Ashima Amin1 , Reshma G. Kini 1
, Reshma G. Kini 1 and Archana Bhat3*
and Archana Bhat3*
1Department of Pathology, Father Muller Medical College, Mangalore, Karnataka India.
2Department of General Medicine , Father Muller Medical College, Mangalore, Karnataka, India.
Corresponding Author E-mail:archanaacharya24@fathermuller.in
DOI : https://dx.doi.org/10.13005/bpj/2738
Abstract
Coronavirus 2019(COVID 2019) is a global pandemic and may trigger coagulation dysfunction with extensive micro thrombosis. This study was conducted to evaluate the basic coagulation parameters in symptomatic patients with and without SARI in COVID.It was a prospective comparative cross sectional study to study the prognostic role of these markers in patients with and without SARI (severe acute respiratory illness) and survivors versus non survivors. Demographic characteristics , detailed medical history and platelets, prothrombin time (PT),activated thromboplastin time (APTT), fibrinogen and D dimer was recorded and analysed in both these groups. The independent group t-test and Mann -Whitney U test was used to analyse continuous variables. ROC was plotted for significant variables to obtain area under curve. The average PT for survivors was 14.6s and non survivors was 29.4s and the difference statistically significant. The area under curve for PT was 0.751 and at a cut off value of 13s had a sensitivity of 75% and specificity of 62.5% for predicting severe COVID with SARI. The median value for aPTT for non survivors was 35.5 (IQR 32.5-42.1) and for survivors it was 31.9 (IQR 29.5-35.7) and was significant. The mean values of D dimer for patients without and with SARI was 384 and 2168 mcg/ml and the difference was statistically significant (p=0.00). The D dimer test was the single most test distinguishing survivors and non survivors with an AUC of 0.844.The levels of fibrinogen and CRP was higher in patients with severe COVID and was statistically significant (p=0.001) and (p=0.028).The platelet count was lower in patients with severe COVID but difference was not statistically significant. The basic coagulation markers have a prognostic significance in treatment of COVID atients with and without SARIp.
Keywords
COVID 19; Coagulation Profile; D dimer; SARI; aPTT; PT,2.
Download this article as:| Copy the following to cite this article: Amin A, Kini R. G, Bhat A. Analysis of Clotting Factors in Covid 19: A Study in Indian Patients in a Tertiary Hospital. Analysis of Clotting Factors in Covid 19: A Study in Indian Patients in a Tertiary Hospital. Biomed Pharmacol J 2023;16(3). |
| Copy the following to cite this URL: Amin A, Kini R. G, Bhat A. Analysis of Clotting Factors in Covid 19: A Study in Indian Patients in a Tertiary Hospital. Analysis of Clotting Factors in Covid 19: A Study in Indian Patients in a Tertiary Hospital. Biomed Pharmacol J 2023;16(3). Available from: https://bit.ly/44FAxRK |
Introduction
Coronaviruses are enveloped nonsegmented positive stranded RNA viruses belonging to the family Coronaviridae and the order Nidovirales.4 The virus spreads through direct contact of infected surfaces or through human to human contact through air borne droplet spread.5,6 The virus has mean incubation period of 5.2 days.7 Most common symptoms include nausea, vomiting, fever, fatigue, dry cough, dyspnoea, myalgia, diarrhea, sore throat, rhinorrhea and chest pain.8,9,10Increased mortality in COVID patients is related to severe symptoms like pneumonia, acute respiratory distress syndrome and multi organ failure.11,12 In severe cases, patients may develop acute respiratory distress syndrome (ARDS), with coagulation predominant-type coagulopathy. 13
The coronavirus causing COVID-19 may trigger coagulation dysfunction because it induces abundant release of pro-inflammatory cytokines in various tissues, which can lead to systemic inflammatory response syndrome that damages the microvascular system and thereby activates the coagulation system, leading to generalised small vessel vasculitis and extensive microthrombosis1.14,15 Patients with severe COVID-19 may be at high risk of venous thromboembolism, which may be present in up to 25% of such patients.16 Risk may be exacerbated by the dehydration due to fever and diarrhea, hypotension, and prolonged bed rest characteristic of the disease, all of which are risk factors for coagulation.17Chinese studies have revealed markedly prolonged PT/APTT and elevated D dimer in nonsurvivors in comparision to COVID 19 survivors.13,18 The coagulation parameters have not been completely reported in patients with and without SARS in Indian literature so far. Hence this research project was undertaken to ascertain the differences in coagulation parameters in symptomatic patients with and without SARI.
Aims and Objectives
To evaluate the basic coagulation parameters in symptomatic patients with and without SARI
To study the prognostic role of the basic coagulation parameters in both the clinical forms of disease.
Materials and Methods
This study was a prospective comparative cross sectional study which was undertaken in COVID patients admitted to Father Muller Medical College Hospital over a period of one year from April 2020- April 2021. The Institutional Ethics Committee clearance and prior written informed consent was obtained from the study participants.
The sample size was 96 (48 in each group)
Inclusion Criteria
Adult COVID patients admitted to ward and ICU of this hospital with symptoms of nausea, vomiting, fever, fatigue, dry cough, dyspnoea, myalgia, diarrhea, sore throat, rhinorrhea and chest pain.
Exclusion Criteria
Asymptomatic COVID patients, pregnant COVID patients and paediatric COVID patients.
At the time of admission to the hospital, blood sample was collected for platelets, prothrombin time (PT), activated thromboplastin time (APTT), fibrinogen and D dimer. Demographic characteristics, detailed medical history and basic coagulation was recorded and was analysed. Platelet analysis was done in Beckman Coulter LH 750. PT, APTT and fibrinogen was analysed in ACL TOP 500 and ACL TOP 300.D dimer was analysed by an automated latex enhanced immunoassay on the ACL TOP.
The COVID patients was divided into 2 groups according to presence or absence of severe SARI requiring ICU care The clotting factors was compared between these 2 groups of patients and also survivors and non survivors . The case definition of severe SARI was defined as those patients requiring ICU care with saturation less than 90 % on room air requiring non-invasive or invasive ventilation.
Statistical Analysis
The sample size of 96 was calculated based on the standard deviation 151 of fibrinogen in admitted COVID patients and standard deviation of 83 in outpatient (in reference to previously done study), mean difference of 70, alpha error 5% for 80% power, 2 sided test, sample size required for each group is 48.19 This was calculated using Master 2 software, CMC, Vellore.
Data was analysed using unpaired t test if the results follow normal distribution or else Mann Whitney test will be used. P<0.05 is considered to be significant. Data was analysed using SPSS version 20.
Statistical analysis
Continuous variables were expressed as mean and SD or median and IQR The independent group t test was used to analyse normally distributed continuous variables, and the Mann-Whitney U test was used to analyse non-normally distributed continuous variables. Categorical variables were presented as frequency rates and percentages and analysed using χ² test or Fisher’s exact test as appropriate. Receiver Operative characteristic curves were plotted for significant variables to obtain area under curve.
Results
Table 1: Group Statistics
|
|
Moderate Vs Severe Cases |
N |
Mean |
Std. Deviation |
Std. Error Mean |
|
PT |
Moderate |
48 |
12.8417 |
3.37190 |
.48669 |
|
Severe |
48 |
21.3104 |
31.41860 |
4.53488 |
|
|
INR |
Moderate |
48 |
1.1438 |
.29556 |
.04266 |
|
Severe |
48 |
1.8483 |
2.72371 |
.39313 |
|
|
aPTT |
Moderate |
48 |
37.8875 |
35.36448 |
5.10442 |
|
|
Severe |
48 |
42.3188 |
38.89234 |
5.61363 |
|
Fibrinogen |
Moderate |
48 |
458.1667 |
166.26732 |
23.99862 |
|
Severe |
48 |
621.4583 |
286.98869 |
41.42325 |
|
|
Platelet |
Moderate |
48 |
265770.8333 |
124442.9699 |
17961.79554 |
|
|
Severe |
48 |
198958.3333 |
130473.9247 |
18832.28889 |
|
DDimer |
Moderate |
48 |
382.5417 |
492.35197 |
71.06489 |
|
|
Severe |
48 |
2168.2083 |
3320.43931 |
479.26413 |
|
CRP |
Moderate |
48 |
46.6608 |
60.04235 |
8.66637 |
|
Severe |
48 |
112.7206 |
123.35552 |
17.80484 |
Table 2: Group Statistics Continue
|
|
Non Survivor Vs Survivor |
N |
Mean |
Std. Deviation |
|
PT (survivor Vs Nopn Survivor) |
Survivors |
80 |
14.6100 |
13.11189 |
|
Non Survivors |
16 |
29.4063 |
46.29603 |
|
|
INR (Survivor Vs Non Survivor |
Survivors |
80 |
1.2924 |
1.13967 |
|
Non Survivors |
16 |
2.5144 |
4.01809 |
|
|
aPTT (Survivor Vs Non Survivor |
Survivors |
80 |
35.7925 |
27.59943 |
|
Non Survivors |
16 |
61.6563 |
63.9037 |
|
|
Fibinogen (Survivor vs Non Survivor) |
Survivors |
80 |
518.4875 |
227.27500 |
|
Non Survivors |
16 |
646.4375 |
317.42106 |
|
|
Platelet (Survivor vs Non Survivor ) |
Survivors |
80 |
237600.0000 |
130760.2502 |
|
Non Survivors |
16 |
206187.50000 |
134452.5784 |
|
|
DDimer (survivor vs Non Survivor ) |
Survivors |
80 |
927.4875 |
2344.09279 |
|
Non Survivors |
16 |
3014.8125 |
2755.96904 |
|
|
CRP (Suvivor vs Non Survivors |
Survivors |
80 |
62.1549 |
78.14500 |
|
Non Survivors |
16 |
167.3700 |
154.77387 |
Table 3: Group statistics
|
|
Non Survivor Vs Survivor |
Std. Error Mean |
|
PT (survivor Vs Nopn Survivor) |
Survivors |
1.46595 |
|
Non Survivors |
11.57401 |
|
|
INR (Survivor Vs Non Survivor |
Survivors |
.12742 |
|
Non Survivors |
1.00452 |
|
|
aPTT (Survivor Vs Non Survivor |
Survivors |
3.08571 |
|
Non Survivors |
15.97509 |
|
|
Fibinogen (Survivor vs Non Survivor) |
Survivors |
25.41012 |
|
Non Survivors |
79.35526 |
|
|
Platelet (Survivor vs Non Survivor ) |
Survivors |
14619.44041 |
|
Non Survivors |
33613.14460 |
|
|
DDimer (survivor vs Non Survivor ) |
Survivors |
262.07754 |
|
Non Survivors |
688.99226 |
|
|
CRP (Suvivor vs Non Survivors |
Survivors |
8.73688 |
|
Non Survivors |
38.69347 |
Table 4
|
|
|
Levene’s Test for Equality of Variances |
t-test Equality of Means |
||
|
F |
Sig |
t |
Df |
||
|
PT |
Equal Variances assumed Equal Variances not assumed |
7.767 |
.006 |
-1.857 -1.857 |
94 48.083 |
|
INR |
Equal Variances assumed Equal Variances not assumed |
7.531 |
.007 |
-1.782 -1.782 |
94 48.107 |
|
aPTT |
Equal Variances assumed Equal Variances not assumed |
.815 |
.369 |
-.584 -.584 |
94 93.163 |
|
Fibrinogen |
Equal Variances assumed Equal Variances not assumed |
12.653 |
.001 |
-3.411 -3.411 |
94 75.356 |
|
Platelet |
Equal Variances assumed Equal Variances not assumed |
1.092 |
.299 |
2.567 2.567 |
94 93.790 |
|
DDimer |
Equal Variances assumed Equal Variances not assumed |
18.579 |
.000 |
-3.686 -3.686 |
94 49.066 |
|
CRP |
Equal Variances assumed Equal Variances not assumed |
4.957 |
.028 |
-3.336 -3.336 |
94 68.087 |
Table 5
|
|
|
|
t-test Equality of Means |
|
|
Sig.(2-tailed) |
Mean Difference |
Std. Error Difference |
||
|
PT |
Equal Variances assumed Equal Variances not assumed |
.066 .069 |
-8.46875 -8.46875 |
4.56093 4.56093 |
|
INR |
Equal Variances assumed Equal Variances not assumed |
.078 .081 |
-.70458 -.70458 |
.39544 .39544 |
|
aPTT |
Equal Variances assumed Equal Variances not assumed |
.561 .561 |
-4.43125 -4.43125 |
7.58735 7.58735 |
|
Fibrinogen |
Equal Variances assumed Equal Variances not assumed |
.001 .001 |
-163.29167 -163.29167 |
47.87295 47.87295 |
|
Platelet |
Equal Variances assumed Equal Variances not assumed |
.012 .012 |
66812.50000 66812.50000 |
26024.62687 26024.62687 |
|
DDimer |
Equal Variances assumed Equal Variances not assumed |
.000 .001 |
-1785.66667 -1785.66667 |
484.50421 484.50421 |
|
CRP |
Equal Variances assumed Equal Variances not assumed |
.001 .001 |
-66.05979 -66.05979 |
19.80197 19.80197 |
Table 6
|
|
|
t-test for Equality of Means |
|
|
95% Confidence Interval of the Difference |
|||
|
Lower |
Upper |
||
|
PT |
Equal Variances assumed Equal Variances not assumed |
-17.52458 -17.63870 |
.58708 .70120 |
|
INR |
Equal Variances assumed Equal Variances not assumed |
-1.488974 -1.49963 |
.08058 .09046 |
|
aPTT |
Equal Variances assumed Equal Variances not assumed |
-19.49612 -19.49788 |
10.63362 10.63538 |
|
Fibrinogen |
Equal Variances assumed Equal Variances not assumed |
-258.34453 -258.65208 |
-68.23880 -67.93125 |
|
Platelet |
Equal Variances assumed Equal Variances not assumed |
15139.99328 15138.48669 |
118485.0067 118486.5133 |
|
DDimer |
Equal Variances assumed Equal Variances not assumed |
-2747.66113 -27759.28132 |
-823.67221 -812.05201 |
|
CRP |
Equal Variances assumed Equal Variances not assumed |
-105.37707 -105.57310 |
-26.74251 -26.54648 |
In our study the values of the levels of all five parameters were elevated in non survivors as compared to survivors.
PT
On admission the mean level of PT in patients with and without SARI 12.8s and 21.3s. When interpreted with INR the mean values were 1.1 and 1.8. The difference in the mean values apart from being statistically significant (p=0.006) and also clinically different with moderate patients having a mean value within normal range for our laboratory(10-13s) and the severe cases well above that. Our finding is similar to Song JC15 et al who hypothesized that these are due to liver involvement as there was significant abnormality in the liver enzymes of patients with COVID.
The average PT for survivors was 14.6 and the non survivors was 29.4s and the difference was statistically significant. Area under the curve for PT (survivors non survivor)was 0.751 and at a cut off value of 13s PT alone had a sensitivity of 75 % and a specificity of 62.5% for predicting those with severe covid. A cut off value of 16s had sensitivity to 39.6%. specificity of 95.8 % in predicting death This finding is similar to those described by Cui S et al16 in whose study the multivariate regression analysis showed the difference in PT inpatients with SARI who survived and did not survive was not significant.
 |
Graph 1: Roc Curve |
Table 7
|
t-test Result Variable(s) |
Area |
a |
Asymptotic Sig.b |
Asymptotic 95% confidence Interval |
|
|
Std Error |
Lower Bound |
Upper Bound |
|||
|
PT |
.735 |
.051 |
.000 |
.635 |
.835 |
|
INR |
.724 |
.052 |
.000 |
.623 |
.825 |
|
aPTT |
.535 |
.059 |
.558 |
.418 |
.651 |
|
Fibrinogen |
.667 |
.055 |
.005 |
.559 |
.775 |
|
Platelet |
.350 |
.057 |
.011 |
.239 |
.461 |
|
DDimer |
.852 |
.039 |
.000 |
.775 |
.928 |
|
CRP |
.740 |
.051 |
.000 |
.639 |
.840 |
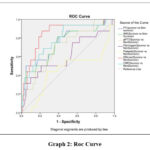 |
Graph 2: Roc Curve |
Area Under the Curve
Table 8
|
Test Result Variables |
Area |
Std. Error |
Asymptotic sig. |
Asymptotic 95% Confidence |
|
PT (survivor vs Non survivor) |
.751 |
.073 |
.002 |
.607 |
|
INR (Survivor Vs Non Survivor |
.738 |
.073 |
.003 |
.506 |
|
aPTT (Survivor Vs Non Survivor |
.705 |
.069 |
.010 |
.570 |
|
Fibinogen (Survivor vs Non Survivor) |
.615 |
.087 |
.147 |
.445 |
|
Platelet (Survivor vs Non Survivor ) |
.448 |
.090 |
.513 |
.272 |
|
DDimer (survivor vs Non Survivor ) |
.644 |
.057 |
.000 |
.732 |
|
CRP (Suvivor vs Non Survivors |
.784 |
.064 |
.000 |
.658 |
The prolongation of PT is understandable. One of the mechanisms of COVID induced coagulopathy (CIC) is the over expression of tissue factor (TF) by the endothelial cells secondary to the cytokine release. Binding activation and consumption of factor VII by TF is probably the main reason for this. It can be inferred that the consumption of factor VII occurs more severely in SARI than in non SARI cases due to stronger cytokine response in them.
aPTT
The difference in aPTT among the moderate and sever cases was not statistically significant. This finding is similar to other studies. However the difference was significant when aPTT was survivors was compared with non survivors. (p=0.003) The median value for non survivors was 35.5 (IQR 32.5-42.1) and for survivors it was 31.9 (IQR 29.5-35.7) This finding is similar to that of study done by Huang C 11 et al.
It has been suggested that CIC be categorized into three stages beginning with stage of high d-dimer and nerar normal PT and aPTT, followed by increasing PT and aPTT with high dDimer and finally with features of Classic DIC as described by International Society of Thrombosis and Hemostasis (ISTH) It is possible that the non survivors in our case had progressed to second stage as compared to our survivors . It is interesting to note that the difference in the aPTT between survivors with and without SARI was also not significant as well as between the SARI survivors and non survivors.
33.9 cut off 21 severe patients and 18 moderate patients
>33.9s in 11/16 non survivors(68.5%) 36.2 5% (of survivors 29/80)
D Dimer (D-DU) (non survivor vs survivor and Non Sari vs Sari). The mean values of D dimer for patients without and with SARI as 384 and 2168 mcg/ml and the difference was highly significant. The IQR of D dimer in survivors and non survivors was 196-817 and 1043-4961 and the median was 352 and 2080 between survivors and non survivors difference was statistically significant ( p<0.001)
The D Dimer test was the single most important test distinguishing survivors and non Survivors with an AUC of. 0.844. At values if 382 the sensitivity and specificity was 93.8 and 51, 2. A cut off of 1000 ensured a 81.3 and 81.2% specificity. At 1711 it was 56.3 and 90% respectively. Our findings is similar to Gao Y.D. et al 20 also is the most common hematological abnormality reported in COVID-19 in a study done Asakura H, Ogawa H21 . Elevated D-dimer level is a sign of excessive coagulation activation and hyperfibrinolysis which is a significant predictor of mortality due to venous thromboembolism both of the deep veins and in the pulmonary circulation the prevalence of which ranges from 0-54% as shown in a study by Suh et al22
The mean levels of fibrinogen values in our study in moderate and severe cases was 458 and 621 respectively and the difference was significant (p =. 001) .The CRP The levels of fibrinogen and CRP was higher in patients with severe COVID and the difference was statistically significant whereas platelet values were lower but difference was not significant
Discussion
The aim of the cross-sectional study was to analyze the association between the coagulation parameters on admission with the severity and survival of adult
COVID patients as thromboembolism and disseminated Intravascular Coagulation are an important cause of morbidity and mortality among COVID patients.
Early on it was discovered that the mechanism for development of DIC in patients with COVID differed from those commonly encountered during sepsis. It is believed that the release of cytokines especially the Interleukin -6(IL-6) is major contributor for development of macrovascular as well as microvascular thrombosis. The mechanism appears to be dual:1. IL -6 increases the endothelial expression of Tissue Factor, ii) Sars Co-V 2 by itself produces widespread endothelitis and also pyroptosis and apoptosis of endothelial cells.
The coagulation cascade activation that occurs I Covid can be identified by prolongation of Prothrombin Time, Activated Partial Thromboplastin Time (aPTT). The fibrinolysis that follows is represented by increased levels of D- Dimer and Fibrin Split Products (FSP). The other conventional laboratory parameters that are useful in monitoring of Covid patients is levels of Lactate Dehydrogenase (LDH ), Serum Ferritin, C- Reactive Protein(CRP) and Interleukin 6 levels.
In our study the values of the levels of all five parameters were elevated in non survivors as compared to survivors
On admission the mean level of PT in patients with and without SARI 12.8s and 21.3s. When interpreted with INR the mean values were 1.1 and 1.8. The difference in the mean values apart from being statistically significant (p=0.006) also clinically different with moderate patients having a mean value within normal range for our laboratory (10-13s) and the severe cases well above that. Our finding is similar to Zhang et al23 who hypothesized that these are due to liver involvement as there was significant abnormality in the liver enzymes of patients with COVID.
The levels of fibrinogen and CRP was higher in patients with severe covid and the difference was statistically significant whereas platelet values were lower but difference was not significant.
Platelet values are known to be lower in patients with severe Covid and multiple mechanisms are proposed beginning with suppression of bone marrow to increased consumption. Lower platelet counts are associated with more severe disease and are useful if monitored serially24. Since we did not follow up platelet counts and it may be the reason that it was not statistically significant. In our study 20 severe and 6 moderate cases had levels below 1,50,000
Both fibrinogen and CRP elevation can be explained by the fact that they are acute phase reactants. Elevation of fibrinogen could also be an indicator of prothrombotic state as shown in study done by Thachil J25 and in conjunction with elevated CRP gives credence to the connection between inflammation and coagulation.
Conclusion
Basic coagulation markers may have a prognostic implication in the treatment of Covid patients with and without SARI.
Acknowledgement
The authors would like to acknowledge Father Muller Medical College hospital , Mangalore to allow us to carry out the present study .
Conflicting of Interests
There are no conflict of interest.
Funding Sources
Father muller research grant ,Father Muller Medical College , Mangalore -575002 grant number FMRC/FMMC/06/2020.
References
- Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020;395:497–506.
CrossRef - Zhu N, Zhang D, Wang W, Li X, Yang B, Song J,et al. A Novel Coronavirus from Patients with Pneumonia in China.New England Journal Of Medicine 2019; 382: 727–733.
CrossRef - Coronavirus disease 2019 (COVID-19) Situation Report – 69 [Accessed: July, 2020]. Available from: https://www.who.int/docs/default-source/coronaviruse/ situation-reports/20200329-sitrep-69-covid-19.pdf.
- de Groot, RJ, King AMQ , Adams MJ, Carstens EB, Lefkowitz EJ. et al. in Virus Taxonomy, Ninth Report of the International Committee on Taxonomy of Viruses.2012;Elsevier Academic Press: 806-828
- Chen G, Wu D, Guo W, et al. Clinical and immunological features of severe and moderate coronavirus disease 2019. J Clin Invest. 2020; 130 (5): 2620-29.
CrossRef - Rothan HA, Byrareddy SN. The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak. J Autoimmun. 2020; 109: 102433
CrossRef - Li Q ,Guan X,Wu P,Wang X,Zhou L,Tong Y et al. Early transmission dynamics in Wuhan, China, of Novel Coronavirus–Infected Pneumonia. New England Journal of Medicine. 2020;382(13):1199–1207.
CrossRef - Jin X,Lian J,Hu J,Gao J,Zheng L,Zhang Y. et al.Epidemiological, clinical and virological characteristics of 74 cases of coronavirus-infected disease 2019 (COVID-19) with gastrointestinal symptoms. Gut 2020;69:1002–1009.
CrossRef - Chakroborty C,Sharma AR,Sharma G,Bhattacharya M, Lee SS .SARS-CoV-2 causing pneumonia-associated respiratory disorder (COVID-19): diagnostic and proposed therapeutic options.European Review for Medical and Pharmacological Sciences 2020; 24: 4016-4026
- Hui DS, Azhar E, Madani TA, Ntoumi F, Kock R, Dar O et al. The continuing 2019-nCoV epidemic threat of novel coronaviruses to global health– The latest 2019 novel coronavirus outbreak in Wuhan, China. Int J Infect Dis 2020; 91: 264-266.
CrossRef - Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020; 395: 497-506.
CrossRef - Zhou F, Yu T, Du R, Fan G, Liu Y, Liu ZWang et al. Clinical course and risk factors for mortality of adult in patients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 2020;6736:1–9
CrossRef - Tang N, Li D, Wang X, Sun Z (2020) Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemost 18:844–847.
- .Chousterman BG, Swirski FK, Weber GF. Cytokine storm and sepsis disease pathogenesis. Semin Immunopathol. 2017;39(5):517–28.
CrossRef - Song JC, Wang G, Zhang W, et al. Chinese expert consensus on diagnosis and treatment of coagulation dysfunction in COVID-19.Mil Med Res,2020,7(1):1 9
CrossRef - Cui S, Chen S, Li X, et al. Prevalence of venous thromboembolism in patient s with severe novel coronavirus pneumonia.J Thromb Haemosta, 2020;18(6):1421-1424.
CrossRef - Zhou B, She J, Wang Y. Venous thrombosis and arteriosclerosis obliterans of lower extremities in a very severe patient with 2019 novel coronavirus disease: a case report. J Thromb Thrombolysis, 2020;50(1):229-232
CrossRef - Wang L, He WB, Yu XM, et al.Coronavirus Disease 2019 in elderly patients: characteristics and prognostic factors based on 4-week follow-up.J Infect.2020; 80(6):639-645.
CrossRef - Lagadinou M , Solomou EE , Zareifopoulos N ,Marangos M , Gogos C , Velissaris D. Prognosis of COVID-19: Changes in laboratory parameters .Le Infezioni in Medicina 2020: 1: 89-95.
- Gao Y.D.,Ding M.,Dong X.,ZhangJ.J.,Kursat Azkur A.,Azkur D.,Gan H.,Sun Y.L.,Fu W., Li W.,et al .Risk factors for severe and critically ill COVID -19 patients :A review .Allergy .2021:76:428-455.doi:10.1111/all.14657
CrossRef - Asakura H,Ogawa H.,COVID 19 -associated coagulopathy and disseminated intravascular cogulation Int J Hematol.2021;113(1): 45-57 .doi 10.1007/s12185-020-03029-y
CrossRef - YJ Suh , H Hong ,M Ohana ,F Bompard ,M-P Revel ,C Valle et al. Pulmonary Embolism and Deep Vien Thrombosis in COVID -19 : A Systematic review and Meta – Analysis Radiology ,298(2021) ,pp .E70-E80, 10.1148/ radiol.2020203557
CrossRef - Zhang C,Shi L,Wang FS .Liver injury in COVID-19 :management and challenges .Lancet Gastroenterol Hepatol.2020; 5(5) :428-430 .doi :10.1016/S2468-1253(20)30057-1
CrossRef - Rohlfing AK, Rath D, Geisler T, Gawaz M. Platelets and COVID-19. Hamastaselogie .2021Oct ; 41(50) : 379-385 .doi : 10.1055/a-1581-4355
CrossRef - Thachil J.The protective rather than prothrombotic fibrinogen in COVID-19 and other inflammatory states .J Thromb Haemost .2020 Aug ; 18(8) :1849-1852 .doi: 10.1111/jth.14942.
CrossRef








