Christopher Amalraj Vallaba Doss1* , Arun Vijay Subbarayalu2
, Arun Vijay Subbarayalu2 , Mohsina Bano3
, Mohsina Bano3 , Malik Khurram Shahzad Awan1
, Malik Khurram Shahzad Awan1 and Mohammed Barkath Ali4
and Mohammed Barkath Ali4
1Development and Community Partnership, College of Medicine, Imam Abdulrahman Bin Faisal University, P.O. Box 1982, Dammam 31441, Saudi Arabia.
2Quality Measurement and Evaluation Department, Deanship of Quality and Academic Accreditation, Imam Abdulrahman Bin Faisal University, P.O No. 1982, Dammam 31441, Saudi Arabia
3Department of Pharmaceutical Chemistry, College of Clinical Pharmacy, Imam Abdulrahman Bin Faisal University PO Box 1982, Dammam 31441, Saudi Arabia
4Vice Deanship for Academic Affairs, College of Medicine, Imam Abdulrahman Bin Faisal University, P.O Box 1982, Dammam 31441, Saudi Arabia
Corresponding Author Email: christopheramalraj@gmail.com
DOI : https://dx.doi.org/10.13005/bpj/2536
Abstract
Background and aim: The COVID-19 Pandemic necessitates strict lockdowns worldwide to prevent its spread, which has hurt people's lives, including students, on a physical, economic, and emotional level. This study examines the impact of the COVID-19 lockdown on the quality of sleep and the prevalence of insomnia among college students in Chennai. Methods: Using a random sampling approach, collegiate students (n=450) are invited to complete Pittsburgh Sleep Quality Index (PSQI) and Insomnia Severity Index (ISI). Frequencies, unpaired T-test, and the chi-square test were the statistical techniques employed to assess the data. Results: The findings imply that 48% of students experienced poor sleep quality, and 37% reported Subthreshold insomnia during the COVID-19 lockdown. Even though no gender difference was observed regarding the overall sleep quality and insomnia scores, there is a significant association observed between gender with sleep quality; however, those failed to show a significant association with insomnia. Conclusions: Thus, the study concluded that the lockdown has affected sleep quality and led to insomnia among college students.
Keywords
COVID-19; life quality; Insomnia; Lockdown; Sleep quality; Sleep disorders
Download this article as:| Copy the following to cite this article: Doss C. A. V, Subbarayalu A. V, Bano M, Awan M. K. S, Ali M. B. Effect of COVID-19 Lockdown on Sleep Quality and Insomnia in Collegiate Students. Biomed Pharmacol J 2022;15(4). |
| Copy the following to cite this URL: Doss C. A. V, Subbarayalu A. V, Bano M, Awan M. K. S, Ali M. B. Effect of COVID-19 Lockdown on Sleep Quality and Insomnia in Collegiate Students. Biomed Pharmacol J 2022;15(4). Available from: https://bit.ly/3hyhiGm |
Introduction
The first case of the novel coronavirus disease 2019 (COVID-19) was found in Wuhan, Hubei Province of China, in December 2019. Later, it spreads rapidly across the globe 1-3. Subsequently, the World Health Organization (WHO) acknowledged this disease as an international emergency. The rapid spread of COVID-19 referred to unique restrictions resisting its transmission and alleviating its impact 4. As a result, many nations took various preventive measures to control the spread of COVID-19. Further, to lessen the spread of COVID‑19 infection, worldwide nations have implemented “lockdowns,” which have limited people to their homes 5, and encouraged safety compliance such as social distancing, hygiene, and wearing face mask 6. In addition, sterilization strategies imposed on the public, as in different nations, reduced the virus from invading its host and spread 7. Accordingly, in response to the COVID-19 pandemic, India executed lockdown measures to control the transmission of the SARS-CoV-2 virus, which causes COVID-19 8. India followed the lockdown in four phases from 24 March 2020 to 31 May 2020; later, it introduced unlock period in different phases 9. In general, lockdown measures over the COVID-19 pandemic have globally resulted in unparalleled variations in human behaviour 10. A more recent study by Ali et al. (2021) also stated that the government-mandated lockdown could mitigate psychological effects on young adults, especially students [11]. In conformance with government efforts to mitigate the spread of COVID-19 infection in India, the ministry of home affairs declared to remain close to the colleges and schools across the country till 31 July 2020 12.
As schools and colleges turn to online education, students are prone to deprived quality sleep, and it has been related to increased anxiety levels 13. It is also suggested that sleep quality is very strongly associated with mental health 14. For instance, most persons with clinical depression demonstrate insomnia features, a substantial risk element for depression 15. Simon Evans et al. (2021) stated the effect of the pandemic and lockdown on sleep quality and diurnal preference, which are closely interconnected with mental health, chiefly in young adults. During lockdowns, sleep habits have altered due to social isolation and variations in social rhythms (work- and daily work) 16. Sleep disorders or insufficient sleep disorders lead to accidents, depression, epilepsy, diabetes, cardiac disease, and reduced life quality 17.
Few studies have been conducted on sleep and sleep disorders during the COVID-19 pandemic 18, 19. On reviewing the literature across the globe, authors measured the sleep quality of different populations during the lockdown through the “Pittsburgh sleep quality index (PSQI)” 20, 21. Other than the common public, Marelli et al. (2021) studied the effect of the COVID-19 lockdown on university administration staff and students in Italy 22. It was found that 60.2% and 73.3%of the university administration staff and students felt poor sleep quality. Ali et al. (2021) also reported that the sleeping pattern among Pakistani students was mainly affected due to the lockdown during the COVID-19 pandemic 11. Furthermore, few researchers have studied the effect of the COVID-19 pandemic and lockdown on sleep and mental health among students across the globe 15, 23-26. Likewise, in the Indian context, researchers have exclusively studied the influence of the COVID-19 lockdown on sleep quality and perceived stress among the general population of India during the COVID-19 pandemic through PSQI and the insomnia severity index (ISI), respectively. 5, 27, 28.
Nevertheless, much-limited studies have been conducted to ascertain the quality of sleep of Indian students 29. Realizing this research gap, this study examined the effect of the COVID-19 lockdown on sleep quality and Insomnia in collegiate students, particularly in Tamilnadu, India. Thus, this study aims to address: (i) the extent of the quality of sleep and insomnia; (ii) any difference between gender in the overall quality of sleep and Insomnia, and (iii) any association between gender concerning the two categories of sleep quality (‘good’ or ‘poor’) and four categories of Insomnia and (iv) any relationship between sleep quality (i.e., PSQI total score) and Insomnia (i.e., ISI total score) among the Collegiate students during the COVID 19 pandemic.
Methodology
Study Design
A cross-sectional observational study design was adopted to study the impact of the COVID-19 lockdown on sleep quality and insomnia in collegiate students, particularly in Tamilnadu, India.
Samples
All the undergraduate students studying from the first year to the final year belonging to SRM College of Health Science were identified as the population for this study. Among them, 450 students were picked up using a random sampling approach. Utmost care was taken to recruit students from all the health science programs in this study.
Methods
With prior permission from the head of each health science college and following the guideline for researching at SRM College, the researchers have sent the survey link and surveyed all the students via email. All the students were asked to respond after filling out the informed consent form. The survey was kept open for a pre-specified period between March 25 to May 31, 2020. In addition, frequent reminders were sent to all the students to participate in the survey. Four hundred sixteen completed questionnaires out of 450 sent were received, demonstrating a 92% response rate. After scrutiny of the data, sixteen survey responses were discarded due to the incomplete response from the students to specific questions. Finally, the completed response from 400 samples was subjected to statistical analysis.
Instrumentation
Pittsburgh Sleep Quality Index (PSQI)
The PSQI is a 19-item questionnaire assessing sleep quality and disturbances over the past month 30. The first four items are open-ended questions, whereas items 5 to 19 are rated by the subjects on a 4-point Likert scale. Individual item scores yield seven components. A total score, ranging from 0 to 21, is calculated by combining the 7 component scores. Any total score of greater than 5 implies poor sleep quality. The psychometric properties of the PSQI were already established by earlier studies 31, 32.
Insomnia Severity Index (ISI)
The ISI is a 7-item self-report questionnaire assessing the nature, severity, and impact of insomnia. The usual recall period is the “last month,” and the dimensions evaluated include: ‘severity of sleep onset’, ‘sleep maintenance’, ‘early morning awakening problems’, ‘sleep dissatisfaction’, ‘interference of sleep difficulties with daytime functioning’, ‘noticeability of sleep problems by others’, and ‘distress caused by the sleep difficulties. Each item is rated using a five-point Likert scale ranging from 0 to 4 (e.g., 0 = no problem; 4 = very severe problem), yielding a total score varying from 0 to 28. Based on the total score, insomnia is categorized as follows: absence of insomnia (0–7); sub-threshold insomnia (8–14); moderate insomnia (15–21); and severe insomnia (22–28). Earlier studies have reported good psychometric properties for this scale 33, 34.
Statistical analysis
The data were analyzed using the Statistical Package of Social Sciences (SPSS) version 20.0 (IBM Corp). To evaluate the gathered data, categorical variables (PSQI Scores/Sleep quality categories) expressed as frequencies & percentages, and continuous variables (PSQI global score/ISI total score) were presented using means and standard deviations. An unpaired T-test was used to study the differences between gender concerning sleep quality and insomnia as measured through PSQI global score and ISI total score, respectively. In addition, a Chi-square test was used to evaluate the association between gender concerning the stages of sleep quality and four categories of insomnia. A P-value of less than 0.05 was considered statistically significant.
Results
Demographic details of the participants
Of 400 students who participated, 41% were males, and 59% were female. Male students’ mean age is 20.76, whereas the mean female was 20.44 years.
Table 1 shows the PSQI global score and ISI total score for the entire sample and male and female students separately. The overall global PSQI score was 5.81±3.26 for all participants; male students’ scores were 6.07, whereas female students’ scores were 5.63. Similarly, the ISI total score was 8.19±5.81 for all participants; the ISI total score for males and females is 8.61 and 7.89, respectively.
Table 1: Comparison between male and female students regarding PSQI global score and ISI total Scores during COVID 19 emergency.
| Parameter | Gender | Mean ± SD | Independent t-value | p-value |
| PSQI global score | Male | 6.07± 3.18 |
1.343 |
0.180-ns |
| Female | 5.63± 3.31 | |||
| ISI total score | Male | 8.61± 5.95 | 1.224 | 0.222-ns |
| Female | 7.89± 5.71 |
ns-Not Statistically significance at 95% (p >0.05).
Table 1 shows no significant difference between gender concerning sleep quality and insomnia as revealed through the p-value at 95% confidence level. Table 2 depicts the categorization of the participants based on their response to PSQI Scores as either ‘good quality sleep’ (<5) or ‘poor-quality sleep’ (>5) and four stages of the Insomnia Severity Index. The results found that 48% of students experienced poor sleep quality during the covid pandemic, as shown through the PSQI global score. Similarly, 37% of them reported Subthreshold insomnia, and 9% have moderate Clinical insomnia. 51% of the students said that they do not have clinically significant insomnia. It is noteworthy to mention that only 2.5 % have severe clinical insomnia.
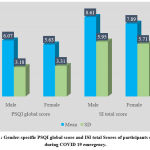 |
Figure 1: Gender-specific PSQI global score and ISI total Scores of participants observed during COVID 19 emergency. |
Table 2: Categorization of Sleep quality and insomnia reported by the participants during COVID 19 pandemic.
|
Pittsburgh Sleep Quality Index (PSQI) |
||
| PSQI Scores and Sleep quality categories | N | Percentage |
| PSQI score <5 | 208 | 52 |
| PSQI score >5 | 192 | 48 |
| PSQI Total Score | 400 | 100 |
| Insomnia Severity Index (ISI) | ||
| ISI Scores & Insomnia Stages | N | Percentage |
| No clinically significant insomnia (0-7) | 205 | 51.3 |
| Subthreshold insomnia (8-14) | 149 | 37.2 |
| Clinical insomnia (moderate severity) (15-21) | 36 | 9.0 |
| Clinical insomnia (severe) (22-28) | 10 | 2.5 |
| ISI total score | 400 | 100 |
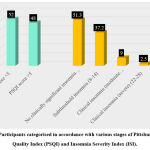 |
Figure 2: Participants categorised in accordance with various stages of Pittsburgh Sleep Quality Index (PSQI) and Insomnia Severity Index (ISI). |
(Further exploration was carried out to study whether there is an association between gender concerning each category of sleep quality and insomnia index (Table 3).
From the results, it is observed that there is an association between gender, taking into consideration each stage of sleep quality, as shown by the p-value at 0.05 levels of significance (p<0.05). 34% (n=135) of females reported good sleep during COVID 19 pandemic, whereas 18% (n=73) of male students agreed to it. However, there is no association between gender about all the four categories of insomnia, as revealed through the p-value (p=0.276).
Table 3: Association between gender with regard to the stages of sleep quality and insomnia
|
PSQI & ISI categories |
Gender | Chi-Square | P-value | |||
| Male
N (%) |
Female
N (%) |
Total
N (%) |
5.737
|
0.017* |
||
| PSQI | Good quality of sleep
(< 5) |
73(18.3) | 135(33.8) | 208(52) | ||
| Poor quality of sleep (≥5) | 90(22.5) | 102(25.5) | 192(48) | |||
| ISI | No clinically significant insomnia (0-7) | 78(19) | 129(32.3) | 205(51.3) | 4.86 | 0.276-ns |
| Subthreshold insomnia
(8-14) |
70(17.5) | 79(19.6) | 149(37.3) | |||
| Clinical insomnia (moderate severity)
(15-21) |
13(3.3) | 23(5.8) | 36(9) | |||
| Clinical insomnia (severe) (22-28) | 4(1) | 6(1.5) | 10(2.5) | |||
*Statistical significance at 95% (p < 0.05), ns-Not Statistically significance at 95% (p >0.05).
Table 4 shows the relationship between PSQI and ISI totals scores of collegiate students during COVID 19 pandemic, and it is found that there is a significant positive correlation between the two parameters at 0.01 levels (r=0.70, p < 0.001).
Table 4: Correlation coefficient showing the relationship between PSQI and ISI totals scores of collegiate students during COVID 19 pandemic.
| Parameters | M ± SD | N | Correlation (r) | p-value |
| ISI total score | 8.19 ± 5.81 | 400 | 0.702 | 0.0001*** |
| PSQI global score | 5.81 ± 3.26 | 400 |
*** Statistically significant at 95% (p < 0.05).
Discussion
Even though several studies have been conducted to ascertain the effect of lockdown on students’ sleep quality, minimal studies have focused on examining gender impact on sleep quality and insomnia among college students during the pandemic. Thus, the authors intended to document the effect of the COVID-19 lockdown on sleep quality and insomnia in collegiate students, and it attempted to uncover whether there is no difference between gender concerning sleep quality and insomnia.
Our study findings indicated that half of the respondents experienced poor sleep quality, as evident from the PSQI score (>5, 48%) during the lockdown period enforced because of the pandemic. Similarly, over 35% experience subthreshold insomnia, and less than 10% are prone to clinical insomnia during the lockdown period. This finding might be due to traumatic incidents, such as those caused by the COVID-19 outbreak can create psychological distress and anxiety symptoms that negatively affect sleep quality [35]. Another reason might be the change in the strategy of reducing physical contact to reduce the spread of COVID-19, and the government of India enforced a nationwide lockdown on 24th March 2020 for 21 days to combat the spread of the coronavirus, and it has extended until August 2021. Furthermore, to continue to provide educational support to the students during the lockdown, most colleges shift to the online teaching method, which necessitates continuous usage of computers by the students. As a result, students are accumulating to the new life of study, which may influence sleep quality 36.
An earlier study also indicated that those students use devices and gadgets late at night, which may impair their sleeping patterns [35]. Another possible explanation is that those blue lights from devices and gadgets can suppress melatonin secretion, thus reducing sleep quality 37, 38. In this study, 51.3% of the respondents reported no clinically significant insomnia during the lockdown period. This observation is contrary to Marelli et al. (2021), who found that the Italian COVID-19 lockdown potentially affected sleep and psycho-emotional well-being7. This effect was more significant in students than administrative staff and greater in females than males. It is observed that the home quarantine during the lockdown showed a more significant impact on the sleep habits of students than workers concerning bedtime and wake-up delay. Previous studies have also stated that during the lockdown, sleep habits altered from the social limitations and to a change of social rhythms, like working and daily events plan 16, 39, 40. The reason for difference between our observation as well reported in the earlier studies need to be discovered in future studies.
Further exploration was carried out to ascertain how sleep quality and insomnia varies between gender. There is no difference between males and females regarding the overall sleep quality and insomnia as visualized through the PSQI global and ISI total scores (p>0.05). Contrary to our observations, Li et al. (2020) observed that the females showed significantly higher than males on PSQI total score and sleep disturbances. Notably, Alharbi et al. (2021) observed no significant gender difference in insomnia among the Saudi population 41.
Likewise, while categorizing the participants’ response between good quality (<5) and poor quality of sleep (>5), a significant association was found between the gender. In line with this finding, an earlier study by Cheng et al. (2012) found that poor sleep quality was significantly associated with undergraduate students and the female gender. On the contrary, no significant association was found between the gender while categorizing the participants’ responses as per four categories of insomnia (p=0.276). More females than males reported subthreshold insomnia [male=18%; females=20%] and clinical insomnia [male=4%; females=6%] (Table 4). Contrary to this finding, Cheng et al. (2012) observed that gender is closely related to insomnia in college students during COVID-19 42.
Lastly, this study observed a positive relationship between PSQI and ISI totals scores of college students during the COVID-19 pandemic. Conversely, Varma et al. (2021) observed poorer sleep quality and increased insomnia-related symptoms during the COVID-19 pandemic 43.
Conclusion
This study revealed the effect of the COVID-19 lockdown on sleep quality and insomnia in collegiate students. During the COVID-19 lockdown, nearly half of the collegiate students experienced poor sleep quality. Also, 37.2% experienced subthreshold insomnia, and less than 10% were prone to clinical insomnia. Furthermore, no gender difference was observed among collegiate students regarding the overall sleep quality and insomnia scores. The gender of the collegiate students showed a significant association with sleep quality; however, those failed to show a significant association with insomnia. A positive relationship was observed between PSQI and ISI totals scores of the collegiate students during the COVID-19 pandemic. These findings clearly stated that the COVID-19 lockdown has affected sleep quality and led to insomnia among collegiate students.
Limitations
The conclusion of this study is based on the responses of the students from selected study settings, and the findings must be generalized with caution. Further, this study covers only health science college students’ perceptions of sleep quality and insomnia, and future work should cover more comprehensive samples of students belonging to other academic disciplines. Finally, since the findings are from self-reported surveys, further work can use more sophisticated clinical methods must be adopted to study insomnia and sleep quality.
Acknowledgements
We would also like to show our gratitude to the SRM College of Health Science for sharing their pearls of wisdom with us during this research.
Conflict of Interest
There is no conflict of interest
Funding Source
There are no funding sources.
References
- Velavan TP, Meyer CG. The COVID-19 epidemic. Trop Med Int Health 2020; 25: 278-280.
CrossRef - Wu YC, Chen CS, Chan YJ. The outbreak of COVID-19: An overview. J Chin Med Assoc 2020; 83: 217-220.
CrossRef - Bahbah EI, Negida A, Nabet MS. Purposing Saikosaponins for the treatment of COVID-19. Med Hypotheses 2020; 140: 109782.
CrossRef - Coronavirus Disease (COVID-19) Situation Report-110. 2020. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports (accessed on 9 May 2020).
- Gupta R, Grover S, Basu A, Krishnan V, Tripathi A, Subramanyam A, et al. Changes in sleep pattern and sleep quality during COVID‑19 lockdown. Indian J Psychiatry 2020;62:370-8.
CrossRef - Al-Bsheish, M., Mu’tamanJarrar, A. S. A Public Safety Compliance Model of Safety Behaviors in the Age of the COVID-19 Pandemic. Inquiry: A Journal of Medical Care Organization, Provision and Financing,2021,58.
CrossRef - Marelli, S., Castelnuovo, A., Somma, A., Castronovo, V., Mombelli, S., Bottoni, D., Leitner, C., Fossati, A., Ferini-Strambi, L. Impact of COVID-19 lockdown on sleep quality in university students and administration staff. Journal of neurology, 2021, 268(1), 8–15. https://doi.org/10.1007/s00415-020-10056-6
CrossRef - Mandal M, Mandal S. Exploring the Effectiveness of Lockdown in COVID-19 Pandemic Containment in India. Am J Med Public Health. 2020; 1(1): 1005.
- Saha, J., and Chouhan, P. Lockdown and unlock for the COVID-19 pandemic and associated residential mobility in India. International Journal of Infectious Diseases, 2021,104(2021), 382-389.
CrossRef - Kocevska D, Blanken TF, Van Someren EJW, Rösler L. Sleep quality during the COVID-19 pandemic: not one size fits all. Sleep Med. 2020 Dec;76:86-88.Doi: 10.1016/j.sleep.2020.09.029.
CrossRef - Ali A, Siddiqui AA, Arshad MS, Iqbal F, Arif TB. (2021). Effects of COVID-19 pandemic and lockdown on lifestyle and mental health of students: A retrospective study from Karachi, Pakistan. Ann Med Psychol (Paris). 2021 Feb 15. Doi: 10.1016/j.amp.2021.02.004.
CrossRef - India Today (2020 June 30). Schools and colleges in India to remain closed till July 31: MHA guidelines for Unlock 2. India Today, New Delhi. Retrieved from https://www.indiatoday.in/education-today/news/story/schools-and-colleges-india-remain-closed-till-july-31-mha-guidelines-unlock-2-1695292-2020-06-29
CrossRef - Norbury, R., Evans, S., 2019. Time to think subjective sleep quality, trait anxiety and university start time. Psychiatry Res. 271, 214–219. https://doi.org/10.1016/j. psychres.2018.11.054.
CrossRef - Nutt, D., Wilson, S., Paterson, L., 2008. Sleep disorders as core symptoms of depression. Dialogues Clin. Neurosci. 10, 329–336. https://doi.org/10.31887/DCNS.2008.10.3/ dnutt.
CrossRef - Simon Evans, Erkan Alkan, Jazmin K. Bhangoo, Harriet Tenenbaum, Terry Ng-Knight. Effects of the COVID-19 lockdown on mental health, wellbeing, sleep, and alcohol use in a UK student sample. Psychiatry Research, Volume 298, 2021, 113819. https://doi.org/10.1016/j.psychres.2021.113819
CrossRef - Altena E, Baglioni C, Espie CA, Ellis J, Gavriloff D, Holzinger B, et al. Dealing with sleep problems during home confinement due to the COVID-19 outbreak: Practical recommendations from a task force of the European CBT-I Academy. J Sleep Res 2020; 29: e13052.
CrossRef - Stores G. Clinical diagnosis and misdiagnosis of sleep disorders. J NeuralNeurosurgery Psychiatry [Internet] 2007; 78: 1293-1297.
CrossRef - Xiao H, Zhang Y, Kong D, Li S, Yang N. Social Capital and Sleep Quality in Individuals Who Self-Isolated for 14 Days During the Coronavirus Disease 2019 (COVID-19) Outbreak in January 2020 in China. Med Sci Monit2020; 12; 26.
CrossRef - Belingheri M, Paladino ME, Riva MA. Working schedule, sleep quality and susceptibility to COVID-19 in healthcare workers. Clin Infect Dis 2020; 27: ciaa499.
- Alharbi AS, Alshahrani SM, Alsaadi MM, Al-Jahdali HH, Wali SO, BaHammam AS. Sleep quality and insomnia during the COVID-19 lockdown among the Saudi public: A cross-sectional study. Saudi Med J. 2021 Apr;42(4):384-390. Doi: 10.15537/smj.2021.42.4.20200735.
CrossRef - Huang Y, Zhao N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional survey. Psychiatry Res 2020; 288: 112954.
CrossRef - Odriozola-González P, Planchuelo-Gómez Á, Irurtia MJ, de Luis-García R. Psychological effects of the COVID-19 outbreak and lockdown among students and workers of a Spanish university. Psychiatry Res. 2020 Aug; 290:113108. Doi: 10.1016/j.psychres.2020.113108.
CrossRef - Baloch GM, Sundarasen S, Chinna K, Nurunnabi M, Kamaludin K, Khoshaim HB, Hossain SFA, AlSukayt A. 2021. COVID-19: exploring impacts of the pandemic and lockdown on mental health of Pakistani students. PeerJ 9: e10612 DOI 10.7717/peerj.10612
CrossRef - Saadeh, H., Saadeh, M., Almobaideen, W., Al Refaei, A., Shewaikani, N., Al Fayez, R. Q., Khawaldah, H., Abu-Shanab, S., and Al-Hussaini, M. (2021 February 16). Effect of COVID-19 quarantine on the sleep quality and the depression symptom levels of university students in Jordan during the Spring of 2020. Frontiers in Psychiatry, https://doi.org/10.3389/fpsyt.2021.605676
CrossRef - Romero-Blanco, C., Rodríguez-Almagro, J., Onieva-Zafra, M. D., Parra-Fernández, M. L., Prado-Laguna, M., & Hernández-Martínez, A. (2020). Sleep Pattern Changes in Nursing Students during the COVID-19 International journal of environmental research and public health, 17(14), 5222. https://doi.org/10.3390/ijerph17145222
CrossRef - Ali K, Mufti U, Mufti A. (2020). Impact of COVID-19 Lockdown on Sleep Quality in Students: A Cross Sectional Study. Ann. Int. Med. Den. Res. 2020; 6(6):PH01-PH03.
- Joshi A., Jabbar F.A, Md. Ajmal RS &Anto L. (2020). Insomnia and perceived stress among Indian young adults during COVID-19 pandemic. International Journal of Indian Psychology, 8(3), 1708-1713. DOI:10.25215/0803.174
- Bhat, B.A., Mir, R.A., Hussain, A. et al.Depressive and anxiety symptoms, quality of sleep, and coping during the 2019 coronavirus disease pandemic in general population in Kashmir. Middle East Curr Psychiatry 27, 61 (2020). https://doi.org/10.1186/s43045-020-00069-2
CrossRef - BuysseDJ, Reynolds CF, 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989; 28:193–213. [PubMed] CrossRef
- Backhaus J, Junghanns K, Broocks A, Riemann D, Hohagen F. Test-retest reliability, and validity of the Pittsburgh Sleep Quality Index in primary insomnia. J Psychosom Res. 2002; 53:737–40.
CrossRef - Blais FC, Gendron L, Mimeault V, Morin CM. Assessment of insomnia: Validation of three questionnaires. Encephale. 1997; 23:447–53.
- Bastien CH, Vallières A, Morin CM. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2001; 2:297–307.
CrossRef - Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, Rubin GJ. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020 Doi: 10.1016/S0140-6736(20)30460-8. [PMC free article] [PubMed] [CrossRef] [Google Scholar] CrossRef
- Celik N, Ceylan B, Unsal A, Çagan O. Depression in health college students: relationship factors and sleep quality. Psychol Health Med. (2019) 24:625–30. DOI: 10.1080/13548506.2018.1546881
CrossRef - Zuki, N. A. M., Azhan, M. A. N., Kamaruddin, H. K., Kassim, A. F. M., Ahmad, M. F., & Bakar, A. H. A. (2021). Sleep Quality Among University Students During Covid-19 Lockdown. International Journal of Academic Research in Progressive Education and Development, 10(2), 814-822.
CrossRef - Levenson, J. C., Shensa, A., Sidani, J. E., Colditz, J. B., & Primack, B. A. (2016). The association between social media use and sleep disturbance among young adults. Preventive Medicine, 85, 36–41. https://doi.org/10.1016/j.ypmed.2016.01.001
CrossRef - Orzech, K. M., Grandner, M. A., Roane, B. M., &Carskadon, M. A. (2016). Digital media use in the 2 h before bedtime is associated with sleep variables in university students. Computers in Human Behavior, 55, 43–50. https://doi.org/10.1016/j.chb.2015.08.049
CrossRef - Cellini N, Canale N, Mioni G, Costa S. Changes in sleep pattern, sense of time and digital media use during COVID-19 lockdown in Italy. J Sleep Res. 2020 Doi: 10.1111/jsr.13074.
CrossRef - Losada-Baltar A, Jiménez-Gonzalo L, Gallego-Alberto L, Pedroso-Chaparro MDS, Fernandes-Pires J, Márquez-González M. “We’re staying at home”. Association of self-perceptions of aging, personal and family resources and loneliness with psychological distress during the lockdown period of COVID-19. J Gerontol B Psychol Sci Soc Sci. 2020 Doi: 10.1093/geronb/gbaa048
CrossRef - Li, Y., Bai, W., Zhu, B. et al.Prevalence and correlates of poor sleep quality among college students: a cross-sectional survey. Health Qual Life Outcomes 18, 210 (2020). https://doi.org/10.1186/s12955-020-01465-2
CrossRef - Cheng SH, Shih CC, Lee IH, Hou YW, Chen KC, Chen KT, Yang YK, Yang YC. A study on the sleep quality of incoming university students. Psychiatry Res. 2012 May 30;197(3):270-4. Doi: 10.1016/j.psychres.2011.08.011. Epub 2012 Feb 18. PMID: 22342120.
CrossRef - Yu Chang, Li Xingxing, Qi Gangqiao, Yang Liang, Fu Wenbo, Yao Qin, Wei Lei, Zhou Dongsheng, Zhang Xiangyang, Zheng Hong. (2021). Prevalence, Risk Factors, and Clinical Correlates of Insomnia in China College Student During the COVID-19. Frontiers in Psychiatry, 12(2021):1375. https://www.frontiersin.org/article/10.3389/fpsyt.2021.694051
CrossRef - Varma, P., Burge, M., Meaklim, H., Junge, M., & Jackson, M. L. (2021). Poor Sleep Quality and Its Relationship with Individual Characteristics, Personal Experiences and Mental Health during the COVID-19 Pandemic. International journal of environmental research and public health, 18(11), 6030. https://doi.org/10.3390/ijerph18116030
CrossRef








