age was found to be 52.1 yrs among diabetics and 37.1 among non-diabetics which is similar to a study8 in Tamil Nadu where themean age of the DM TB patients was 52.92 yrs and was statistically significant. In Andhra Pradesh showed the mean age as 46.5±10.3 among diabetics and 35.8±11.7 among non-diabetics3.
More than half 54.4% (117) tuberculosis patients studied up to primary schooling, 23.7% (51) patients completed high school education and 14.9% (32) patients were illiterates, where it was observed that most of the TB patients had received less schooling, which was consistent with other studies. A study done9 in Bangladesh reported that 25.1% of the participants had primary schooling, 19.8% had secondary schooling and 40.7% were illiterates. Another study 10 in Pakistan has shown 51.6% as illiterates, 34.7% as primary schooling and 10.7% as secondary schooling.
In our study, 4.7% of participants were current smokers and 69.3% were non-smokers which is in line with a study4 in Ethiopia which revealed 15% as smokers and 85% as non-smokers. But another study done11 in Nigeria showed 4.8% as non-smokers and 95.2% as current smokers. This variation may be due to change in the social scenario.
We found that majority (84.2%) of the TB patients were non-alcoholic and about 15.8% used to consume alcohol similar to a study12 in Tamil Nadu in which 38.9% were non-alcoholic and 1.6% were alcoholic. But another study4 in Ethiopia had no much difference in alcohol consumption i.e 51.7% as non-alcoholic and 48.3% as alcoholic which may be due to different socio- cultural factors.
The prevalence of DM among TB patients in our study was 23.7% which is in consistent reports of other studies13 done in Karnataka State in 2011 where the prevalence was 32%, in Kerala State 44% (2012) and Tamil Nadu State, India 25% (2012). Other studies like an institutional based cross-sectional study3 in Andhra Pradesh showed the prevalence of DM as 30.6%. A facility based cross-sectional study done14 in Puducherry (2017) reported 29% as DM prevalence. In contrast to the above findings, another study done in Nigeria.15 found the prevalence to be 5.7% which could be attributed to the difference in demographic characteristics. We employed American Diabetic Association (ADA) criteria to assess the diabetes mellitus and studied tuberculosis patients registered under RNTCP.
Few of the variables analysed were based on the information obtained by the study participants hence an element of recall bias and masking of data could be present. TB patients registered under RNTCP were included in the study; patients taking treatment in private hospitals may have missed. Among all the TB patients only new sputum-positive pulmonary TB patients were included which may be the limitation. In the present study few risk factors of DM were studied. All other risk factors could not be studied because of lack of resources. The prevalence of DM among TB patients was 23.7% which is quite high so screening of all TB patients should be done just like HIV screening which will help in early diagnosis and proper management of the disease. For DMTB patients, regular blood glucose estimation and treatment should be given in DOTS centres along with anti-TB drugs. Primordial prevention can play an important role in preventing the occurrence of DM. Health education regarding the risk factors and symptoms of DM should be given to high risk groups.
Though the results were found to be consistent with those reported by other authors direct comparisons are not valid for the reasons detailed above and also relate to different criteria used by researchers over time to diagnose both conditions, non-representativeness of patients studied both in terms of number and selection criteria and different settings. A well planned large scale observational study or meta-analysis has the potential to settle the issue.
Conclusion
Routine screening for DM in TB patients is mandatory due to increase in the prevalence of DM which would not only help in early diagnosis but also reduces the complications by proper management and in turn will help in successful outcome of TB treatment.
Conflicts of Interest
There are no conflict of Interest.
Funding Sources
There is no funding sources.
References
- Revised National TB Control Programme Technical and Operational Guidelines for Tuberculosis Control in India 2016.India. p 269.
- Park, K, 2017, Textbook of Preventive and Social Medicine, M/s Banarsidas Bhanot Publishers, Jabalpur.
- Padmalatha, P, Hema, K 2014, ‘Study on prevalence of diabetes mellitus in tuberculosis patients attending a tertiary care hospital in guntur, andhra pradesh’, IndianJournal of Basic and Applied Medical Research,.vol. 4, no. 1, pp. 494-498.
- Damtew, E, Ali, I & Meressa, D 2014, ‘prevalence of diabetes mellitus among active pulmonary tuberculosis patients at st. peter specialized hospital, addis ababa, ethiopia’, World Journal of Medical Science, vol. 11, no.3, pp.389-396.
- Balakrishnan, S, Vijayan, S, Nair, S, Subramoniapillai, J & Mrithyunjayan S 2012, ‘high diabetes prevalence among tuberculosis cases in kerala, india’ Plos One ,vol. 7, no. 10, pp.1-7.
- J, Kishan, K, Gar 2010, ‘tuberculosis and diabetes mellitus: a case series of 100 patients’ , SAARC Journal Of Tuberculosis, Lung Diseases & HIV/AIDS, vol. 7, no. 2, pp.34-38.
CrossRef - Dutt, N, Gupta, A 2014, ‘ a study on diabetes mellitus among cases of pulmonary tuberculosis in a tertiary care hospital, ahmedabad’, National Journal Of Medical Research, vol. 4, no. 4, pp.349-353.
CrossRef - Natarajaboopathy, R, Jayanthi, NN, 2016, ‘a study on prevalence of diabetes and prediabetes in a newly diagnosed tuberculosis patients’, Journal of Evolution of Medical and Dental Sciences, vol. 5, no. 99, pp. 7231-7233.
CrossRef - Sarker, M, Barua, M, Guerra, F,Saha, A, Aftab, A, Latif, AHMM, Mahbub, L, Shyla, I, Akramul, I, 2016, ‘double trouble: prevalence and factors associated with tuberculosis and diabetes comorbidity in bangladesh’, Plos One , vol. 11, no. 10, pp. 1-15.
CrossRef - Tahir, Z, Ahmad, M, Akhtar, AM, Yaqub, T, Mushtaq, MH & Javed H, 2016, ‘diabetes mellitus among tuberculosis patients: a cross sectional study from pakistan’, African Health Sciences, vol. 16, no. 3, pp. 671-676.
CrossRef - Ekeke, N, Ukwaja, KN, Chukwu, JN, Nwafor, CC, Meka, AO, Egbagbe, EE, Soyinka, FO, Alobu, I, Agujiobi, I, Akingbesote, S, Igbinigie, O, Offor, JB, Madichie, NO, Alphonsus, C, Anyim, MC, Mbah, OK & Oshi, DC, 2017, ‘ screening for diabetes mellitus among tuberculosis patients in southern nigeria: a multi-centre implementation study under programme settings’, Scientific Report , vol. 7, pp.1-8.
CrossRef - Viswanathan, V, Kumpatla, S, Aravindalochanan, V, Rajan, R, Chinnasamy, C, Srinivasan, R, Selvam , JM, Kapur , 2012, ‘a prevalence of diabetes and pre-diabetes and associated risk factors among tuberculosis patients in india’, Plos One, vol. 7, no. 7, pp.1-9.
CrossRef - Rajaa S, Krishnamoorthy Y, Knudsen S, et al. Prevalence and factors associated with diabetes mellitus among tuberculosis patients in South India—a cross-sectional analytical study. BMJ Open 2021;11: e050542. doi:10.1136/ bmjopen-2021-05054.
CrossRef - Raghuraman, S, Vasudevan, KP, Govindarajan, S, Chinnakali, P, Panigrahi, KC 2014, ‘prevalence of diabetes mellitus among tuberculosis patients in urban puducherry’, World Journal of Medical Sciences, vol. 6, pp.30-34.
CrossRef - Olayinka, AO, Anthonia, O, Yetunde, K 2013, ‘prevalence of diabetes mellitus in persons with tuberculosis in a tertiary health centre in lagos, nigeria’, Indian Journal of Endocrinology and Metabolism, vol. 17, p. 486-489.
CrossRef








