A.A. Mas Putrawati Triningrat1* , Ni Luh Made Novi Ratnasari1
, Ni Luh Made Novi Ratnasari1 , Made Paramita Wijayati1
, Made Paramita Wijayati1 , Ida Ayu Sri Indrayani2
, Ida Ayu Sri Indrayani2 , I Made Agus Kusumadjaja1 and Ariesanti Tri Handayani1
, I Made Agus Kusumadjaja1 and Ariesanti Tri Handayani1
1Opthalmology Department, Faculty of Medicine, Udayana University, Prof. Dr. IGNG Ngoerah Hospital, Denpasar.
2Neurology Department, Faculty of Medicine, Udayana University, Prof. Dr. IGNG Ngoerah Hospital, Denpasar.
Corresponding Author E-mail: masputra06@gmail.com
DOI : https://dx.doi.org/10.13005/bpj/2581
Abstract
Introduction: Cerebral toxoplasmosis is one of the opportunistic diseases that present in patients with HIV/AIDS. One of the rare symptoms is unilateral papilledema due to cerebral toxoplasmosis. Case report: A 26-year-old male patient came with complaints blurred vision for 2 months. The patient had a history of pouting lips, and weakness face, arm, and legs on the left side of the body. The patient has been diagnosed with the observation of space occupying lesion Cerebri in November 2020. Patient with HIV stage IV (WHO) infection and CD4 14 cells/uL and viral load 5.43 x 105 copies /mL. Visual acuity left eye 6/18 PH 6/12, contrast sensitivity examination in both eyes 1.65, and the results of FD-15 are within normal limits, but the results of perimetry was enlargement of blind spot, relative afferent pupillary defect in the left eye, with optic nerve head swelling in the left eye. An MRI showed the presence of intracerebral neurotoxoplasmosis. Discussion: Papilledema is the manifestation of optic nerve abnormality due to an increase in intracranial pressure. Cerebral toxoplasmosis leads to asymmetric target lesion present with ring enhancement image on MRI with contrast which causes SOL and manifests as papilledema. Bilateral papilledema is a hallmark of increasing cerebrospinal fluid pressure, but unilateral papilledema is a rare case with a 2% of prevalence among papilledema cases. Two proposed mechanisms of atypical papilledema were anatomical nerve sheath anomalies and unilateral axoplasmic blockage of the lamina cribrosa. Conclusion: Early diagnosis and appropriate treatment have a very important role in determining the prognosis of patients with cerebral toxoplasmosis.
Keywords
Cerebral Toxoplasmosis; HIV/AIDS; Unilateral Papilledema
Download this article as:| Copy the following to cite this article: Triningrat A. A. M. P, Ratnasari N. L. M. N, Wijayati M. P, Indrayani I. A. S, Kusumadjaja I. M. A. Unilateral Papilledema as a Rare Manifestation of Cerebral Neurotoxoplasmosis in HIV Patient: Case Report. Biomed Pharmacol J 2022;15(4). |
| Copy the following to cite this URL: Triningrat A. A. M. P, Ratnasari N. L. M. N, Wijayati M. P, Indrayani I. A. S, Kusumadjaja I. M. A. Unilateral Papilledema as a Rare Manifestation of Cerebral Neurotoxoplasmosis in HIV Patient: Case Report. Biomed Pharmacol J 2022;15(4). Available from: https://bit.ly/3gWKczB |
Introduction
Human Immunodeficiency Virus (HIV) is a type of retrovirus that infects the immune system through the destruction of CD4 lymphocyte cells and develops into acquired immunodeficiency syndrome (AIDS). According to the United Nations Program on HIV and AIDS (UNAIDS) in 2019, the prevalence of HIV in Southeast Asia is 3.8 million people/year, equivalent to 78% of the total infection cases. The prevalence in Indonesia shows that in 2019 there were 50,828 HIV cases, and Bali Province was in the 7th position with the highest number of HIV/AIDS cases.1 HIV patients are also often accompanied by opportunistic infections, one of which is cerebral toxoplasmosis with an incidence ranging from 35 to 80% of the total HIV cases.2
Toxoplasma gondii infection in humans can occur through the oral route, transplacental, blood transfusion, and through organ transplantation.3 Toxoplasma gondii in the form of tachyzoites can enter via the oral route to the reticuloendothelial system (RES). In the digestive tract, the cyst wall will be damaged by digestive enzymes and will release sporozoites. After from the intestine, the parasite will enter the systemic circulation and spread to various organs, especially the lymph, skeletal, central nervous system, placenta and retina.3,4
The manifestations of cerebral toxoplasmosis depend on the location and number of lesions. Damage to the CNS will give a typical picture in the form of multiple lesions with extensive necrosis necrotic area on radiology, as well as clinical symptoms such as headache (49-63%), fever (41-68%), focal deficits (22-80%), seizures (19 -29%), confusion (15-52%), ataxia (15-25%), lethargy (12-44%), cranial nerve weakness (12-19%), and visual disturbances (8-15%).5
The most common ocular symptoms of toxoplasmosis are blurred vision and decreased visual acuity, ocular pain, floaters, and photophobia may be present in some cases. HIV was found positive in tear, corneal, vitreous, and chorioretinal tissue samples with affected ocular structures including adnexa, anterior segment, posterior segment, and neuro-ophthalmic. Neurophthalmic manifestations occurring in 10% to 15% of HIV patients include papilledema, cranial nerve palsy, ocular motility disorders, and visual field defects.6 In immunocompetent patients, an activated immune reaction is able to envelop the tachyzoites into a dormant cyst form. However, in patients with immunocompromised conditions, a disordered immune system will cause more severe clinical symptoms, both in acute infection and due to reactivation of dormant cysts.3,4
Papilledema is the most common neuro-ophthalmic manifestation in optic nerve infections that occur in the optic nerve head caused by increasing intracranial pressure (ICP). Papilledema due to cerebral toxoplasmosis occurs due to the connection of the subarachnoid cavity in the brain with the optic nerve membrane. If there is an infection that causes an increase in ICP, this increase will be transmitted to the optic nerve so that there is a disturbance in axoplasmic transport.3,7 Optic disc edema usually manifests as hyperemia, dilatation, a gray appearance around the optic nerve, and telangiectasia of the disc surface capillaries. This also results in the appearance of flame hemorrhages around the disc. When disc edema and visual impairment are present, the differential diagnosis should include anterior ischemic optic neuropathy (AlON), papillitis, intraorbita compression, infection and CNS lesions.8
Case Description
A 26-year-old male patient came to the Prof. Dr. IGNG Ngoerah Hospital on January 29, 2021, with complaints of blurred vision in his left eye for two months ago. The blur in the left eye is said to be more blurred at the edges than in the center. The patient said the blurring occurred suddenly and persisted until now. Complaints of pain when glancing (-), severe pain in the head denied, intermittent headaches denied, history of nausea (-) vomiting (-). Other complaints such as red eyes (+), watery (+), and eye discharge (+) in the last 4 days ago. The eyes feel like a foreign body sensation (+), stinging (+), yellowish white, and sticky eye discharge comes out in the morning. The patient felt difficulty to open his eyes in the morning due to the discharge.
Patient has history of weakness in half of the body (+), pouting lips, and slurred speech for 2 months ago. Earlier, the patient was said to be able to stand on his own, but later when he was riding a motorcycle, the patient fell due to weakness in the left half of his body. The patient was treated in the Wijaya Kusuma Room at Sanglah Hospital with obs Space occupying lesion (SOL) cerebral et causa suspect cerebral abscess dd tumor dd vascular process in November 2020. While being treated the patient received Ultravist therapy 1 x 1 (IV), Acetylcysteine 3 x 200 mg, Pyrimethamine 1 x 25 mg, Clindamycin 1 x 150 mg, Dexamethasone 4 x 10 mg (I.V), Omeprazole 2 x 40 mg (I.V), Paracetamol 3 x 1000 mg (I.O), Micafungin 1 x 50 mg (IV). During the treatment, the patient admitted that his left eyelid could not close completely during sleep. After that, the patient’s left eye began to watery and discharge dirt, and the patient just realized that the left eye(LE) was blurrier than the right eye(RE).
History of chronic diseases such as diabetes mellitus and hypertension were denied. History of being diagnosed with HIV 3 months ago (+) with CD4: 14 cells/mm3 and viral load 5.43 x 105 copies/mL (30 November 2021). After being diagnosed, the patient then received treatment with Highly Active Antiretroviral Therapy (HAART), such as Fix drugs combination (FDC) 1 x 1 consisting of Lamivudine 150 mg, Tenofovir 300 mg, and Evafirenz 600 mg. The patient has also been diagnosed with condyloma acuminata and treated with 80% Trichloracetic acid (TCA) solution every week and 20 mg zinc tablets every 4.5 hours. The patient has a history of changing partners before being diagnosed with HIV stage IV. Denied history of using drugs, history of glasses (-), eye surgery (-), allergies (-), and history of suffering from COVID-19 was denied.
Patient control to the ophthalmology polyclinic and the visual acuity (VA) OS 6/18 pinhole (PH) 6/12 while VA RE 6/12 PH 6/6. The intraocular pressure was found to be within normal limits (RE 16 mmHg and LE 12 mmHg). Examination of the anterior segment of the eye found positive conjunctival vascular injection (CVI) in both eyes, secret (+), positive direct pupillary reflex in both eyes, positive indirect pupillary reflex in both eyes, and positive Rapid Afferent Pupillary Defect (RAPD) in LE. Funduscopy showed LE optic nerve head is round, blurred, cup disc ratio (CDR) is difficult to evaluate, arterial to the venous ratio (aa/vv) is 2/3, the retina is good, and macular reflex is positive. Meanwhile, funduscopy of RE revealed well-defined optic nerve head, hyperemia, CDR 0.3, aa/vv 2/3 good retina, and positive macular reflex.
Schirmer I test, obtained 7 mm RE and 9 mm LE, examination of tears breaks up time (TBUT) in the right eye for 4 seconds and the left eye for 6 seconds. Contrast sensitivity examination in both eyes did not find decreasing in contrast sensitivity (RLE 1.65), Ishihara in both Eyes within normal limit, and the results of the Farnsworth D-15 test (FD-15) were within normal limits. The examination was then followed by evaluation of the posterior segment, Humfrey Visual Field (HVF) test, and Optical Coherent Tomography (OCT).
The posterior segment of the patient’s LE showed round optic nerve head, blurred boundaries, difficult to evaluate Cup Disc Ratio (CDR), bulging (+), good retina, good macular reflex (+). The results of the HVF examination revealed an enlargement of the blind spot in the patient’s LE (Figure 1). Optical coherence tomography (OCT) for retinal nerve fiber layer (RNFL) showed swelling in all quadrants of the LE (Figure 2).
 |
Figure 2. (A) Fundus photo on 1/2/2021 showing well-defined rounded OD of papillary nerve II, CDR 0.3, a/v 2/3 retina good, |
Laboratory investigations showed non- reactive anti-toxoplasma IgM: 0.09 IU/mL, anti-toxoplasma reactive with IgG > 300 IU/mL, LED 53.9 mm/hour, WBC 5.04 10³/UL, HB: 12.73 g/dL, PLT: 213,50 10³/ L, SGOT 75,2 U/L, SGPT: 118,70 U/L, GDS: 87 mg/dL, Lymphocytes: 1.70 103/µL; CD4: 14 cells/uL, HIV RNA: 5.43 x 105 copies/mL, HBsAg: No-reactive, Anti-HCV: non-reactive. The patient was diagnosed with LE optic disc swelling ec optic neuritis dd papilledema ec suspected intracranial process dd infection; RLE conjunctivitis ec susp bacteria dd virus + dry eye disease; Cerebral neurotoxoplasmosis; HIV on HAART. The patient received warm compress therapy, xitrol ed 6 x1 RLE, Lyteers ed 6 x 1 RLE, Oculenta eo 1 x 1.
On 2nd February 2021 patient was planned for Magnetic Resonance Imaging (MRI) examination of the orbital focus head with contrast T1T2 weighted fat suppression.
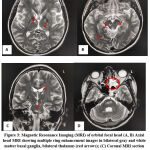
Magnetic Resonance Imaging of the head on 4th February 2021 and based on the results of MRI of the orbital focus, a ring enhancement image was obtained which suggested neurotoxoplasmosis in the gray and white matter of bilateral fronto- parieto-temporal lobes, bilateral basal ganglia, bilateral thalamus, bilateral caudate nucleus, right midbrain, bilateral pons and cerebellar hemispheres; Left sphenoid dilatant pneumosinus extending to the left orbital apex that appears to cause mild compression of the left optic nerve sheath; Bilateral oculi, bilateral optic nerves, and bilateral extraocular muscles showed no abnormalities; Bilateral maxillary, sphenoid and left ethmoid sinusitis; Deviation of the nasal septum to the left (Figure 3).
The patient returned for control on 16th February, 2021, and after the results of the head MRI was obtained, the patient was decided for observation, controlled every 2 months to monitor the development of visual acuity, color, contrast sensitivity, and the patient’s field of view. Neurology department gave therapy with Pyrimethamine 2 x 25 mg and Clindamycin 4 x 300 mg (tapering off).
The next follow-up on April 19, 2021, the patient’s visual function was re-evaluated comprehensively. The patient showed significant improvement in visual acuity and could be corrected. RE vision was 6/9 PH 6/6 (S-0.50 6/6), LE 6/9 PH 6/6 (S-0.50 6/6).
RLE contrast sensitivity of 1.65, evaluation of color vision with Ishihara obtained RLE 25 plates, FD-15 RLE within normal limits, the anterior segment of RLE did not find any ocular signs of toxoplasmosis. Evaluation of the posterior segment found clear vitreous, right eye fundus showing well-defined optic nerve head, CDR 0.3, aa/vv 2/3 retina good, RM (+). Meanwhile, for the fundus LE, the optic nerve head was still round with blurred boundaries, hyperemia, low CDR, good retina, and RM (+). No active lesions or Toxoplasma scars were found in the retina RLE. Evaluation of the visual field with HFV found that there was still an enlargement of the blind spot in the LE which in subsequent controls got better (Figure 4).
The patient continued his treatment i Neurology polyclinic and VCT for neurotoxoplasmosis and HIV therapy. Treatment from the neurologist was continued with Pyrimethamine 1 x 25 mg, Clindamycin 2 x 300 mg, and Mecobalamin 3 x 500 mg with consideration of clinical and neurological improvement in the patient. Antiretroviral therapy from VCT was continued with the formulation of fixed drugs formula 1 x 1 (Tenofovir 300 mg + Lamivudine 150 mg + Efavirenz 600 mg) and prophylaxis with Cotrimoxazole 1 x 960 mg. CD4 and clinical monitoring continued during subsequent follow- ups.
There are improvements in visual acuity, visual field, and posterior segment in the next follow-up on 16th June, 2021. Right eye VA was 6/9 PH 6/6 (S-0.50 6/6), the VA of the LE 6/ 9 PH 6/6 (S-0.50 6/6). Contrast sensitivity of RLE was 1.65, evaluation of color vision with Ishihara obtained RLE 25 plates, FD-15 RLE within normal limits, anterior segment RLE within normal limits, fundus RE round optic nerve head with clear margins CDR0.3, aa/vv 2/3 retina good, macula RM (+) as well as on funduscopy LE where optic nerve head is well demarcated with CDR that can be assessed. Evaluation visual field is also still being done to evaluate the patient’s visual function.
Laboratory examination on the patient showed CD4: 121.2 cells/uL, CD8: 1,721.4 cell/ uL, HIV viral load: undetectable per mL of blood. Patients were planned for observation from the ophthalmology clinic and continued treatment at VCT and Neurology Poly for tapering off Clindamycin and Pyrimethamine.
 |
Figure 5: Fundus photo on 16/6/2021 shows a well-defined optic nerve papilla in the left eye. (Courtesy of Novi, 2021). |
Discussion
Papilledema is one of the manifestations of various spectrum diseases of the optic nerve, including anterior ischemic optic neuropathy, non- arthritic ischemic optic neuropathy, and neoplasms (meningioma, optic nerve glioma). Ischemic neuropathy and optic neuritis are the most common differential diagnoses of unilateral papilledema in young adults <50 years old.
This case reports a fairly rare manifestation of unilateral papilledema in a 26-year-old male patient with a history of HIV/AIDS. A decrease in the patient’s VA and visual field is one of the manifestations of an increase in intracranial pressure (ICP) due to intracerebral Toxoplasmosis infection.
The most common manifestation of Toxoplasmosis in the eye is toxoplasma chorioretinitis, while optic neuritis due to toxoplasma without retinitis is quite rare. Toxoplasma gondii is an obligate intracellular parasite that is widely distributed throughout the world. In Indonesia, the prevalence of T. gondii seropositive in humans ranges from 2% to 63%.5 This parasite causes asymptomatic persistent chronic infection in immunocompetent individuals, but in immunocompromised individuals, reactivation will occur, causing clinical symptoms.5
Cerebral toxoplasmosis is an opportunistic infection of the central nervous system that is most often found in HIV/AIDS patients, especially in HIV/AIDS patients with low CD4 cells. In patients with HIV infection, Toxoplasma gondii causes severe opportunistic infections that require appropriate management.5,9
A study by Anuradha and Preethi in India showed that the seropositive T. gondii among HIV patients was 34.78%.9 This study is also supported by Meisheri et al., which showed that 67.8% of clinical manifestations of toxoplasmosis occurred in patients with HIV/AIDS compared to 30.9% of immunocompetent persons.10
The presence of toxoplasma infection in the central nervous system (CNS) produces multifocal lesions with a predilection for sites in the basal ganglia, frontal, parietal, and occipital lobes. Patients generally will complain of headaches, the appearance of focal neurologic deficits, seizures, changes in mental status, and fever. While the clinical symptoms of neuro ophthalmology usually appear to include homonymous hemianopsia, quadranopsia, and muscle paresis of eye movements.11
Physiologically, the optic nerve originates from the ganglion cell layer on the retinal surface to the optic chiasm. The optic nerve consists of axons of retinal ganglion cells and glial cells. The number of axons tends to be fixed, while the number of glial cells and myelin is relatively variable in various places compared to axons. Anatomically, the optic nerve is divided into four parts:12
1) The intraocular region (optic nerve head) is about 1.0 – 1.02 mm long with a transverse diameter of 1.5 mm to the sclera. The optic nerve fibers in the optic disc are divided into four layers: the superficial nerve fiber layer, the prelaminar area, the laminar area, and the retrolaminar area.
2) The intraorbital region starts from the posterior surface of the sclera and has a length of about 30-40 mm and a diameter of 3 mm due to the addition of the myelin sheath starting from the retrolaminar. Intraorbita region nerve fibers are the longest part of the entire optic nerve, with a slightly tortuous shape like the letter “S”. About 8-15 mm behind the eyeball, the central retinal artery penetrates into the optic nerve.
3) Intracanalicular region is the region of the optic nerve in the optic canal which is part of the alla minor (lesser wing) of the sphenoid bone. Has a length of about 8 – 10 mm and is tightly fixed in the optic canal.
4) Intracranial region, the optic nerve leaves the optic canal at a distance of 1 mm in the medial cranial fossa as the optic nerve in the intracranial region. The length of the intracranial optic nerve fibers is ±10-16 mm. The nerve fibers of this region run superior to the ophthalmic artery and superomedial to the internal carotid artery. Because it is part of the CNS, the interorbital portion of the optic nerve is also covered by the pia mater, arachnoid, and dura mater.
The most susceptible region was the canalicular regio. It could be compressed by trauma mechanism due to anatomical abnormalities of the orbital bones. The optic canal is a canal composed by Alla minor (lesser wing) of the sphenoid bone and optic nerve, along with the ophthalmic artery running through this canal. The dilatation of the sphenoid sinus will cause pressure on the intracanalicular region of the optic nerve.12
Papilledema is the most common neuro-ophthalmic manifestation in optic nerve disorders that occur in the optic nerve head due to increased ICP. Papilledema that occurs bilaterally is a typical sign of increased intracranial pressure either due to the effect of space pressure or increased cerebrospinal fluid (CSF). Unilateral papilledema is a rare condition. According to Chang et al. (2017), the prevalence of true unilateral papilledema is only around 2% of all papilledema cases, with the highest cause due to malignancy or idiopathic intracranial hypertension (IIH).13
Two hypotheses of the mechanism of developing unilateral papilledema are 1) The presence of abnormalities of the optic nerve sheath, either congenital or acquired, which results in inhibition of the transmission of CSF pressure to the optic nerve; 2) Abnormalities in the venous sinuses and differential unilateral axoplasmic block that decrease the transmission of increased intracranial pressure to the scleral canal of the optic nerve.13,14
The degree of papilledema based on the American Academy of Ophthalmology (2019) is divided according to the Frisen classification into five grades. Grade 0 optical disk normal, CDR normal; grade I blurring of the optic disc margin, the indistinct border with a grayish halo around it, grade II increased nasal border of the optic disc, blurring of the entire temporal margin with a 360º gray halo, grade III increased temporal border of the optic disc, obscurations of the optic disc major vessels, finger-like extensions radiating from the halo; grade IV elevation of the entire ONH margin, flat appearance without cup concavity, total obscuration of central retinal arteries and veins; grade V dome-shaped protrusion from ONH.11
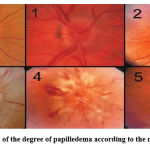 |
Figure 6: Classification of the degree of papilledema according to the modified Frisen scale.11 |
A typical feature of cerebral toxoplasmosis is the presence of an asymmetric target sign.15 In this patient, papilledema resulted from multiple ring enhancement lesions in bilateral fronto-parieto-temporal lobes, bilateral basal ganglia, bilateral thalamus, and bilateral caudate nuclei, causing bilateral perifocal edema and causing space-occupying effects in the brain parenchyma. This causes an increase in intracranial pressure, which is transmitted to the optic nerve via CSF flow in the subarachnoid space which is also connected to the sheath with the optic nerve.
The optic nerve in the intracanalicular region is the most crucial location for obstruction of CSF flow in the subarachnoid space of the optic nerve, which can cause a “bottleneck effect” on the opening of the optic canal in the intraorbita region, which is smaller in some cases than in normal people. The dura mater of the optic canal fuses with the periosteum of Os. The sphenoid produces a static portion. In contrast, the more dynamic part covers the pia mater and arachnoid layers.16
In this patient, unilateral papilledema in the left eye was caused by the presence of perifocal edema of the mesencephalon and basal ganglia, which caused intracranial space-occupying effects and increased intracranial pressure. The increase in intracranial pressure will be transmitted through the CSF flow in the optic nerve subarachnoid space. A left sphenoid dilatation pneumosinus in this patient gave compression to the left intraorbital region. The opening of the left intraorbital optic canal is smaller than the lumens of the other optic canals. This results in a “bottleneck effect” on CSF flow in the subarachnoid space of the left optic nerve and results in the manifestation of grade III Frisen’s papilledema in the left optic disc.
Unilateral papilledema in this patient is an early manifestation of increased intracranial pressure due to cerebral neurotoxoplasmosis. If not treated properly will cause bilateral asymmetric papilledema in conditions of advanced intracranial pressure elevation. Sinus venous abnormalities due to left sphenoid dilatation pneumosinus also cause axoplasmic stasis to the optic nerve scleral canal and contribute to the development of left papilledema.
The management of this patient follows the treatment of toxoplasma cerebri from the neurology section and the procedure for treating toxoplasmosis in the 2019 National Guidelines for Medical Services in HIV/AIDS patients. This patient was first identified with a CD4 count of 14 cells/uL. CD4 count < 200 cells/uL in HIV/AIDS patients increases the risk of developing CNS neurotoxoplasmosis due to reactivation of chronic infections.15 The management of cerebral toxoplasmosis is still using a combination of pyrimethamine loading dose 1 x 200 mg and clindamycin 4 x 600 mg. After administering the combination of the two antimicrobials, the evaluation will be carried out two weeks after the administration of clindamycin and pyrimethamine. Both neurological clinical evaluation and CT scan were carried out to monitor disease progression.2 Tapering off the dose of clindamycin and pyrimethamine was carried out based on clinical neurological monitoring in stages.
The 2019 National Guidelines for Medical Services in HIV/AIDS patients also recommends prophylaxis with Co-trimoxazole 1 x 960 mg in HIV/AIDS patients with CD4 < 100 cells/uL. Antiretroviral therapy can be started 2-3 weeks after diagnosis. This patient has received therapy according to PNPK with ARV FDC 1 x 1 and cotrimoxazole prophylaxis. Prophylactic administration can be discontinued in adult patients who have received ARVs and CD4 cells > 200 cells/uL for three consecutive months. Clindamycin and pyrimethamine can be given up to 6 months after ARV administration.15
Management of unilateral papilledema in this patient was carried out with close observation for the first one month, followed by periodic observations every two months to show functional and anatomical improvement. In the 4th month, the patient had shown a significant improvement in VA (6/9 PH 6/6) RLE, improved contrast sensitivity, and HVF in the left eye, which no longer showed an enlargement of the blind spot. The anatomical improvement showed the reduction of papilledema, well defined demarcation, CDR and the disappearance of papillary hyperemia in the 4th month of follow-up.
The clinical improvement in the ophthalmology department will provide input for the neurology department in seeking clinical improvement and periodic tapering off of Toxoplasmosis therapy. The management of cases of papilledema due to Toxoplasmosis cerebri requires multidisciplinary collaboration from the Neuro-ophthalmology, Neurology, and Tropical Infections Department to maximize the therapeutic outcome for the patient.
Conclusion
Cerebral toxoplasmosis is one of the opportunistic infections that occur in patients with HIV/AIDS. The manifestations of increased intracranial pressure can be in the form of bilateral or unilateral papilledema. Papilledema of the optic nerve indicates axoplasmic stasis caused by increased intracranial pressure. Appropriate and immediate treatment is needed to prevent chronic papilledema and papilledema to avoid permanent complications. Appropriate multidisciplinary diagnosis and management will prevent permanent optic nerve complications, which will determine the patient’s prognosis for both intracerebral improvement and vision and visual field.
Acknowledgement
The authors would like to thank Udayana University, Sanglah General Hospital, and the patients which has helped a lot during this research.
Author Contribution
All authors have equal contributions in the manuscript.
Conflict of Interest
The authors declare no conflict of interest.
Funding Sources
there is Funding Sources
References
- Kemenkes RI. General situation of HIV/AIDS and HIV test. Pusat Data dan Informasi Kementrian Kesehatan RI. 2018. p. 1–12.
- Sanni Hassana D, Hadisaputro S, Sofro MAU. Toxoplasmosis and Cerebral Toxoplasmosis in HIV/AIDS Patients in Kariadi Hospital, Semarang. J Epidemiol Kesehat Komunitas. 2021;6(1):213–7.
CrossRef - Indrayani IA. Uji Validitas Kadar CD4 untuk Diagnosis Toksoplasmosis Serebri pada Penderita Acquired Immunodeficiency Syndrome. Universitas Udayana; 2011.
- Sugianto P. Infeksi Toksoplasma pada Sistem Saraf. In: Continuing Neurology Education. Malang: Danar Wijaya Brawijaya University Press; 2014.
- Yostila D, Armen A. Toxoplasmosis Cerebri Pada HIV AIDS. J Kesehat Andalas. 2018;7(Supplement 4):96–9.
CrossRef - Kaberi B., Jim W. Ocular Manifestations of HIV. In: NCBI Bookshelf. 2021.
- Indraswati E, Suhartono G. Sindrom Foster Kennedy. Oftalmoogi Indones. 2008;6:92–3.
- Alipanahi, R. S. Acute Papillitis in Young Female with Toxoplasmosis. Middle East African J Ophtalmol. 2011;18(3):249–51.
CrossRef - Anuradha B, C P. Seroprevalence of toxoplasma IgG antibodies in HIV positive patients in and around Khammam, Telangana State. J Clin Diagn Res; 2014;8:101–12.
CrossRef - Meisheri YV, Mehta S, Patel U. A prospective study of seroprevalence of toxoplasmosis in general population, and in HIV/AIDS patients in Bombay, India. J Postgr Med. 2007;43:93–7.
- Ophtalmology AA of. HIV Ocular Manifestation. AAOBCSC. 2020;5:334–5.
- Brar VS, Law, S K, Lindsey JL. Basic and Clinical Science Course : Fundamentals and Principles of Ophthalmology. Section 2. In: American Academy of Ophthalmology. San Fransisco: European Board of Ophthalmology Subcommittee; 2021. p. 144–82.
- Chang T, Alibhoy A. Unilateral papiloedema. Pr Neurol. 2017;17:310–1.
CrossRef - Elnahry AG. Unilateral papilledema revealing an intracanalicular optic nerve sheath meningioma. Neuro-opthalmology. 2018;18(3):1–5.
- Pedoman Nasional Pelayanan Kedokteran Tatalaksana HIV. Keputusan Menteri Kesehatan Republik Indonesia Np HK.01.07/ Menkes/ 90/ 2019. Jakarta: Kementrian Kesehatan Republik Indonesia.; 2019.
- Pircher A, Montali M, Berbera J, Remonda L, Killer HE. No The Optic Canal : The Bottleneck for Cerebrospinal Fluid Dynamics in Normal Tension Glaucoma. Front Neurol. 2017;8(47):1–7.
CrossRef