Hatem Hamed Elatroush1 , Tarek Samy Essawy2
, Tarek Samy Essawy2 , Mahmoud Mohamed Kenawy1
, Mahmoud Mohamed Kenawy1 , Ahmed Samir Abd El Aziem Karoub3 and Amira Mohamed Ismail1
, Ahmed Samir Abd El Aziem Karoub3 and Amira Mohamed Ismail1
1Critical care department, Faculty of Medicine, Cairo University, Cairo, Egypt.
2Pulmonology and chest diseases department, Faculty of Medicine, Benha University, Benha, Egypt.
3Critical care department, Shibin El Kom Teaching Hospital, Menoufia, Egypt.
Corresponding Author E-mail: drahmadsamir2013hana@gmail.com
DOI : https://dx.doi.org/10.13005/bpj/2634
Abstract
Background: Lung ultrasound is a new diagnostic tool for diagnosis of acute chest conditions. The aim of the current study was to assess the accuracy of lung ultrasound algorithm in intensive care unit (ICU) patients with respiratory failure. Methods: This is a randomized comparative study included 80 patients admitted to the intensive care unit, Shebin El-Kom Teaching Hospital during three years from October 2017- October 2020. The study received the approval of ethical committee of faculty Medicine, Kasr- El-Einy, Cairo University. History, clinical examination, Chest X ray, Computed tomography (CT) chest, lung US, and Echocardiography were done. Results: Ultrasonography (US) showed sensitivity and specificity 100 %, 100% respectively in diagnosis of pneumothorax Regarding pneumonia, sensitivity and specificity of US were (68.2%, 86.2% respectively). Regarding interstitial lung disease (ILD), sensitivity and specificity of US were (55.6%, 98.6%). Additionally, as regard pulmonary edema and pleural effusion, US sensitivity and specificity were (66.7%, 97.4%) and (78.9%, 98.4%) respectively. Conclusion: In comparison with CT scan, bedside lung ultrasonography (LUS) seems to be a valuable substitute in cases where performing CT is problematic. We recommend starting the use of bedside LUS as routine tool to improve the diagnostic accuracy for most of the pulmonary presentations.
Keywords
Acute respiratory failure; CT chest; Interstitial lung disease; Intensive care unit; Lung Ultrasonography
Download this article as:| Copy the following to cite this article: Elatroush H. H, Essawy T. S, Kenawy M. M, Karoub A. S. A. E. A, Ismail A. M. The Assessment of the Diagnostic Accuracy of Bedside Lung Ultrasound in Critically Ill Respiratory Failure Patients. Biomed Pharmacol J 2023;16(1). |
| Copy the following to cite this URL: Elatroush H. H, Essawy T. S, Kenawy M. M, Karoub A. S. A. E. A, Ismail A. M. The Assessment of the Diagnostic Accuracy of Bedside Lung Ultrasound in Critically Ill Respiratory Failure Patients. Biomed Pharmacol J 2023;16(1). Available from: https://bit.ly/41ExDLS |
Introduction
A critical illness is a condition that poses a significant risk of mortality or morbidity. The implementation of an efficient Chain of Response, which involves precise vital sign recording with recognition and interpretation of aberrant data, patient assessment, and appropriate response, involves all healthcare staff significantly .1 Rapid diagnosis and conclusive therapy are necessary for positive results.1, 2
Acute respiratory failure (ARF) is a serious illness that needs constant monitoring and treatment. A noninvasive, widely accessible imaging technique called bedside lung ultrasonography (LUS) can support clinical evaluation and physical examination.3 The fundamental benefit of bedside LUS, is that it can be used right away to diagnose thoracic diseases. Other benefits include delaying or even avoiding the need for patient transportation to the radiology suite or for radiation exposure, as well as directing life-saving therapies in the event of an urgent situation. Numerous studies have documented the use of LUS by pulmonologists, and emergency doctors.3, 4
Traditionally, thoracic computed tomography (TCT) or bedside chest X-ray (CXR) were used for lung imaging in critically unwell patients (CT). Both methods have drawbacks that restrict how beneficial they can be. Critically, although appearing to be a new area, ultrasonography is the result of a long effort that started in 1946. The lung was traditionally not considered as a part of ultrasound, now it is included as a priority in the critical ultrasound. 5
Among intensivists, the idea of employing bedside ultrasound to examine the lung is growing in popularity. A unique diagnostic ultrasonography method called the Bedside Lung Ultrasonography in Emergency Department (BLUE-protocol) is designed to be used in conjunction with straightforward clinical data. It suggests a methodical study that can be completed in three minutes. 6 Therefore, the aim of the current study is o assess the lung ultrasound algorithm’s (BLUE protocol) diagnostic efficacy in intensive care unit (ICU) patients hospitalized with respiratory failure.
Patient And Methods
This randomized comparative study included 80 patients admitted to the ICU, Shebin El-Kom Teaching Hospital during three years from October 2017- October 2020.
Ethical consideration
The Kasr El-Einy Faculty of Medicine’s ethical committee approved the study at Cairo University. The parents or caregivers were asked for their signed informed consent, which was then obtained.
Inclusion criteria
Adult patients admitted with clinical and laboratory manifestations of ARF. A total of 80 patients with ARF were included in this study (e.g., interstitial lung disease, IPF, Acute pulmonary oedema, COPD exacerbation, pneumothorax, ARDS, etc.
Exclusion criteria
Age younger than 18 years, sever morbid obesity (BMI˃35 kg/m2) due to poor visualization of chest by US.
All patients included in the study subjected to the following
Methods of blindness
For the duration of data collection and analysis, members of the study group involved in gathering functional data were blinded to randomization. Ultrasound apparatus used: Wed-2018 Full-digital Ultrasound Diagnostic System, Probe selection: No one probe has been shown to be superior to another; instead, a single high-resolution micro-convex probe with a broad frequency range (3–5 MHz) can be employed. The patient was either sitting up straight, lying sideways, or both. The patient was lying flat for the duration of this post.
Upper anterior point
On the upper hand, this corresponds to the base of the middle and ring fingers. It is located above the top lobe. The middle of the palm of the lower hand is the lower anterior point (close to the nipple in a man). It is located above the lingular or middle lobe. The left heart will be missed by these points. Move as far posteriorly and laterally as you can from the lower anterior point to the posterior axillary line (limited by the bed). The bottom lobe is covered by it. By turning a curvilinear probe just enough to lie between the ribs (the cephalad will still be on the left of the picture), rib shadows can then be reduced.
Statistical Analysis
Microsoft Excel 2019 and SPSS v.25 for Microsoft Windows 10 were used to organize the results and perform statistical analysis. For quantitative data, the data were described using the mean (±) SD, and for qualitative data, frequency, and proportion. Chi-Squared (2) is a statistical method for comparing two groups or more about a single qualitative variable. P≤0.05 was regarded as a significant value.
Results
In this investigation, eighty patients were evaluated. The average BMI was 29.35±3.12 kg/m2, and the age was 57.35±13.30 years. 53 % of them were men, 47% were women, 15% had ischemic heart disease (IHD), 11% had chronic kidney disease (CKD), 9% had cerebrovascular stroke (CVS), 6% had an old stroke, 5% had atrial fibrillation (AF), 10% had COPD and asthma, and 66% had no significant medically significant behaviors. 26% of people smoked, as shown in Table (1).
Table 1: Demographic characteristics and co-morbidity of the studied patients (n=80).
| Variable | Studied patients (n = 80) | |
| No. | % | |
| Age
Mean ±SD Range |
57.35 ± 13.30 19 – 83 |
|
| BMI (kg/m2)
Mean ±SD Range |
29.35 ± 3.12 21 – 32 |
|
| Sex
Male Female |
42 38 |
53 47 |
| Special habit
No Smoker Ex-smoker Addict Smoker & Addict |
53 21 3 1 2 |
66 26 4 1 3 |
| DM
Yes No |
46 34 |
58 42 |
| HTN
Yes No |
41 39 |
51 49 |
| IHD
Yes No |
12 68 |
15 85 |
| CKD
Yes No |
9 71 |
11 89 |
| CVS
Yes No |
7 73 |
9 91 |
| Old stroke
Yes No |
5 75 |
6 94 |
| AF
Yes No |
4
76 |
5
95 |
The mean of CRP level, TLC count were 59.35 and 17.34 respectively. Diaphragmatic Excursion and Diaphragmatic thickness fraction were 6 cm and 32.1% respectively. Regarding ABG, the mean PH, PCo2, HCo3 and P/F ratio were 7.30, 49.7, 22.57 and 212.94, respectively. Also, sputum, urine and blood culture were positive in (33.8%, 13.8% and 8.8%, respectively), of the studied group 56.3% were on Invasive mechanical ventilation, as shown in Table (2).
Table 2: Laboratory investigations of the studied patients.
| Variable | Studied patients (n= 80) | |
| Mean ± SD | Range | |
| CRP | 59.35 ± 67.16 | 6 – 300 |
| TLC | 17.35 ± 7.1 | 6 – 39 |
| ABG
PH PCo2 HCo3 P/F ratio |
7.30 ± 0.13 49.7 ± 17.71 22.57 ± 6.01 212.94 ± 60.1 |
7.01 – 7.59 19 – 93 7- 38 90- 360 |
| Diaphragmatic parameters
Diaphragmatic Excursion (cm) Diaphragmatic thickness fraction % |
6 ± 1.77 32.1 ± 9.8 |
0.5 – 9 10- 72 |
| No. | % | |
| CRP
+ve -ve |
53 27 |
66 34 |
| Blood culture
+ve -ve |
7 73 |
8.8 91.3 |
| Sputum culture
+ve -ve |
27 53 |
33.8 66.3 |
| Urine culture
+ve -ve |
11 69 |
13.8 86.3 |
| Ventilatory support
Oxygen mask Nasal cannula Noninvasive CPAP Invasive MV |
11
17 7 45 |
13.8
21.3 8.8 56.3 |
In CXR finding32.5% of the studied group had normal lung, 18.8% had pneumonia and 20% showed pleural effusion of the studied group, also Heterogenous opacities has been detected in 10 %. Parapneumonic effusion has been dedicated in 3.8% ,6.3% had pulmonary edema and 6.3% showed pneumothorax and interstitial lung disease (ILD) detected in 2.5% of studied patients. Regarding CT chest findings 20% had normal lung, 27.5% had pneumonia and 23.8% showed pleural effusion, 6.3% showed pneumothorax. Interstitial syndrome detected in 11.3% of studied patients, as shown in Table (3).
Table 3: X-ray and CT chest findings of the studied patients.
Variable |
Studied patients (n = 80) | |
| No. | % | |
| Chest X- ray findings
Normal Lung Pneumothorax ILD Pulmonary Edema Pneumonia Pleural Effusion Parapneumonic Effusion Heterogenous opacities |
26 5 2 5 15 16 3 8 |
32.5 6.3 2.5 6.3 18.8 20 3.8 10 |
| CT chest findings
Normal Lung Pneumothorax Interstitial Syndrome Pulmonary edema Pneumonia Pulmonary Embolism Pleural Effusion Atelectasis |
16 5 9 3 22 4 19 2 |
20 6.3 11.3 3.8 27.5 5 23.8 2.5 |
Pneumothorax was presented by: Absent lung sliding & present lung point in all patients; Interstitial lung disease was presented by lung sliding & multiples B lines in (50%) patients. Pulmonary edema was presented by lung sliding & multiples B lines Pneumonia was presented by lung sliding & A lines &pneumonia in (39.1%) patients. Pleural effusion was presented by lung sliding& A lines &pleural effusion in (87.5%) patients. ARDS was presented by lung sliding & multiples B lines in all patients, as shown in Table (4).
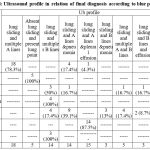 |
Table 4: Ultrasound profile in relation of final diagnosis according to blue protocol. |
The agreement of sonographic findings according to BLUE protocol and laboratory findings was found in 55 cases out of 80 cases (68.8%) where Kappa measure of agreement was moderate/substantial (K= 0.61). There was highly statistically significant difference between US and CT Finding .US detected all cases of pneumothorax that have been diagnosed by the CT, US detected 15 cases of pneumonia out 22 cases diagnosed by the CT chest, 5 cases out of 9 cases of interstitial lung disease. And 2 cases out of 3 cases of pulmonary edema and 15 cases out of 19 of pleural effusion, as shown in Table (5).
Table 5: Ultrasound diagnosis in relation of CT diagnosis as a gold standard test in the studied group.
| US diagnosis | CT diagnosis as a gold standard | Total | ||||||
| Normal lung | Pneum- othorax | Pneum-onia | Interstit- ial lung disease | Pulm- onary edema | Pleural effusion | Others | ||
| Normal lung
Pneumothorax Pneumonia Interstitial lung disease Pulmonary edema Pleural effusion Others |
13
0 1 1 1 0 0 |
0
5 0 0 0 0 0 |
5
0 15 0 0 0 2 |
1
0 1 5 0 1 1 |
0
0 1 0 2 0 0 |
1
0 3 0 0 15 0 |
0
0 2 0 0 0 0 |
23
5 23 6 4 16 3 |
| Total | 16 | 5 | 22 | 9 | 3 | 19 | 2 | 80 |
The sensitivity and specificity of US in diagnosis of pneumothorax were (100 %, 100%) respectively. Regarding pneumonia, sensitivity and specificity of US were (68.2%, 86.2%) respectively. Regarding ILD, sensitivity and specificity of US were (55.6%, 98.6%) respectively. As regard pulmonary edema and pleural effusion, US sensitivity and specificity were (66.7%, 97.4%) and (78.9%, 98.4%) respectively as shown in Table (6).
Table 6: Sensitivity, Specificity and Accuracy of US in diagnosing etiology of pleural effusion.
| Disease | Sensitivity
% |
Specificity
% |
PPV
% |
NPV
% |
Accuracy |
| Pneumothorax | 100% | 100% | 100% | 100% | 70% |
| Pneumonia | 68.2% | 86.2% | 65.2% | 87.72% | 81.3% |
| ILD | 55.6% | 98.6% | 83.3% | 94.6% | 83.8% |
| Pulmonary edema | 66.7% | 97.4% | 50% | 98.7% | 96.3% |
| Pleural effusion | 78.9% | 98.4% | 93.8% | 93.7% | 93.8% |
Discussion
In the study by Ali et al. it was discovered that 69% of the patients were men and 31% were women, and that the mean age of the participants was 49.2211.52 years. Additionally, 23% of people had hypertension, 13% had diabetes mellitus, 10% had heart disease, 5% had renal illness, and 2% had liver disease.7 These findings concur with our findings. While only 47% had concomitant conditions. Additionally, the mean age of the patients under study was . 52.5% of people were female and 47.5% were male. In 15% of patients, hypertensive pulmonary edema and iatrogenic PTX were the most common etiologies that led to respiratory symptoms, while pulmonary embolism and other systemic illnesses were least common (5% each). This runs counter to our findings.8
As US recognized every case of pneumothorax that the CT had identified in our investigation, there was a highly statistically significant difference between US and CT Findings. On the other hand, the US found 5 cases out of 9 cases of interstitial lung disease and 15 cases of pneumonia out of 22 cases identified by the CT chest. Additionally, pleural effusion occurs in 15 out of 19 instances and pulmonary edema in 2 out of 3 cases. Using a different meta-analysis, Winkler et al. discovered that the chest radiograph’s overall sensitivity and specificity were 49% (95% CI, 40-58%) and 92% (86-95%), respectively. This meta-analysis of seven trials found that lung ultrasonography had an overall sensitivity of 95% (92-96%) and specificity of 94%. According to the latest research, pleural effusion was diagnosed by US with a sensitivity and specificity of (78.9%, 98.4%) respectively.5 According to the current research, which was supported by Ali et al. lung ultrasounds had sensitivity, specificity, and diagnostic accuracy of 95.4%, 97.1%, and 96%, respectively, for pleural effusion. While chest X-rays’ sensitivity, specificity, and diagnostic precision in identifying pleural effusion were, respectively, 70.7%, 91.45%, and 78%.7 Furthermore, these results were comparable to those attained by El Mahalawy et al. who included 130 patients who were mechanically ventilated and those who were not and found that thoracic ultrasound had a sensitivity of 94% and a specificity of 96%, compared to CXR 70% sensitivity and 90% specificity.9 These findings corroborated those of Lichtenstein et al. who found that LUS had a sensitivity of 92%, specificity of 93%, and diagnostic accuracy of 93% for pleural effusion, compared to bedside CXR’s sensitivity, specificity, and accuracy of 47%, 39%, and 82%, respectively. 10 Further research indicated that CXR had worse diagnostic accuracy, sensitivity, and specificity than LUS in the diagnosis of pleural effusion, with values of 46 versus 100%, 90 versus 98%, and 76 versus 97%, respectively.8 The sensitivity and specificity of ultrasound for the diagnosis of pneumothorax were 100% in the current investigation. These findings are somewhat like those of Ali et al. who discovered that chest ultrasound had a sensitivity of 87.5%, specificity of 98.5%, and accuracy of 95% compared to CXR which had sensitivity, specificity, and accuracy of 53.1%, 98.5%, and 84% respectively in diagnosing pneumothorax.7 Also, our findings agree with Soldati et al. showed that (52%) of PTXs cases were revealed by Bedside chest radiography (CXR) with (sensitivity, 52%; specificity, 100%), whereas (92%) of PTXs were identified by LUS with one false-positive result (sensitivity, 92%; specificity, 99.4%).11 Bedside LUS has corresponding values of 75, 93, and 92%, while CXR has a sensitivity of 0%, specificity of 99%, and diagnostic accuracy of 89% for PTX.12 Additionally, numerous meta-analysis studies, produced results that matched those of our study. This study compares the use of CxR with lung ultrasonography (LUS) for the diagnosis of pneumothorax, with CXR having a sensitivity and specificity of 52% and 100%, respectively, and LUS having a sensitivity and specificity of 78.6% and 98.4%.13 according to Alrajab et al. 119 patients with chest injuries had a 53% sensitivity of chest ultrasonography to pneumothorax,14 in contrast to Hyacinthe et al. findings.15 In addition, because of chest ultrasound’s higher sensitivity than bedside chest X-rays (86.1% compared 52.7%), higher negative predictive values (96.8% versus 90.1%), and higher diagnostic accuracy (95.3% versus 90.6%), our results were superior to those of Abdalla et al. of 192 patients. However, compared to lung US, chest X-rays had slightly higher specificity (99.4%) and stronger positive predictive values (95.0% vs. 88.6%).16 Additionally, oblique CXR had a sensitivity and specificity of 61.4 and 99.2%, respectively, for detecting occult PTX. LUS has a 62.9 and 98.8% sensitivity and specificity, respectively.17 The high incidence of pneumothorax in mechanically ventilated patients, which is regarded as one of the most dangerous consequences of positive pressure ventilation, may be the cause of these discrepancies. 17
According to the current research, CXR had a sensitivity and specificity of (68.2%, 86.2%) when it came to detecting pneumonia, which is lower than that reported by Ali et al. discovered (89.3% vs 60.7%) and (97.7% compared 90.9%), respectively.7 These findings concur with those of Nazerian et al. who examined 285 patients and found that ultrasound had much greater sensitivity and specificity for detecting pneumonia than CXR (81% versus 64% and 94% versus 90%, respectively).18 Also, the current findings are less conclusive than those of Cortellaro et al. who reported that ultrasonography had significantly greater sensitivity and specificity than CXR (99% versus 67%) and (95% versus 85%), respectively, on 120 patients.19 On the other hand, Alkhayat and Alam Eldeen’s investigation of 62 patients revealed that (74%) of the time, chest ultrasonography was diagnostic.20 Because areas of consolidation may only be identified with the transthoracic ultrasound technique when they are attached to the pleural surface, this variation in accuracy may be explained by this. 9
The present findings indicated that the US had a sensitivity and specificity of (66.7%, 97.4%), respectively, for pulmonary edema. This is in line with Ali et al. findings, which showed that lung US provides a novel tool for pulmonary edema diagnosis at the bedside.7 Chest X-rays and chest ultrasound had higher sensitivity and specificity 88.9% and 98.9%, respectively than the latter. These findings corroborated with those of El Mahalawy et al. who reported that the sensitivity and specificity of chest ultrasound were 93% and 93%, respectively.9 Another study by Xirouchaki et al. found that chest ultrasonography had 94% sensitivity, 93% specificity, and 94% accuracy in identifying interstitial syndrome.12 Chest X-rays had a sensitivity, specificity, and accuracy of 46%, 80%, and 58% in detecting interstitial syndrome, respectively. These findings agreed with several investigations, including those by Agmy et al. who studied 109 patients and reported that the overall sensitivity and specificity of chest ultrasound were 93.2% and 100%, respectively,21 and Lichtenstein, who discovered that they ranged from 90% to 100%. The condition known as pulmonary edema, which can be either cardiogenic or non-cardiogenic and manifests as fluid buildup in the lung parenchyma and air gaps that impairs gas exchange, may be the reason for ICU admission or may arise suddenly in the ICU.22 Although heart failure is widespread, the prevalence of acute cardiogenic pulmonary edema is mostly unknown.23
Conclusion
In comparison with bedside CXR, LUS was found to be a more reliable, accurate, and sensitive bedside tool in diagnosing most of the common chest diseases encountered in critically ill patients. In comparison with CT scan, bedside LUS seems to be a valuable substitute in cases where performing CT is problematic. We recommend starting the use of bedside LUS as routine tool to improve the diagnostic accuracy for most of the pulmonary presentations.
Acknowledgement
We are grateful to all the participants in this study.
Conflicts of Interest
The authors report no potential conflict of interest.
Funding source
No funding has been received.
References
- Pairo-Castineira E, Clohisey S, Klaric L, Bretherick AD, Rawlik K, and Pasko D, Genetic mechanisms of critical illness in Covid-19. Nature, vol. 591, pp. 92-8, 2021.
CrossRef - Barman B, Parihar A, Kohli N, Agarwal A, Dwivedi DK, Kumari G. Impact of Bedside Combined Cardiopulmonary Ultrasound on Etiological Diagnosis and Treatment of Acute Respiratory Failure in Critically Ill Patients, Indian Journal of Critical Care Medicine: Peer- reviewed, Official Publication of Indian Society of Critical Care Medicine, vol. 24, pp. 1062, 2020.
CrossRef - Islam M, Levitus M, Eisen L, Shiloh AL, and Fein D, Lung ultrasound for the diagnosis and management of acute respiratory failure. Lung, vol. 198, pp. 1-3, 2020.
CrossRef - Smit JM, Raadsen R, Blans MJ, Petjak M, Van de Ven PM, Tuinman PR. Bedside ultrasound to detect central venous catheter misplacement and associated iatrogenic complications: a systematic review and meta-analysis. Critical Care, vol. 22, pp. 1-5, 2018.
CrossRef - Winkler MH, Touw HR, van de Ven PM, Twisk J, Tuinman PR. Diagnostic accuracy of chest radiograph, and when concomitantly studied lung ultrasound, in critically ill patients with respiratory symptoms: a systematic review and meta-analysis. Critical care medicine, vol. 46, pp. 707-14, 2018.
CrossRef - Xian J, Pei X, Lu W, Zhong H, Lin Y, Jin H, Su Z. The clinical value of bedside ultrasound in predicting the severity of coronavirus disease-19 (COVID-19) Annals of Translational Medicine, Vol. 9, pp. 336, 2021.
CrossRef - Ali NM, Maguid H, Gamil NM, Tawfeek MM, Hegab SS. Evaluation of the role of bedside lung ultrasound versus chest X-ray In Critically Ill Patients. Zagazig University Medical Journal, voi. 6, PP. 887, 2019.
CrossRef - Mohsen A, Samy W, El-Azizy H, Shehata MA. Lung ospective comparative study with bedside chest radiography using computed tomography of chest as a gold standard. Research and Opinion in Anesthesia and Intensive Care, voi. 2, PP.110, 2018
CrossRef - Elmahalawy II, Doha NM, Ebeid OM, Abdel-Hady MA, Saied O. Role of thoracic ultrasound in diagnosis of pulmonary and pleural diseases in critically ill patients. Egyptian Journal of Chest Diseases and Tuberculosis, vol. 2, PP.261, 2017.
CrossRef - Lichtenstein D, Goldstein I, Mourgeon E, Cluzel P, Grenier P, Rouby JJ. Comparative diagnostic performances of auscultation, chest radiography, and lung ultrasonography in acute respiratory distress syndrome. The Journal of the American Society of Anesthesiologists, vol. 1, PP.9-15, 2004.
CrossRef - Soldati G, Testa A, Sher S, Pignataro G, La Sala M, Silveri NG. Occult traumatic pneumothorax: diagnostic accuracy of lung ultrasonography in the emergency department. Chest. VOL. 133, PP.204-11, 2018.
CrossRef - Xirouchaki N, Magkanas E, Vaporidi K, Kondili E, Plataki M, Patrianakos A, Akoumianaki E, Georgopoulos D. Lung ultrasou and in critically ill patients: comparison with bedside chest radiography. Intensive Care Med, vol. 37, PP.1488-93, 2011.
CrossRef - Ding W, Shen Y, Yang J, He X, Zhang M. Diagnosis of pneumothorax by radiography and ultrasonography: a meta-analysis. Chest, vol. 140, PP. 859-66, 2011
CrossRef - Alrajab S, Youssef AM, Akkus NI, Caldito G. Pleural ultrasonography versus chest radiography for the diagnosis of pneumothorax: review of the literature and meta-analysis”, Critical Care, V0L. 17, PP.1-8, 2013.
CrossRef - Hyacinthe AC, Broux C, Francony G, Genty C, Bouzat P, Jacquot C, Albaladejo P, Ferretti GR, Bosson JL, Payen JF. Diagnostic accuracy of ultrasonography in the acute assessment of common thoracic lesions after trauma. Chest, vol. 141, PP.1177-83, 2012.
CrossRef - Abdalla W, Elgendy M, Abdelaziz AA, Ammar MA. Lung ultrasound versus chest radiography for the diagnosis of pneumothorax in critically ill patients: a prospective, single-blind study. Saudi Journal of Anaesthesia, voi. 10, PP.265, 2016.
CrossRef - Matsumoto S, Kishikawa M, Hayakawa K, Narumi A, Matsunami K, Kitano M. A method to detect occult pneumothorax with chest radiography. Annals of emergency medicine 57, PP.378-81, 2011.
CrossRef - Nazerian P, Volpicelli G, Vanni S, Gigli C, Betti L, Bartolucci M, Zanobetti M, Ermini FR, Iannello C, Grifoni S. Accuracy of lung ultrasound for the diagnosis of consolidations when compared to chest computed tomography. The American journal of emergency medicine, vol. 33, PP.620-5, 2015.
CrossRef - Cortellaro F, Colombo S, Coen D, Duca PG. Lung ultrasound is an accurate diagnostic tool for the diagnosis of pneumonia in the emergency department. Emergency medicine journal, vol. 29, PP.19-32, 2012.
CrossRef - Alkhayat KF, Alam-Eldeen MH. Value of chest ultrasound in diagnosis of community acquired pneumonia. Egyptian Journal of Chest Diseases and Tuberculosis, vol. 63, PP.1047-51, 2014.
CrossRef - Agmy GR, Hamed S, Saad MA, Ibrahim R, Mohamed AA. Assessment of severe dyspnea in critically ill patients by transthoracic sonography. Fayoum experience of the Bedside Lung Ultrasonography in Emergency protocol. Egyptian Journal of Bronchology, VOL. 12, PP.92-7, 2018.
- Lichtenstein DA. BLUE-protocol and FALLS-protocol: two applications of lung ultrasound in the critically ill. Chest, vol.147, pp.1659-70, 2015.
CrossRef







