Manuscript accepted on :17-01-2023
Published online on: 17-02-2023
Plagiarism Check: Yes
Reviewed by: Dr. Gandham Rajeev
Second Review by: Dr. Sushmita
Final Approval by: Dr. Patorn Piromchai
Mohammed Rashid Zghair Al-Notazy 1* , Haider Falih Shamikh Al-Saedi2
, Haider Falih Shamikh Al-Saedi2 , Mukhallad Abdul Kareem Ramadhan3
, Mukhallad Abdul Kareem Ramadhan3  and Ahmed Ghazi Hassan Al-Dalfi 4
and Ahmed Ghazi Hassan Al-Dalfi 4
1Department of Pharmacy, Al-Manara College of medical sciences, Misan, Iraq.
2Department of Pharmacology, University of Al-Ameed, Karbala, Iraq.
3Department of Pathology, College of Medicine, University of Misan, Misan, Iraq.
4Department of Clinical Pharmacy, Imam Al-Husein medical city, Karbla Directorate of health, Karbala, Iraq.
Corresponding Author E-mail: mohammedalnotazy@uomanara.edu.iq
DOI : https://dx.doi.org/10.13005/bpj/2627
Abstract
A growing body of literature recognizes the role of vitamin D deficiency in various health-related problems such as obesity, cardiovascular diseases, and dyslipidemia. Hence, we design a small non-blinded randomized clinical study to explore some of these effects. The primary outcome was to investigate whether supplementation with vitamin D could reduce body mass index (BMI), while the secondary outcome was to see its effects on blood pressure (BP), serum total cholesterol (TC), and HDL-cholesterol over 12 weeks period in overweight otherwise healthy individuals. Twenty-two subjects were randomized into two groups, group A was given vitamin D supplementation of 200 IU/day and group B was assigned to 2000 IU/day. A baseline assessment of body mass index (BMI), blood pressure (BP), serum total cholesterol (TC), and serum HDL-cholesterol was performed at baseline, 4, 8, and 12 weeks. Repeated measure ANOVA was used to determine the effect of supplements within subjects and between the groups of our study. The study was unable to demonstrate any statistically significant effects of these supplemental doses of vitamin D on both primary and secondary outcomes over the study period. The scope of this study was limited by a small sample size and a large randomized double-blinded clinical study could provide more definitive evidence.
Keywords
BMI; Blood Pressure; Cholesterol; HDL-Cholestrol; Vitamin D
Download this article as:| Copy the following to cite this article: Al-Notazy M. R. Z, Al-Saedi H. F. S, Ramadhan M. A. K, Al-Dalfi A. G. H. Effects of Vitamin D Supplementation on Healthy, Overweight, nd Obese Adults: A Non-Blinded, Randomized Trial. Biomed Pharmacol J 2023;16(1). |
| Copy the following to cite this URL: Al-Notazy M. R. Z, Al-Saedi H. F. S, Ramadhan M. A. K, Al-Dalfi A. G. H. Effects of Vitamin D Supplementation on Healthy, Overweight, nd Obese Adults: A Non-Blinded, Randomized Trial. Biomed Pharmacol J 2023;16(1). Available from: https://bit.ly/3KjMOnD |
Introduction
It has been commonly assumed that vitamin D plays a fundamental role in growth, development, and general health, especially for bone maintenance as well as calcium and phosphorus hemostasis. However, recent scientific research has shown the implications of vitamin D on multiorgan systems, and serum level fluctuations have been seen in a variety of diseases. Notable examples of these diseases are cardiovascular diseases, diabetes, dyslipidemia, and obesity 1,2,3.
According to the last update of WHO, obesity worldwide has increased 3-fold since 1975, and “In 2016, more than 1.9 billion adults, 18 years and older, were overweight. Of these over 650 million were obese” as well as “39 million children under the age of 5 were overweight or obese in 2020” 4. A large number of published papers have described the role of vitamin D on obesity and its complications such as alteration of blood pressure, serum lipid panel, and other cardiovascular and metabolic diseases. Early meta-analysis has identified that vitamin D deficiency prevalence was 24% more in overweight subjects in comparison to placebo (PR: 1.24; 95% CI: 1.14-1.34) 5. The above-mentioned study concluded that obese and overweight subjects are prone to vitamin D deficiency and its complications 5. This view is supported by a previous study that has seen the same findings on Asians and European-Americans 6. Another publication stated that patients could have lower body mass index (BMI) when they have desirable serum vitamin D levels and found the inverse relationship between blood pressure and serum vitamin D level 7. Other meta-analysis studies including 12 RCTs have identified that vitamin D would benefit blood pressure in elderly and vitamin D-deficient patients 8. Whereas, other meta-analysis research papers identified 11 cohort studies and 27 RCTs (43,320 and 3,810 participants respectively) that have not found such effects 9.
In the case of dyslipidemia, some literature has shown a beneficial effect on lipid panels in those who are supplemented with vitamin D in comparison to controls 10,11,12. In contrast to these findings, several studies have shown negative consequence sees of supplemental vitamin D on HDL 13,11,14. To date, there has been little agreement on the impacts of vitamin D supplementation on serum lipid profile.
According to the World Health Organization Iraq Office website, an estimated 30% of the population have high blood pressure levels and more than 30% suffer from obesity. Additionally, more than 25% of total deaths are attributed to cardiovascular diseases 15. In this study, we have tried to shed some light on the effect of two differant affordable supplements of vitamin D3 (200 IU and 2000 IU) on body mass index (BMI), blood pressure (systolic and diastolic), serum total cholesterol (TC) and High-density lipoprotein cholesterol (HDL-C) on Iraqi people since these parameters have been recognized by WHO Iraq Office Website as the area where the actions should be acted to improve the public health outcome.
Materials and methods
Participants.
This study was a non-blinded, randomized trial which has been designed to discover the prevention role of supplemental doses of vitamin D. It has been approved and registered by an ethical committee in Al-Manara college of medical sciences/Ministry of Higher Education and Scientific research/ /Iraq with registration No: 317 Date:30-05-2021.
Inclusion criteria
All participants gave written informed consent and appeared healthy, men were 13 (59%) and women were 9 (41%), aged (20-41) years old with a body mass index (BMI) range between 27.1 and 32.36 kg.m-2. A body mass index (BMI) above 25 kg.m-2 is classified as overweight, and over 30 kg.m-2 is considered obese.
Exclusion criteria
Individuals with any history of diabetes mellitus (DM), cardiovascular disease (CVD), malabsorption, renal disease, liver disease, difficulty in swallowing tablets or capsules, or who were taking medications or supplements (with or without vitamin D3 ) known to affect any dependent variable were excluded. Pregnant or lactating women and women who taking contraceptive medications were not included.
Study designs
After the interview, the subjects went to a screening visit. If the inclusion criteria were achieved, the next visit and baseline assessment were performed in the fasting state within 1 week. Heights, weights, and blood pressure were measured as well as fasting blood samples were drawn. At this visit, all subjects were given a daily supplement of vitamin D3 throughout the 12 weeks. The participants were given oral information and written recommendation on a healthy diet. The subjects were randomized into two groups, group A takes one tablet of vitamin D 200 IU per day, and group B on 200 IU per day. The laboratory staff or the investigators had no contact with the study participants, and neither knew the group status of the participants. Fasting blood samples were drawn and blood pressure and weights were measured after 0, 4, 8, and 12 weeks of the study (Figure 1).
 |
Figure 1: Study Design. |
Adverse events
Five adverse events were reported, four from participants in group B and one from group A. Three participants in group B reported nausea, and joint pain, however, the events spontaneously disappeared within 1-2 days and all three remained in the study. Tachycardia occurred in 2 subjects in group B and was excluded, and hypertension occurred in 1 subject in group A also excluded. None of them seem to be related to the study intervention.
Follow-up and measures
Anthropometric measurements at baseline 0, 4, 8, and 12 weeks were taken by trained staff at Almanara college of medical sciences/Iraq. Body weight was measured after an overnight fasting state without shoes and in minimal clothing using a digital scale (Rossmax BMI Body fat weighing scale WB220). Height was measured using a Seca tape measure (Seca, Hamburg, Germany). BMI was calculated by using MDCalc online Tools. Both systolic and diastolic blood pressure was measured with an automatic device at baseline (Rossmax CF155), and after every 4 weeks until the end of the study (12 weeks). The subjects were seated, rested for 5-10 min, and subsequently, two measurements of blood pressure were made at 2-min intervals in the morning and similarly two measurements in the evening. The mean value of the four measurements was used. Total cholesterol was measured using Free Cholesterol CHOD-POD Liquid (spinreact) and HDL- cholesterol was measured using HDL Cholesterol D Direct Enzymatic colorimetric (spinreact). All the work is performed according to the manufacturer’s protocol.
Outcome
We evaluated the effects of vitamin D supplementation on BMI as a primary outcome over 12 weeks. In addition, both systolic and diastolic blood pressure, total serum cholesterol, and HDL cholesterol were also evaluated as secondary outcomes.
Statistical Analysis
Repeated measure ANOVA was performed to analyze our data using IBM® SPSS® Statistics (Statistical Package for the Social Sciences) version: 28.0.1.1 (15). Vitamin D groups and time are independent variables (IV) whereas BMI, systolic and diastolic blood pressure, TC, and HDL are dependent variables (DV). A P-value of ≤ 0.05 is considered significant. Within-subjects analyses were performed to see the effects of time on dependent variables, while between-subjects tests were performed to see the effect of vitamin D doses on the dependent variables across all time points.
Ethics statements
This study was conducted according to the principles of the Declaration of Helsinki, and the study design and protocols were approved by the ethics committee of Al-Manara college of medical sciences/ Ministry of Higher Education and Scientific research/Iraq with registration No: 317 Date:30-05-2021. All subjects were informed about the aims and protocol of our study. All participants gave written informed consent before conducting the study. However, we did not use a therapeutic dose of vitamin D and 200 and 2000 IU are considered supplemental and can be given without prescription (OTC).
Results
Effect of two supplemental doses of vitamin D3 (200 IU and 2000 IU) on body mass index (BMI) at baseline, 4, 8, and 12 weeks of the study
The first aim of the current study is to investigate the impact of vitamin D supplementation on body mass index (BMI). Repeated measure ANOVA was conducted to see whether the body mass index of the subjects chosen would be affected by vitamin D3 supplements over 12 weeks of the study. Box’s test for equivalence of covariance matrices indicates the assumption of homogeneity of covariances was met with a p-value larger than 0.001 (p-value=0.102). Mauchly’s test of sphericity indicated the sphericity assumption was met (p-value=0.068). Hence, the multivariate test indicates that there were no statistically significant effects of vitamin D over time on BMI, Wilks’ Lambda tests were 0.871 F(3,18)=0.892, p-value=0.464, Partial Eta Square=12.9%. In addition, it could not be seen significant effects of combined vitamin D*time interaction, Wilks’ Lambda 0.847, F(3,18)=1.081, p-value=0.382, Partial Eta Square=15.3%. The pairwise comparison indicates that there was no obvious difference in BMI across all paired comparisons (p value>0.05) (Bonferroni adjusted paired t-test).
The test between subjects effects which means the main effects of grouping variables (200 IU and 2000 IU vitamin D) on BMI across all times has shown no statistically significant effects, F(1,20)=0.137, p-value=0.715, Partial Eta Square=7%. Finally, it could not be found any significant difference neither within the subject body mass indexes nor between groups of vitamin D3 supplementation over all the time points. Figure 2 shows the effects of vitamin D over time and on BMI.
 |
Figure 2: the bar chart shows the effects of two different doses of vitamin D on body mass index (kg/m2) over multiple time points. |
Effect of two supplemental doses of vitamin D3 (200 IU and 2000 IU) on systolic and diastolic blood pressure at baseline, 4, 8, and 12 weeks of the study
In the case of systolic blood pressure, repeated measure ANOVA was conducted and have shown that there were no significant effects of 2 supplemental doses of vitamin D on systolic blood pressure. Box’s test for equivalence of covariance matrices indicates the assumption of homogeneity of covariances was met with a p-value larger than 0.001 (p value=0.011). Mauchly’s test of sphericity indicated the sphericity assumption was not met (p value=0.001), however, it was adopted to evaluate the Greenhouse-Geisser and Huynh-Feldt (epsilon 0.413 and 0.448 respectively). Within-subject effects, the univariate repeated measure ANOVA with the Greenhouse-Geisser method of correction indicated there was no significant effect of time in both groups on systolic blood pressure, F(1.238, 24.766)=0.647, p value=0.461, Partial Eta Squre=0.03. In addition, this was not qualified by supplements*time interaction, Greenhouse Geisser F(1.238,24.766)=0.864, p-value=0.385, Partial Eta Square=0.041. The pairwise comparison indicates that there was no difference in systolic blood pressure across all paired comparisons (p value>0.05) (Bonferroni adjusted paired t-test).
Additionally, the test between subjects effects which means the main effects of grouping variables (200 IU and 2000 IU vitamin D) on systolic blood pressure across all times has shown no statistically significant effects, F(1,20)=2.244, p-value=0.150, Partial Eta Square=10.1%. Figure 3 shows the estimated marginal means of systolic blood pressure across the time points.
In the case of diastolic blood pressure, repeated measure ANOVA was also conducted and has shown that there were no significant effects of 2 supplemental doses of vitamin D on diastolic blood pressure. Box’s test for equivalence of covariance matrices indicates the assumption of homogeneity of covariances was met with a p-value larger than 0.001 (p-value=0.191). Mauchly’s test of sphericity indicated the sphericity assumption was met (p-value=0.731). Hence, the multivariante test indicates that there were no statistically significant effects of time on diastolic blood pressure, Wilks’ Lambda tests were 0.990 F(3,18)=0.060, p-value=0.980, Partial Eta Square=10%. However, it could be seen significant effects of combined vitamin D*time interaction Wilks’ Lambda 0.632, F(3,18)=3.489, p-value=0.037, Partial Eta Square=36.8%. The pairwise comparison indicates that there was no difference in diastolic blood pressure across all paired comparisons (p value>0.05) (Bonferroni adjusted paired t-test).
The test between subjects effects which means the main effects of 200 IU and 2000 IU vitamin D groups on diastolic blood pressure across all time has shown no statistically significant effects, F(1,20)=1.071, p-value=0.313, Partial Eta Square=5.1%. Figure 4 shows the effects of time and vitamin D on diastolic blood pressure.
In conclusion, A clear benefit of vitamin D on systolic and diastolic blood pressure could not be identified in this analysis.
 |
Figure 3: the bar chart shows the effects of two different doses of vitamin D on systolic blood pressure over multiple time points. |
 |
Figure 4: the bar chart shows the effects of two different doses of vitamin D on systolic blood pressure (mmHg) over multiple time points. |
Effect of two supplemental doses of vitamin D3 (200 IU and 2000 IU) on serum total cholesterol level at baseline, 4, 8, and 12 weeks of the study
Repeated measure ANOVA was also conducted to investigate whether the two doses of vitamin D have an effect on serum total cholesterol over 12 weeks period. It has shown that there were no significant effects. Box’s test for equivalence of covariance matrices indicates the assumption of homogeneity of covariances was met with a p-value larger than 0.001 (p value= 0.372911). Mauchly’s test of sphericity indicated the sphericity assumption was not met (p value= 0.001), however, it was adopted to evaluate the Greenhouse Geisser and Huynh Feldt (epsilon .641 and 0.743 respectively). Within-subject effects, the univariate repeated measure ANOVA with Greenhouse Geisser method of correction indicated there was no significant effect of time in both groups of the study on serum total cholesterol, F(1.924, 38.473)=1.616, p value=0.212, Partial Eta Squre=7.5%. In addition, this was not qualified by vitamin D3 group*time interaction, Greenhouse Geisser F(1.924, 38.473)=0.413, p-value=0.657, Partial Eta Square=2%. The pairwise comparison indicates that there was no difference in serum total cholesterol across all paired comparisons (p value>0.05) (Bonferroni adjusted paired t-test).
Additionally, the test between subjects effects which means the main effects of grouping variables (200 IU and 2000 IU vitamin D) on total cholesterol across all time has shown no statistically significant effects, F(1,20)=0.556, p-value=0.465, Partial Eta Square= 2.7%. Figure 5 shows the estimated marginal means of TC across the time points.
 |
Figure 5: the bar chart shows the effects of two different doses of vitamin D on serum total cholesterol (mg/dl) over multiple time points. |
Effect of two supplemental doses of vitamin D3 (200 IU and 2000 IU) on serum HDL-cholesterol level at baseline, 4, 8, and 12 weeks of the study
As described earlier, repeated measure ANOVA was also conducted to see any effects of vitamin D3 supplements on HDL-cholesterol over 12 weeks of study and we could not see any significant difference in serum HDL-cholesterol levels in both groups of vitamin D over the time of the study. Box’s test for equivalence of covariance matrices indicates the assumption of homogeneity of covariances was met with a p-value larger than 0.001 (p-value=0.551). Mauchly’s test of sphericity indicated the sphericity assumption was met (p-value=0.452). Hence, the multivariate test indicates that there were no statistically significant effects of vitamin D over time on HDL-cholesterol, Wilks’ Lambda tests were 0.863 F(3,18)=0.950, p-value=0.438, Partial Eta Square=12.8%. In addition, it could not be seen significant effects of combined vitamin D*time interaction, Wilks’ Lambda 0.872, F(3,18)=0.881, p-value=0.469, Partial Eta Square=36.8%. The pairwise comparison indicates that there was no difference in serum HDL-Cholestrol across all paired comparisons (p value>0.05) (Bonferroni adjusted paired t-test).
The test between-subjects effects of grouping variables (200 IU and 2000 IU vitamin D) on serum HDL-cholesterol across all times has shown no statistically significant effects, F(1,20)=1.100, p-value=0.307, Partial Eta Square=5.2%. Figure 6 shows the effects of vitamin D and time on serum HDL cholesterol.
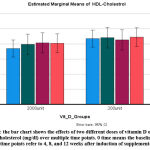 |
Figure 6: the bar chart shows the effects of two different doses of vitamin D on serum HDL-cholesterol (mg/dl) over multiple time points. |
Table 1: Relevant demographics of research participants
| Sample Characteristics | Number | Percentage |
|
Gender |
||
| Women | 9 | 40.90% |
| Men | 13 | 59.10% |
| Age Group | ||
| 18-29 | 14 | 63.60% |
| 30-39 | 6 | 27.3% |
| 40-50 | 2 | 9.1% |
| Incidence of Obesity | ||
| Overweight | 18 | 81.80% |
| Obese | 4 | 18.20% |
Table 2: Baseline characteristic of study participants
| Baseline | VIT_D_200 IU Group A | N=11 | VIT_D_2000 IU Group B | N=11 |
| Mean | SD | Mean | SD | |
| Age | 27.27 | 8.101 | 26.09 | 7.79 |
| BMI kg\m2 | 28.49 | 2.13 | 28.25 | 1.93 |
| BP (Systolic) | 115.91 | 13.103 | 123.91 | 12.15 |
| BP (Diastolic) | 74.09 | 10.719 | 81.45 | 8.66 |
| Cholesterol (mg/dl) | 173 | 30.29 | 187.45 | 28.79 |
| HDL (mg/dl) | 43.55 | 10.15 | 37 | 7.67 |
Table 3: Characteristics of study participants after 12 weeks of vitamin D supplements
| Vit_D_3 months | VIT_D_200 IU Group A | N=11 | VIT_D_2000 IU Group B | N=11 |
| Mean | SD | Mean | SD | |
| Age | 27.27 | 8.101 | 26.09 | 7.79 |
| BMI kg\m2 | 28.88 | 2.64 | 28.34 | 2.26 |
| BP (Systolic) | 108.64 | 33.09 | 123.45 | 10.54 |
| BP (Diastolic) | 75.36 | 6.313 | 79.09 | 9.803 |
| Cholesterol (mg/dl) | 177.27 | 33.45 | 185.18 | 30.64 |
| HDL (mg/dl) | 44.52 | 10.76 | 40.45 | 9.06 |
Discussion
Being overweight and obese have been considered risk factors for several chronic and metabolic diseases, including cardiovascular diseases and diabetes which are the leading causes of death worldwide. Many risk factors for overweight and obesity are preventable and modifiable 4. The association between vitamin D deficiency and body mass index is debatable. In 2018, a meta-analysis and systematic review of 55 observational studies were carried out and concluded that “the vitamin D deficiency could be associated with an increased BMI of both diabetic and non-diabetic subjects, however, they recommended more robust randomized, double-blinded future study to overcome the limitation of the observational studies 16. Our study could not detect any evidence of that effects at both 200 and 2000 IU on BMI across multiple time points.
Hypertension could be caused by being overweight and obese and is a major health burden and a fundamental risk factor for coronary artery disease, stroke, renal diseases, peripheral vascular diseases, etc 17. The previous literature investigated the role of vitamin D in many different doses on blood pressure and has observed inconsistent results on whether it has positive or negative consequences. It has been reported in a different experimental study that VDR (vitamin D receptor) deficiency is associated with increases in both systolic and diastolic blood pressure 18,19. A group of researchers investigated a total of 491 healthy subjects without any chronic diseases, ages 21 to 67 at baseline and followed up over 8 year period. Accordingly, they have concluded “vitamin D deficiency is a potential risk for blood pressure elevation and the development of hypertension” in an 8-year follow-up 20. Another clinical study has shown that vitamin D3 could affect both mean arterial pressure and systolic pressure but not diastolic one after 8 weeks of study 21. In contrast to the above findings, our study has been unable to identify a statistically significant effect of vitamin D (200 and 2000 IU tablets) on both systolic and diastolic blood pressure. Our set of results is consistent with those that have been seen by 22,23.
The results of previous research which examined the effects of vitamin D on serum lipids are conflicting. Positive effects have been reported in some of them 11,10. The debate about whether vitamin D has effects gained fresh prominence over decades. The two main meta-analysis studies have shown contradictory findings on lipid profiles. A meta-analysis of 12 randomized controlled trials (1346 participants) has indicated that “No statistically significant effects for vitamin D supplementation were observed for TC, HDL-C and TG (differences in means were 1.52 mg/dl (-1.42 to 4.46 mg/dl), -0.14 mg/dl (-0.99 to 0.71 mg/dl) and -1.92 mg/dl (-7.72 to 3.88 mg/dl) respectively)” 24. However, in 2019 meta-analysis of a total of 41 randomized control clinical trials (RCTs) comprising 3434 participants found a beneficial effect on total cholesterol, LDL-cholesterol, and triglyceride but no effects on HDL cholesterol 25. In our research, a clear benefit of supplemental doses of vitamin D (200 and 2000 IU tablets) on serum total cholesterol, and HDL-cholesterol could not be identified in this study.
Conclusion
The current research aimed to examine the effect of supplemental doses of vitamin D3 on BMI, blood pressure, serum total cholesterol, and HDL-cholesterol across multiple time points (0, 4, 8, and 12 weeks). The results of the current research have not detected statistically significant effects on the above-mentioned parameters.
Limitation
The scope of this research was limited in terms of sample size, study period, and exposure to sunlight. Further researches need to investigate in depth the effect of multiple doses of vitamin D3 on all cardiovascular risk parameter including subjects with metabolic syndrome with a large sample size in good design randomized, double-blinded, clinical trial. Finally, it can be said that our evidence was considered to be of mild to moderate quality depending on all the strengths and weaknesses of the study.
Acknowledgment
Special thanks to Al-Manara college for medical sciences and to the people who took part in the study as study subjects and investigators who did the laboratory assessment.
Conflict of Interest
There is no conflict of interest.
References
- Dobnig H, Pilz S, Scharnagl H, et al. Independent association of low serum 25-hydroxyvitamin d and 1,25-dihydroxyvitamin d levels with all-cause and cardiovascular mortality. Arch Intern Med. Jun 23 2008;168(12):1340-9. doi:10.1001/archinte.168.12.1340
CrossRef - Chonchol M, Scragg R. 25-Hydroxyvitamin D, insulin resistance, and kidney function in the Third National Health and Nutrition Examination Survey. Kidney Int. Jan 2007;71(2):134-9. doi:10.1038/sj.ki.5002002
CrossRef - Durup D, Jørgensen HL, Christensen J, et al. A Reverse J-Shaped Association Between Serum 25-Hydroxyvitamin D and Cardiovascular Disease Mortality: The CopD Study. J Clin Endocrinol Metab. Jun 2015;100(6):2339-46. doi:10.1210/jc.2014-4551
CrossRef - WHO. Overweight and obesity. 2021.
- Pereira-Santos M, Costa PR, Assis AM, Santos CA, Santos DB. Obesity and vitamin D deficiency: a systematic review and meta-analysis. Obes Rev. Apr 2015;16(4):341-9. doi:10.1111/obr.12239
CrossRef - Yao Y, Zhu L, He L, et al. A meta-analysis of the relationship between vitamin D deficiency and obesity. Int J Clin Exp Med. 2015;8(9):14977-84.
- Lin L, Zhang L, Li C, Gai Z, Li Y. Vitamin D and Vitamin D Receptor: New Insights in the Treatment of Hypertension. Curr Protein Pept Sci. 2019;20(10):984-995. doi:10.2174/1389203720666190807130504
CrossRef - Farapti F, Fadilla C, Yogiswara N, Adriani M. Effects of vitamin D supplementation on 25(OH)D concentrations and blood pressure in the elderly: a systematic review and meta-analysis. F1000Res. 2020;9:633. doi:10.12688/f1000research.24623.3
CrossRef - Zhang D, Cheng C, Wang Y, et al. Effect of Vitamin D on Blood Pressure and Hypertension in the General Population: An Update Meta-Analysis of Cohort Studies and Randomized Controlled Trials. Prev Chronic Dis. Jan 9 2020;17:E03. doi:10.5888/pcd17.190307
CrossRef - Qin XF, Zhao LS, Chen WR, Yin DW, Wang H. Effects of vitamin D on plasma lipid profiles in statin-treated patients with hypercholesterolemia: A randomized placebo-controlled trial. Clin Nutr. Apr 2015;34(2):201-6. doi:10.1016/j.clnu.2014.04.017
CrossRef - Muñoz-Aguirre P, Flores M, Macias N, Quezada AD, Denova-Gutiérrez E, Salmerón J. The effect of vitamin D supplementation on serum lipids in postmenopausal women with diabetes: A randomized controlled trial. Clin Nutr. Oct 2015;34(5):799-804. doi:10.1016/j.clnu.2014.10.002
CrossRef - Chai W, Cooney RV, Franke AA, Bostick RM. Effects of calcium and vitamin D supplementation on blood pressure and serum lipids and carotenoids: a randomized, double-blind, placebo-controlled, clinical trial. Ann Epidemiol. Sep 2013;23(9):564-70. doi:10.1016/j.annepidem.2013.07.003
CrossRef - Heikkinen AM, Tuppurainen MT, Niskanen L, Komulainen M, Penttilä I, Saarikoski S. Long-term vitamin D3 supplementation may have adverse effects on serum lipids during postmenopausal hormone replacement therapy. Eur J Endocrinol. Nov 1997;137(5):495-502. doi:10.1530/eje.0.1370495
CrossRef - Rajpathak SN, Xue X, Wassertheil-Smoller S, et al. Effect of 5 y of calcium plus vitamin D supplementation on change in circulating lipids: results from the Women’s Health Initiative. Am J Clin Nutr. Apr 2010;91(4):894-9. doi:10.3945/ajcn.2009.28579
CrossRef - WHO. WHO in Iraq.
CrossRef - Rafiq S, Jeppesen PB. Body Mass Index, Vitamin D, and Type 2 Diabetes: A Systematic Review and Meta-Analysis. Nutrients. Aug 28 2018;10(9)doi:10.3390/nu10091182
- Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. May 15 2018;71(19):e127-e248. doi:10.1016/j.jacc.2017.11.006
CrossRef - Andrukhova O, Slavic S, Zeitz U, et al. Vitamin D is a regulator of endothelial nitric oxide synthase and arterial stiffness in mice. Mol Endocrinol. Jan 2014;28(1):53-64. doi:10.1210/me.2013-1252
CrossRef - Jia J, Tao X, Tian Z, Liu J, Ye X, Zhan Y. Vitamin D receptor deficiency increases systolic blood pressure by upregulating the renin-angiotensin system and autophagy. Exp Ther Med. Apr 2022;23(4):314. doi:10.3892/etm.2022.11243
CrossRef - Karadeniz Y, Özpamuk-Karadeniz F, Ahbab S, Ataoğlu E, Can G. Vitamin D Deficiency Is a Potential Risk for Blood Pressure Elevation and the Development of Hypertension. Medicina (Kaunas). Nov 25 2021;57(12)doi:10.3390/medicina57121297
CrossRef - Panahi Y, Namazi S, Rostami-Yalmeh J, et al. Effect of Vitamin D Supplementation on the Regulation of Blood Pressure in Iranian Patients with Essential Hypertension: A Clinical Trial. Adv Exp Med Biol. 2021;1328:501-511. doi:10.1007/978-3-030-73234-9_35
CrossRef - Grundmann SM, Schutkowski A, Schreier B, et al. Vitamin D Receptor Deficiency Does Not Affect Blood Pressure and Heart Function. Front Physiol. 2019;10:1118. doi:10.3389/fphys.2019.01118
CrossRef - Wu L, Sun D. Effects of calcium plus vitamin D supplementation on blood pressure: a systematic review and meta-analysis of randomized controlled trials. J Hum Hypertens. Sep 2017;31(9):547-554. doi:10.1038/jhh.2017.12
CrossRef - Wang H, Xia N, Yang Y, Peng DQ. Influence of vitamin D supplementation on plasma lipid profiles: a meta-analysis of randomized controlled trials. Lipids Health Dis. Mar 20 2012;11:42. doi:10.1186/1476-511x-11-42
CrossRef - Dibaba DT. Effect of vitamin D supplementation on serum lipid profiles: a systematic review and meta-analysis. Nutr Rev. Dec 1 2019;77(12):890-902. doi:10.1093/nutrit/nuz037
CrossRef







