Mugdha Kamble1* , Manju Toppo1
, Manju Toppo1 , Aseem2
, Aseem2 , Archa Sharma2
, Archa Sharma2 and Syed Zia Husain1
and Syed Zia Husain1
1Department of Community Medicine, Gandhi Medical College, Bhopal, India,
2Department of Microbiology, Gandhi Medical College, Bhopal, India
Corresponding Author E-mail: mugdhak1207@gmail.com
DOI : https://dx.doi.org/10.13005/bpj/2701
Abstract
Only 44% of Indians were found to be correctly using masks, according to the latest survey.1,2 91.5% of participants did not wash their hands before using the mask, and 97.3% did not wash their hands after removing it.3 People touch their faces about 23 times every hour, and of those touches, 44% make contact with the mucosal membranes. The mucous membrane of the nose, eyes, and mouth can be self-inoculated, which is a significant method of virus transmission.3 To determine the bacterial load and microbial contamination on the mask, this study was designed with the objective: 1. To study the bacterial load and type of microbes growing on masks in Hamidia Hospital premises. 2. To suggest appropriate recommendations according to the study findings. A cross-sectional comparative study was planned in Hamidia Hospital for three months. Two groups were selected one containing 31 healthcare workers and the other constituting 30 general population visiting Hamidia Hospital. Result and conclusion: This study shows that the prolonged use of a mask (>6 hours) increases the risk of self-inoculation in the general population and frequent clinical contact in a healthcare setting adds to the risks for healthcare workers. Reuse of single-use masks, sharing of masks, and fabric masks should be avoided at all costs. Hand hygiene practices and replacing masks once they become damp are of key importance to avoid contamination. Additionally, it is usually advisable to discard medical face masks after each usage, whereas cotton face masks should be carefully cleaned.
Keywords
Contaminated Masks; Masks; prolonged mask usage; risks
Download this article as:| Copy the following to cite this article: Kamble M, Toppo M, Aseem A, Sharma A, Husain S. Z. Contamination of Face Masks and Mask Hygiene Amongst Health Care Workers and General Population in Hamidia Hospital Premises- A Comparative Study. Biomed Pharmacol J 2023;16(2). |
| Copy the following to cite this URL: Kamble M, Toppo M, Aseem A, Sharma A, Husain S. Z. Contamination of Face Masks and Mask Hygiene Amongst Health Care Workers and General Population in Hamidia Hospital Premises- A Comparative Study. Biomed Pharmacol J 2023;16(2). Available from: https://bit.ly/3M60u4B |
Introduction
The use of masks is one component of preventative and control methods that reduce the spread of COVID-19 and other respiratory viral infections. Masks can be worn by an infected person to act as a source controller and prevent the spread of an infection, or by healthy individuals to protect themselves from getting infected.1,2,4
A recent survey noted that only 44% of Indians wear masks properly, in compliance with the guidelines.1,2 Before putting the mask on and after taking it off, 91.5% and 97.3% of people, respectively, did not wash their hands.3
Face masks should only be worn as recommended in standard guidelines. Since they are frequently reused and worn for extended periods, respiratory infections produced by coughing, sneezing, and breathing can infect many who wear them over a longer period. Approximately 23 times an hour, people touch their faces, and of that, 44% involve mucous membrane contact. An important way of virus transmission is through the self-inoculation of the mucous membranes of the nose, eyes, and mouth.3
The usage of both fabric and medical masks is generally believed to be safe, albeit this has not yet been discussed or thoroughly researched. Studies on the effectiveness of masks typically ignore the possibility that human saliva and exhaled air include bacteria that provide a biosafety risk, mainly when masks are worn for an excessive amount of time, improperly kept, or reused without being properly disinfected. Human saliva harbors approximately 100 million bacteria per milliliter. It is inhabited by a wide range of pathobionts, such as Staphylococcus aureus, Pseudomonas aeruginosa, Candida albicans, Klebsiella pneumoniae, Neisseria, Prevotella, and Veillonella species. 3,5–7 Similarly, cotton serves as a medium for microbial development and is ideal for retaining humidity, making cotton masks susceptible to heavy microbial contamination in comparison to surgical masks.3,8
Currently there is limited data on the presence of respiratory pathogens on surface of PPE and other fomites in hospital settings. This study was therefore planned to find out the bacterial load and microbial contamination on the mask.
Objective
To study the bacterial load and type of microbes growing on masks in Hamidia Hospital premises.
To suggest appropriate recommendation according to the study findings.
Methodology
A cross-sectional comparative study was planned in Hamidia Hospital for three months. Two groups were selected one containing 31 healthcare workers and the other constituting 30 general population visiting Hamidia Hospital. Simple random sampling was used to select the study participants in each group.
Study plan
After taking permission from Institutional Ethical Committee and microbiology department, blood agar and BHI broth for culture and zip lock bags for carrying the masks were brought. The flow chart given below describes in detail the study procedure.
 |
Figure 1: Study Plain |
Results and Observations
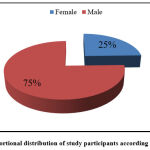 |
Figure 2: Proportional distribution of study participants according to their gender. |
Figure 2, illustrates that male were in majority proportion amongst the study participants.
Table 1: Distribution of study participants according to occupation
| Health care worker | Occupation | Frequency | Percentage |
| Doctor | 10 | 14.8 | |
| Nursing staff | 8 | 13.1 | |
| Ward boy | 7 | 11.5 | |
| Lab tech | 3 | 4.9 | |
| Sweeper | 3 | 4.9 | |
| Community | Guard | 4 | 6.6 |
| Labour | 8 | 13.1 | |
| Farmer | 7 | 11.5 | |
| Mechanic | 1 | 1.6 | |
| Driver | 3 | 4.9 | |
| Police | 1 | 1.6 | |
| Shopkeeper | 4 | 6.6 | |
| Student | 2 | 3.3 | |
|
Total |
61 | 100.0 | |
Tables 1, amongst the health care workers, doctors were in maximum proportion followed by nurses whereas, in the community group, laborers followed by farmers were the majority participants.
 |
Figure 3: Distribution according to type of mask preferred. |
Figures 3, the majority proportion of participants collectively were wearing surgical masks and only a few of them were wearing N-95 and fabric masks.
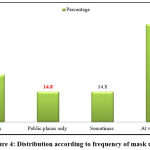 |
Figure 4: Distribution according to frequency of mask usage |
Figure 4, illustrates the masks wearing preferences of study participants, the majority of them preferred wearing masks at the work place whereas very few proportions preferred wearing masks in public places only.
Table 2: Factors associated with mask wearing and hygiene practices among HCW and community people.
| Variables | Mask from HCW | Mask from Community | Total | Chi-Square | p-value | |
| Is the mask
|
Clean | 24 (77.4) | 4 (13.3) | 28 | 25.215
|
0.000
|
| Dirty | 7 (22.6) | 26 (86.7) | 33 | |||
| Covering nose | No | 10 (32.3) | 18 (60) | 28 | 4.725
|
0.030
|
| Yes | 21 (67.7) | 12 (40) | 33 | |||
| How often do you change mask | 6 hours | 0 | 1 (3.3) | 1 | 1.788
|
0.618
|
| 12 hours | 5 (16.1) | 7 (23.3) | 12 | |||
| 24 hours | 7 (22.6) | 7 (23.3) | 14 | |||
| Dispose after single use | 19 (61.3) | 15 (50) | 34 | |||
| How long have you been wearing mask | < 6 hours | 0 | 4 | 4 | 8.547 | 0.036 |
| >6 hours | 31 (100) | 26 (86.7) | 57 | |||
| Do you reuse mask after it has fallen on ground | No | 27 (87.1) | 24 (80) | 51 | 0.560
|
0.454
|
| Yes | 4 (12.9) | 6 (20) | 10 | |||
| Do you clean your hands before and after changing mask | No | 4 (12.9) | 11(36.7) | 15 | 4.643
|
0.031
|
| Yes | 27(87.1) | 19(63.3) | 46 | |||
| Do you reuse the same mask after wearing it once without washing next day? | No | 20 (64.5) | 15 (50) | 35 | 1.714
|
0.190
|
| Yes | 10 (32.2) | 15 (50) | 25 | |||
Table 2, elucidates the association of mask-wearing practices in both the group of study participants. There was a statistical difference among both groups in wearing a mask covering the nose, duration of wearing a mask, and practicing hand hygiene. Amongst the health care workers, most of them had their noses covered while wearing masks, all the health care workers were wearing the same mask for more than 6 hours and practiced appropriate hand hygiene, in comparison to the community group.
Table 3: Distribution according to the type of bacterial growth.
| BACTERIA (species) | Frequency | Percentage |
| Bacillus | 22 | 36.1 |
| Staphylococcus aureus | 11 | 18.0 |
| Klebsiella pnemoniae | 7 | 11.4 |
| Micrococcus | 5 | 8.2 |
| Acinetobacter | 1 | 1.6 |
| Bacillus and micrococcus | 1 | 1.6 |
| Citrobacter | 1 | 1.6 |
| Diphtheroids | 1 | 1.6 |
| Escherichia coli | 1 | 1.6 |
| No growth | 11 | 18.0 |
| Total | 61 | 100.0 |
Table 3, shows the type of bacterial growth found in the masks. Bacillus was the most common type followed by S. aureus and K. pneumonia. 18% of the masks did not have any bacterial growth in them.
Table 4: Association of pathogenic growth with both the group.
| Group | Pathogenic | Total | Chi-square value | p-value | |
| No | Yes | ||||
| HCW | 10 | 21 | 31 | 1.183 | 0.276 |
| Community | 6 | 24 | 30 | ||
| Total | 16 | 45 | 61 | ||
Table 4, divulges that the majority of the masks from the community group showed pathogenic bacterial growth whereas two third of masks from the HCW group showed pathogenic bacterial growth. The difference between the two groups was not statistically significant.
Table 5: Association of bacterial load and both the group
| Group | Colony forming unit per ml (CFU/ml) | Total | |||
| 0 | 103 | 104 | 105 | ||
| HCW | 8 | 10 | 4 | 9 | 31 |
| Community | 3 | 15 | 3 | 9 | 30 |
| Total | 11 | 25 | 7 | 18 | 61 |
Table 5, shows the bacterial load in the masks in both groups. The majority of the participants in both groups had a bacterial load of 103 CFU/ml followed by 105 CFU/ml which is considered a heavy bacterial load to cause infection.
Table 6: Association of pathogenic growth and duration of mask worn by the participants.
|
|
Pathogenic growth | Total | Chi-Square | p-value | ||
| No | Yes | |||||
| How long have you been wearing mask | 6 hours | 2 | 2 | 4 | 8.198a |
0.042 |
| 12 hours | 1 | 10 | 11 | |||
| 24 hours | 2 | 17 | 19 | |||
| >1 days | 11 | 16 | 27 | |||
| Total | 16 | 45 | 61 | |||
Table 6, shows the association between the duration of the mask worn and the pathogenic growth seen. The more the duration of a mask worn more is the chance of it having pathogenic bacterial contamination.
Discussion
This study shows that the prolonged use of masks (>6 hours) increases the risk of self-inoculation in the general population and frequent clinical contact in a healthcare setting adds to the risks for healthcare workers. Reuse of single-use masks, sharing of masks, and fabric masks should be avoided at all costs. Hand hygiene practices and replacing masks once they become damp are of key importance to avoid contamination. Additionally, it is usually advisable to discard medical face masks after each usage, whereas cotton face masks should be properly cleaned.
This study has provided new data which will help in developing policies for mask hygiene in workplaces and public places especially when the new COVID variants are constantly striking. Large scale study is needed to generate proper evidence regarding the microbial contamination of masks.
According to a study by Marn-Nieto J et al.6, there were more bacteria in the >4 hours group (13.2 vs. 48.75 colony-forming units/L; P = 0.03) than in the 4 hours group. After 4 hours of use, Lize D. et al.3 found that microorganisms, and more especially pathobionts, accumulate on both surgical and more so on cotton face masks. Due to a decreased bacterial load, surgical masks might be a preferable choice when the same face mask is worn for extended periods. Longer mask use significantly increased the number of fungal colonies, but not the number of bacterial colonies, according to Parl A et. al.7 observation.
Conclusion
With increased disseminated guidelines of mask usage protocols of mask hygiene should also be advocated thoroughly. The bacterial growth and load found on the masks can be hazardous specifically for people having immune-compromised conditions like DM and PLHIV hence special attention and care should be practiced regarding mask usage in this group. Additionally, health workers not following the protocols despite being aware of them sets a poor example to the rest of the community. The usage of masks for longer duration should be avoided at all costs.
Limitations
Due to funding constraints, we could conduct a study on only 61 masks, and fungal growth could not to assess.
Acknowledgment
We would like to extend our heartfelt gratitude to the Dean of GMC, Bhopal to permit us to conduct this research and Microbiology Department to provide us with the guidance and assistance required in completing this research work.
Conflict of Interest
There is no conflict of interest
References
- When and how to use masks. Accessed February 28, 2023. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public/when-and-how-to-use-masks
- Reporter S. Only 44% wear mask correctly, shows survey. The Hindu. https://www.thehindu.com/news/national/karnataka/only-44-wear-mask-correctly-shows-survey/article32614925.ece. Published September 15, 2020. Accessed February 28, 2023.
- L D, E C, I S, et al. Cotton and Surgical Face Masks in Community Settings: Bacterial Contamination and Face Mask Hygiene. Front Med. 2021;8. doi:10.3389/fmed.2021.732047
CrossRef - Guidance on mask use in the context of COVID-19 | OpenWHO. Accessed February 28, 2023. https://openwho.org/courses/COVID-19-mask-use
- Zhiqing L, Yongyun C, Wenxiang C, et al. Surgical masks as source of bacterial contamination during operative procedures. J Orthop Transl. 2018;14:57-62. doi:10.1016/j.jot.2018.06.002
CrossRef - FACE MASK CONTAMINATION DURING COVID-19 PANDEMIA. A STUDY ON PATIENTS RECEIVING INTRAVITREAL INJECTIONS – PubMed. Accessed February 28, 2023. https://pubmed.ncbi.nlm.nih.gov/33965993/
- Bacterial and fungal isolation from face masks under the COVID-19 pandemic | Scientific Reports. Accessed February 28, 2023. https://www.nature.com/articles/s41598-022-15409-x
- Contamination and washing of cloth masks and risk of infection among hospital health workers in Vietnam: a post hoc analysis of a randomised controlled trial | BMJ Open. Accessed February 28, 2023. https://bmjopen.bmj.com/content/10/9/e042045
CrossRef








