Santosh Kumar Sahu1* , Nihar Ranjan Mishra1
, Nihar Ranjan Mishra1 , Sisir Kumar Sahoo1
, Sisir Kumar Sahoo1 , Binod Chandra Raulo1
, Binod Chandra Raulo1 and Dattatreya Kar2
and Dattatreya Kar2
1Department of Orthopedic, IMS and SUM Hospital, Siksha O Anusandhan (Deemed to be) University, K8 Lane 1, Kalinganagar, Bhubaneswar, Odisha, India.
2Department of Medical Research, Health Science, IMS and SUM Hospital, Siksha O Anusandhan (Deemed to be) University, Bhubaneswar, Odisha, India.
Corresponding Author E-mail: drsksims@gmail.com
DOI : https://dx.doi.org/10.13005/bpj/2565
Abstract
Pain is believed to be a poorly understood phenomenon, which is mostly regulated by neural, cellular, hormonal & emotional components. Epidural analgesia is used for pain relief in patients undergoing primary total knee arthroplasty, though provides good pain control, many a time is associated with side effects such as hypotension, urinary retention and impaired mobility. The purpose of the current study is to compare the efficacy of ACB to local infiltration of analgesics by Intraarticular Epidural Catheter for primary total knee arthroplasty by comparing visual analog scale, knee flexion, and active SLRT on the day of surgery (POD-0), POD1-3, day of discharge, and 4 weeks after surgery. This study is prospectively randomized, the cases undergoing primary knee replacement were divided into two groups, which includes a minimum of 36 cases in each group.Group-1(36) patients received local infiltration of analgesics via IAECand Group-2(36) patients received single shot ACB. As far as age, sex, BMI(kg/m2), pre-op VAS, mean pre-op flexion, mean pre-operative varus, mean pre-op KSS(Knee society score), duration of surgery and hospital stay is concerned no significant difference was noticed between the two groups.Group-1(LIA via IAEC) had significantly lower VAS on a postoperative day (POD) 1-3, lower tramadol consumption, better ROM (atPOD1-3), superior quadriceps recovery(active SLRT), earlier mobilization day, better KSS (at 4weeks) postoperatively, compared to Group-2(single shot ACB).LIAby IAEC for patients undergoing primary TKA is a better option compared to single shot ACB concerning to pain levels, narcotic usage, range of motion, quadriceps recovery and KSS (Knee society score).
Keywords
Adductor canal block; Epidural catheter; Intraarticular; Knee Arthroplasty; Local infiltration of analgesic
Download this article as:| Copy the following to cite this article: Sahu S. K, Mishra N. R, Sahoo S. K, Raulo B. C, Kar D. Efficacy of Local Infiltration of Analgesics via Intra-articular Epidural Catheter vs Adductor Canal Block in Primary Total Knee Arthroplasty Surgery. Biomed Pharmacol J 2022;15(4). |
| Copy the following to cite this URL: Sahu S. K, Mishra N. R, Sahoo S. K, Raulo B. C, Kar D. Efficacy of Local Infiltration of Analgesics via Intra-articular Epidural Catheter vs Adductor Canal Block in Primary Total Knee Arthroplasty Surgery. Biomed Pharmacol J 2022;15(4). Available from: https://bit.ly/3yYsKAK |
Introduction
Primary TKA procedures are usually associated with moderate to severe pain1,2,3. Pain management after TKA is always challenging and is believed to be a poorly understood phenomenon, which is mostly regulated by neural, cellular, hormonal & emotional components. A multimodal approach is always desirable to combat this complex phenomenon. The suggested efficacy of periarticular analgesics intraoperatively is inconsistent. Epidural analgesia is used for pain relief in patients undergoing primary TKA, though provides good pain control, many a time is associated with side effects such as hypotension, urinary retention and impaired mobility. Apart from that, the risk of hematoma and infection in the epidural space are rare but dreaded complications associated with epidural analgesia. Hence the current study aims at exploring alternative modalities of analgesia. Many studies have demonstrated that adductor canal block (ACB) can provide adequate analgesia with a multimodal analgesic regimen4-6 with better functional outcomes post-operatively in comparison with a femoral nerve block (FNB)7,8. It has been suggested in many studies that LIA (Local infiltration of analgesics) can provide superior postoperative analgesia and earlier mobilization compared to placebo9,10, intrathecal morphine9, epidural analgesia11,12 and FNB13-16. Moreover, local infiltration of analgesics is cheap and relatively easy to perform than FNB, while providing good analgesia17-22. We, therefore, compared the efficacy of IAEC vs ACB in primary TKA with respect to VAS, ROM, KSS and quadriceps recovery, in a prospective, randomized trial.
Material and Methods
The current study was done on patients undergoing primary total knee replacement at IMS & SUM Hospitals (IEC Letter No. DMR/IMS/SH/SOA/792/2019), during the study period of March 2018 to April 2020. This study is prospectively randomized, the cases undergoing primary knee replacement were divided into two groups, which includes a minimum of 36 cases in each group. Group -1(36) patients received intra-articular epidural catheter (IAEC) and Group 2 (36) patients received ACB (adductor canal block). The postoperative pain was assessed in each patient through a pain chart. Patients undergoing primary TKR who satisfy inclusion criteria were included in the study. They were admitted and examined, randomly selected and post-operative pain management will be given according to the modified Caledonian protocol in Group1/LIA by IEAC and Group-2/adductor canal block. The patients were evaluated clinically and pain management protocol was followed accordingly during their stay after the surgery at our hospital. Pain control was assessed by VAS (Visual Analogue Scale) scores and outcomes in terms of ROM achieved on the day of discharge. All patients undergoing Primary unilateral TKA, patients with osteoarthritis of the Knee and those with TKA done under spinal anesthesia were included in our study. Patients undergoing bilateral TKR, Revision TKR and those with Rheumatoid arthritis, Neuromuscular deficit, History of cardiac disease or arrhythmia requiring special monitoring, use of general anesthesia, Patients with severe renal insufficiency, uncontrolled diabetes mellitus, bleeding disorders, alcohol or drug abuse, allergy to local anesthetics were excluded from our study. Preemptive analgesia in the form of Celecoxib 200 mg, Pregabalin 75 mg (Omit pre-operative dose was omitted in patients with renal impairment) and Paracetamol 650mg, were given to all patients undergoing primary TKA, all a night before surgery. Combined Spinal and epidural anesthesia (Epidural only as intra-op backup). Post-operative analgesia was provided by peri-articular injection of 0.2% Ropivacaine solution followed by an infusion administered through a catheter placed under direct vision via a Touhy needle, inserted about 10 cm above the incision into the surgical field by outside-in technique at the end of surgery in group-1(IAEC) and USG guided Adductor canal block by local anesthetic agents in group-2(ACB). No drains were used. Ropivacaine 0.2%, 10 mL bolus was given 8 hourly and 10 ml before removal of the catheter while doing Pod 1 dressings, a top-up dose of 10 ml if severe pain complained in Group1(IAEC). 0.5% levobupivacaine 20 ml was injected after ensuring the correct placement of the needle under USG guidance in Group2 (ACB).
Intra-articular Epidural Catheter Placement (IAEC) Adductor canal block (ACB)
The patients were made to mobilize on the same day of surgery and Physiotherapy was continued thereafter. The patients were discharged, once they could move independently and their pain was controlled with oral analgesics.
Post-operative Assessment
VAS at 12hr, 24hr, 48hr, and 72hrs & at the time of discharge.
ROM at POD-3, at the time of discharge & at 4wks
Early Functional Recovery- Active SLRT, Maximum Flexion at the time of discharge.
Power of Quadriceps muscle
Opioid Consumption
Pt discharged POD
Follow up of all patients till 6 weeks to rule out any drug-related side effects & complications post-surgery (Infection)
Results
As far as age, sex, BMI (kg/m2), pre-op VAS, mean pre-op flexion, mean pre-op varus, mean pre-op KSS (Knee society score), duration of surgery and hospital stay is concerned, no significant difference was noticed between the two groups (Table I). The visual analog scores suggested that the average pain scores were significantly lower in the IAEC group as compared to the ACB group[chart-2] (Table2). The active knee flexion at POD#3, at the time of discharge and 4 weeks after surgery, was greater in the IAEC group[chart-1] (Table 3). The active SLRT showed significantly superior at the day of discharge in the IAEC group(p<0.001) compared to the ACB group, but at 2 weeks following surgery, there was no significant difference(p>0.05) between the two groups[chart-3](Table-4). The average knee society score (KSS) at 6 weeks follow-up was significantly higher in the IAEC group(90.46+/-12.6) compared to ACB group79.5+/-10.9[Table5](Chart-4). All the data were analyzed using SPSS20 software.
 |
Figure 1: Intra-articular Epidural Catheter Placement (IAEC). |
 |
Figure 2: Adductor Canal Block (ACB). |
Table 1: (Patient Demography).
| IAEC(n=36) | ACB(n=33) | P-value | |
| Age(yrs) | 69+/-7.08 | 66+/-6.56 | 0.081 |
| Gender | M:F=12:24 | M:F=11:22 | 0.609 |
| BMI | 26.56+/-4.12 | 27.48+/-2.86 | 0.076 |
| Pre-op VAS | 7.5+/-2.27 | 7.7+/-2.34 | 0.467 |
| Mean Pre-op flexion | 100.4 | 102.0 | 0.66 |
| Mean Pre-op Varus deformity(degrees) | 12.5 | 13 | 0.63 |
| Mean Pre-op KSS | 32.6 | 31.4 | 0.54 |
| Duration of surgery(Minutes) | 110.24+/-21.65 | 120.54+/-25.23 | 0.124 |
| Hospital Stay(Days) | 5+/-0 | 5.22+/-0.28 | 0.088 |
Patient Demography
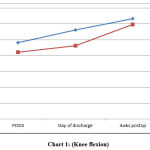 |
Chart 1: (Knee flexion). |
Table 2: Visual Analogue Scale (VAS).
| IAEC | ACB | P-value | |
| POD-0 | 2.26+/-1.28 | 3.65+/-2.24 | 0.018 |
| POD-1 | 2.5+/-2.2 | 5+/-3.2 | <0.001 |
| POD-2 | 2.3+/-1.4 | 4.6+/-1.8 | <0.001 |
| POD-3 | 2.1+/-1.6 | 4+/-1.9 | <0.001 |
| Day of Discharge | 1.6+/-1.5 | 3.4+/-2.1 | <0.001 |
Visual Analog Score
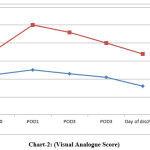 |
Chart 2: (Visual Analogue Score). |
Table 3: Knee Flexion in Degrees.
| IAEC | ACB | P-value | |
| POD-3 | 96.5+/-10.9 | 84.2+/-16.4 | <0.001 |
| Day of discharge | 112.6+/-8.4 | 92.6+/-12.5 | <0.001 |
| 4weeks post-op | 126.8+/-6.3 | 119.4+/-9.7 | <0.001 |
Knee Flexion in Degrees
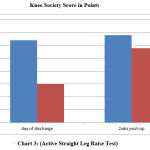 |
Chart 3: (Active Straight Leg Raise Test). |
Table 4: Active Straight Leg Raise Test
| IAEC (n=36) | ACB (n=33) | P-value | |
| Day of discharge | 32(88.8%) | 15(45.45%) | <0.001 |
| 2weeks post-op | 34(94.44%) | 29(87.87%) | 0.496 |
Knee Flexion in Degrees
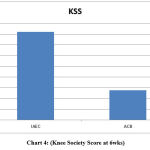 |
Chart 4: (Knee Society Score at 6wks). |
Table 5: Knee Society Score
| Time | IAEC Group | ACB Group | p-value |
| Pre-operative | 32.6 | 31.4 | 0.54 |
| 6weeks | 90.46+/-12.6 | 79.5+/-10.9 | <0.001 |
Discussion
ACB can be delivered as single-shot injections or by continuous adductor canal catheter infusion and was initially recommended as ‘pure sensory’ nerve blocks without associated motor weakness. Single-shot ACB has been recommended as an efficient measure to control pain and improved rehabilitation.23-29 Among the other modalities like, sciatic nerve block or femoral nerve block (FNB), ACB has been associated with a lower incidence of motor weakness following surgery, thus aiding faster recovery and rehabilitation. Many studies have suggested the use of ACB over FNB to avoid motor weakness and to achieve faster recovery and rehabilitation. 30-33,8 Toftdahl et al14 in their study have shown that peri- and intra-articular analgesia following total knee arthroplasty has superior analgesic effects and achieved faster rehabilitation as compared to continuous FNB. Andersen et al12 found that peri and intra-articular infusion of ropivacaine improved analgesia as compared to epidural infusions. In their study, Smith et al 37 reported lower VAS for patients receiving intra-articular bupivacaine infusion as compared to periarticular liposomal bupivacaine injection. Many studies have suggested that intraoperative periarticular injection following primary total knee arthroplasty has significantly reduced the amount of postoperative analgesia required10,34,18,35 with relatively lower pain scores10,4,35. The visual analog scale suggested that the average pain scores were significantly lower in the IAEC group, compared to the ACB group (chart-2).In our study, VAS on IAEC placement patients was significantly lower on the day of surgery, POD 1-3 and on the day of discharge when compared with the ACB patients (Table 2). Acute pain, even if of short duration, if not addressed appropriately may result in sensitization of the nervous system, causing chronic pain 36,37. This could be the reason why low pain levels were recorded in the IAEC group as compared to the ACB group at the time of discharge. The active knee flexion at POD-3, at the time of discharge and 4 weeks post-surgery, was significantly greater in the IAEC group as compared to the ACB group [chart-1] (Table 3). Because of better pain relief in the IAEC group, encouraged early mobilization and facilitate physiotherapy following the surgery. The number of patients, who were able to do active SLR, was significantly higher in the IAEC knee compared with the ACB knee at the time of discharge [chart-3] (Table-4). Although the difference was not significant at 2weeks post-op. Average knee society score (KSS) at 6 weeks follow-up was significantly higher in the IAEC group compared to the ACB group [Table5](Chart-4). . In their study Feibel et al 38 showed an increased incidence of falls following surgery in patients receiving continuous femoral nerve block. Adductor canal block can also result in motor deficit because of the proximal spread of the drugs.23,26 But the incidence is very low. In the current study, none of our patients had experienced falls, at any time following the procedure.
Conclusion
The current study suggests that Local infiltration of analgesics by IAEC (Intraarticular Epidural Catheter) for patients undergoing primary TKA is a better option compared to single shot adductor canal block, as far as pain levels, opioid usage, range of motion, quadriceps recovery and KSS (Knee society score) is concerned. Because of better pain relief in the IAEC group, it encouraged early mobilization and facilitates physiotherapy following the surgery. Moreover, IAEC is a rather easier procedure to perform, when compared to that of single shot ACB, which requires an experienced anesthesiologist.
Acknowledgement
The authors are highly grateful to the Chairman and the Dean, IMS & SUM Hospital, Siksha O Anusandhan (deemed to be) University for providing the necessary facility during the period of study.
Conflict of Interest
The Authors declare there is no conflict of interest.
Funding Source
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- Strassels S. A, Chen C andCarr D.B. Postoperative analgesia: economics, resource use, and patient satisfaction in an urban teachinghospital. Anesth Analg.,2002;94(1):130-7.
CrossRef - Wu C. L, and Richman J. M. Postoperative pain and quality of recovery. Curr Opin Anaesthesiol.,2004; 17(5): 455-60.
CrossRef - Mishra N. R, Sahu S. K, Kar D. Approach to Manage Post-traumatic Revision Anterior Cruciate Ligament Reconstruction Associated with a Hoffa Fracture of the Medial Femoral Condyle: A Case Report.J Health Sci Med Res.,2022. http://dx.doi.org/10.31584/ jhsmr.2022873
CrossRef - Jenstrup M. T, J.ger P, Lund J, Fomsgaard J. S, Bache S, Mathiesen O.et al. Effect of adductor-canal-blockade on pain and ambulation after total knee arthroplasty: a randomized study. ActaAnaesthesiol Scand.,2012; 56(3): 357-64.
CrossRef - Hanson N. A, Allen C. J, Hostetter L. S, Nagy R, Derby R. E, Slee A. E.et al. Continuous ultrasound-guided adductor canal block forntotal knee arthroplasty: a randomized, double-blind trial. ,2014; 118(6): 1370-7.
CrossRef - Andersen H. L, Gyrn J, Moller L, Christensen B, Zaric D. Continuous saphenous nerve block as supplement to single-dose local infiltration analgesia for postoperative pain management after total knee arthroplasty. RegAnesth Pain Med.,2013; 38(2):106-11.
CrossRef - Nader A, Kendall M. C, Manning D. W, Beal M, Rahangdale R, Dekker R, et al. Single-dose adductor canal block with local infiltrative analgesia compared with local infiltrate analgesia after total knee arthroplasty: a randomized, double-blind, placebocontrolled trial. RegAnesth Pain Med.,2016; 41(6): 678-84.
CrossRef - Kwofie M. K and Shastri U. canal block versus femoral nerve block on quadriceps strength and fall risk: a blinded, randomized trial of volunteers. RegAnesth Pain Med., 2013; 38(4): 321-5.
CrossRef - Elkassabany N. M, Antosh S, Ahmed M, Nelson C, Israelite C, Badiola I.et al. The risk of falls after total knee arthroplasty with the use of a femoral nerve block versus an adductor canal block: A double-blinded randomized controlled study. , 2016; 122(5): 1696-703.
CrossRef - Busch C. A, Shore B. J, Bhandari R, Ganapathy S, MacDonald S. J, Bourne R. B.et al. Efficacy of periarticular multimodal drug injection in total knee arthroplasty. A randomized trial. J Bone Joint Surg Am.,2006; 88(5): 959-63.
CrossRef - Essving P, Axelsson K, Aberg E, Spannar H, Gupta A, Lundin A. Local infiltration analgesia versus intrathecal morphine for postoperative pain management after total knee arthroplasty: a randomized controlled trial. ,2011; 113(4): 926-33.
CrossRef - Andersen K. V, Bak M, Christensen B. V, Harazuk J, Pedersen N. A, Soballe K. A randomized, controlled trial comparing local infiltration analgesia with epidural infusion for total knee arthroplasty. ,2010; 81(5): 606-10.
CrossRef - Thorsell M, Holst P, Hyldahl H. C, Weidenhielm L. Pain control after total knee arthroplasty: a prospective study comparing local infiltration anesthesia and epidural anesthesia. ,2010; 33(2): 75-80.
CrossRef - Toftdahl K, Nikolajsen L, Haraldsted V, Madsen F, Tonnesen E. K, Soballe K. Comparison of peri- and intraarticular analgesia with femoral nerve block after total knee arthroplasty: a randomized clinical trial. ,2007; 78(2): 172-9.
CrossRef - Chaumeron A, Audy D, Drolet P, Lavigne M, Vendittoli P. A. Periarticular injection in knee arthroplasty improves quadriceps function. ClinOrthopRelat Res. 2013; 471(7): 2284-95.
CrossRef - Ashraf A, Raut V. V, Canty S. J, McLauchlan G. J. Pain control after primary total knee replacement. A prospective randomized controlled trial of local infiltration versus single shot femoral nerve block. ,2013; 20(5): 324-7.
CrossRef - Uesugi K, Kitano N, Kikuchi T, Sekiguchi M, Konno S. I. Comparison of peripheral nerve block with periarticular injection analgesia after total knee arthroplasty: a randomized, controlled study. ,2014; 21(4): 848-52.
CrossRef - Parvataneni H. K, Shah V. P, Howard H, Cole N, Ranawat A. S, Ranawat C. S. Controlling pain after total hip and knee arthroplasty using a multimodal protocol with local periarticular injection: a prospective randomized study. J Arthroplasty.,2007; 22(6 Suppl 2): 33-8.
CrossRef - Affas F, Nygards E. B, Stiller C. O, Wretenberg P, Olofssen C. Pain control after total knee arthroplasty: a randomized trial comparing local infiltration anesthesia and continuous femoral nerve block. Acta Orthop.,2011; 82(4): 441-7.
CrossRef - Spangehl M. J, Clarke H. D, Hentz J. G, Misra L, Blocher J. L, Seamans D. P. Periarticular injections and femoral & sciatic blocks provide similar pain relief after TKA: A randomized clinical trial. ClinOrthopRelat Res.,2015; 473(1): 45-53.
CrossRef - Ng F. Y, Ng J. K. F, Chiu K. Y, Yan C. H, Chan C. W. Multimodal periarticular injection vs continuous femoral nerve block after total knee arthroplasty: a prospective, crossover, randomized clinical trial. J Arthroplasty.,2012; 27(6): 1234-8.
CrossRef - Carli F, Clemente A, Asenjo J. F, Kim D. J, Mistraletti G, Gomarasca M.et al. Analgesia and functional outcome after total knee arthroplasty: periarticular infiltration vs continuous femoral nerve block. Br J Anaesth.,2010; 105(2): 185-95.
CrossRef - Sankineani S. R, Reddy A. R. C, Eachempati K. K, Jangale A, Gurava Reddy A. V. Comparison of adductor Canal block and IPACK block (interspace between the popliteal artery and the capsule of the posterior knee) with adductor canal block alone after total knee arthroplasty: A prospective control trial on pain and knee function in immediate postoperative period. Eur J Orthop Surg Traumatol.,2018; 28(7): 1391–1395.
CrossRef - Gibbs D. M. R, Green T. P, Esler C. N. The local infiltration of analgesia following total knee replacement. J Bone Joint Surg Br.,2012; 94-B(9): 1154–1159.
CrossRef - Cui Y, Yang T, Zeng C, et al. Intra-articular Bupivacaine after joint arthroplasty: A systematic review and meta-analysis of randomised placebo-controlled studies. BMJ Open.,2016; 6(7): e011325.
CrossRef - Kasture S, Saraf H. Epidural versus intra-articular infusion Analgesia following total knee replacement. J Orthop Surg (Hong Kong).,2015; 23(3): 287–289.
CrossRef - Antoni M, Jenny J. Y, Noll E. Postoperative pain control by intra-articular local anesthesia versus femoral nerve block following total knee arthroplasty: Impact on discharge. Orthop Traumatol Surg Res.,2014; 100(3): 313–316.
CrossRef - Halawi M. J, Grant S. A, Bolognesi M. P. Multimodal analgesia for total joint arthroplasty. Orthopedics.,2015; 38(7): e616-25.
CrossRef - Beausang D. H, Pozek J-P, Chen A. F, et al.. A randomized controlled trial comparing adductor canal catheter and intraarticular catheter after primary total knee arthroplasty. J Arthroplasty.,2016; 31(9 Suppl): 298–301.
CrossRef - Jaeger P, Nielsen Z. J. K, Henningsen M. H, Hilsted K. L, Mathiesen O, Dahl J. B. Adductor canal block versus femoral nerve block and quadriceps strength: A randomized, double-blind, placebo-controlled, crossover study in healthy volunteers. Anesthesiology.,2013; 118(2): 409–415.
CrossRef - Kim D. H, Lin Y, Goytizolo E. A, et al.. Adductor canal block versus femoral nerve block for total knee arthroplasty: A prospective, randomized, controlled trial. Anesthesiology.,2014; 120(3): 540–550.
CrossRef - Shah N. A, Jain N. P. Is continuous adductor canal block better than continuous femoral nerve block after total knee arthroplasty? Effect on ambulation ability, early functional recovery and pain control: A randomized controlled trial. J Arthroplasty.,2014; 29(11): 2224–2229.
CrossRef - Mudumbai S. C, Kim T. E, Howard S. K, et al.. Continuous adductor canal blocks are superior to continuous femoral nerve blocks in promoting early ambulation after TKA. Clin Orthop Relat Res.,2014; 472(5): 1377–1383.
CrossRef - Peters C. L, Shirley B and Erickson J. The effect of a new multimodal perioperative anesthetic regimen on postoperative pain, side effects, rehabilitation, and length of hospital stay after total joint arthroplasty. J Arthroplasty.,2006; 21(6 Suppl 2): 132-8.
CrossRef - Vendittoli P. A, Makinen P and Drolet P. et al. A multimodal analgesia protocol for total knee arthroplasty: a randomized, controlled study. J Bone Joint Surg.,2006; 88A: 282-9.
CrossRef - Carr D. B and Goudas L. C. Acute pain. Lancet.,1999; 353(9169): 2051-8.
CrossRef - amad T. A, Moore K .A and Sapirstein A. et al. Interleukin-1beta– mediated induction of Cox-2 in the CNS contributes to inflammatory pain hypersensitivity. Nature., 2001; 410: 471-5.
CrossRef - Feibel R. J, Dervin G. F, Kim P. R, Beaulé P. E. Major complications associated with femoral nerve catheters for knee arthroplasty: A word of caution. J Arthroplasty.,2009; 24(6 Suppl): 132–137.
CrossRef
Abbreviations
LIA- Local Infiltration of Analgesics
IAEC- Intra-articular Epidural Cathetre
ACB- Adductor Canal Block,
TKA – Total Knee Arthroplasty
KSS – Knee society score
SLRT – Straight Leg Raise Test
POD -Post Operative Day
FNB- Femoral Nerve Block
VAS- Visual Analogue Scale
ROM- Range Of Motion.








