Krishnaveni. C1 , Kiranmayee. P2
, Kiranmayee. P2 , Raghuveer. C. V3*
, Raghuveer. C. V3* , Sheela. S. R4
, Sheela. S. R4 , Kalyani. R3
, Kalyani. R3  and Venkateshu K. V1
and Venkateshu K. V1
1Department of Anatomy, Sri Devaraj Urs Medical College, Sri Devaraj Urs Academy of Higher Education and Research, Tamaka, Kolar, Karnataka, India.
2Department of Cell Biology and Molecular Genetics, Sri Devaraj Urs Medical College, Sri Devaraj Urs Academy of Higher Education and Research, Tamaka, Kolar, Karnataka, India.
3Department of Pathology, Sri Devaraj Urs Medical College, Sri Devaraj Urs Academy of Higher Education and Research, Tamaka, Kolar, Karnataka, India.
4Departments of Obstetrics and Gynaecology, Sri Devaraj Urs Medical College, Sri Devaraj Urs Academy of Higher Education and Research, Tamaka, Kolar, Karnataka, India
Corresponding Author E-mail: krishna.i@hotmail.com
DOI : https://dx.doi.org/10.13005/bpj/2451
Abstract
Preeclampsia (PE) is a multifactorial pregnancy specific disorder with complexity in pathophysiology. Many markers have been evolved but none of them was specific. The aim of the study was to compare the maternal serum soluble endoglin (sEnd) levels in pre-eclamptic & normotensive pregnant women in early and late gestational weeks. A total of 300 subjects were enrolled from the R.L.Jalappa Hospital and Research Centre, Obstetrics & Gynaecology department. In this case-control study design the cases were 150 subjects who were diagnosed as pre-eclamptic women and controls are 150 normotensive pregnant women who are healthy without any complications till delivery. Both in cases and controls the subjects were after 20 weeks of gestation. By taking written informed consent from each participant the 5ml of blood was collected and measured for the estimation of sEnd levels by using commercially available kits. The Area under Receiver Operating Characteristic Curve was calculated by using Statistical Packages for Social sciences Software with values 0.87 with 87% sensitivity and 83% specificity with cut off value ≥ 8 ng/ml. The sEnd levels are significantly increased in preeclamptic women than normotensive pregnant women (P=0.0001).So sEnd can be a diagnostic marker for PE in Kolar population. This is the first south eastern Indian study with 300 sample size.
Keywords
CD105; Hypertensive Pregnancy Disorders; Preeclampsia Antiangiogenic Factors; Pregnancy Diagnostic Marker; Soluble Endoglin
Download this article as:| Copy the following to cite this article: Krishnaveni C, Kiranmayee P, Raghuveer C. V, Sheela S. R, Kalyani R, Venkateshu K. V. Maternal Serum Soluble Endoglin Levels as a biomarker in Preeclampsia: A Case Control Tertiary Care Hospital Based Study. Biomed Pharmacol J 2022;15(2). |
| Copy the following to cite this URL: Krishnaveni C, Kiranmayee P, Raghuveer C. V, Sheela S. R, Kalyani R, Venkateshu K. V. Maternal Serum Soluble Endoglin Levels as a biomarker in Preeclampsia: A Case Control Tertiary Care Hospital Based Study. Biomed Pharmacol J 2022;15(2). Available from: https://bit.ly/3L9jvAC |
Introduction
PE is a multisystemic pregnancy hypertensive syndrome with improper implantation of placenta, and vascular endothelial impairment. The incidence of hypertensive pregnancy disorders in worldwide is 5 to 7% which contribute for the maternal and fetal morbidity and mortality1. PE itself contributes 7 to 10% in maternal and fetal morbidity and mortality2. During pregnancy, the placenta undergoes angiogenesis and vasculogenesis to accommodate fetal demands. Due to defective angiogenesis mechanism there will be imbalance in secretions of placental angiogenesis during placental development, followed by endothelial vascular disorders, hypertension, proteinuria and preeclampsia (PE)1, 3.The pathophysiology of PE was explained as a two‐stage disease. The early-stage: decrease in cytotrophoblastic invasion of uterine spiral arterioles and leads to utero-placental vascular insufficiency. Late-stage: Due to delicate placenta there will be an imbalance in soluble angiogenic factors leads to systemic endothelial dysfunction4. Based on gestational weeks, PE was further classified as early-onset and late onset PE. Early onset PE is which occurs before 34 weeks, due to improper implantation of placenta categorized by placental lesions and diminished in fetal development which leads to fetal and maternal consequences. Whereas late-onset PE occurs on or late 34 weeks but was much related to pre-existing maternal factors like obesity, metabolic syndrome, dyslipidemia but not appreciated with fetal development5. In patching together to PE and angiogenesis, in PE there will be an imbalance in proangiogenic (Placental Inhibitor Growth Factor) and antiangiogenic factors (Soluble Fms Like Tyrosine Kinase-1, Soluble Endoglin factors) in the maternal blood distribution. Endoglin is expressed by placental endothelial cells of chorionic villi (syncytiotrophoblasts) at 11 weeks of gestation 6. Placental Endoglin releases soluble Endoglin into the maternal blood flow. Soluble Endoglin (sEng) is an antiangiogenic, endothelial cell impairment indicator and PE marker with a molecular weight of 180 KD. During gravida status, the vital performance of endoglin in normotensive pregnant women is to control the multiplication, differentiation, incursion of trophoblastic cells to regulate endothelial cell proliferation, and blastocyst implantation. The pathogenesis of PE is associated with placental abnormalities and vascular remodeling. As placental vessels were damaged and by desquamation of membrane-bound sEng isoform transforming growth factor-beta (TGF- β) there will be vasoconstriction. so sEng isoform prevents cell signaling and endothelial function and this results in decreased blood flow and increased levels of sEng6. The over-expressed placental endoglin will be relieving sEng into the maternal circulation7.The released sEng in maternal blood binds with TGF-β (family), by inhibiting the stimulation of endothelial nitric oxide synthase (eNOS) decreases nitric oxide leads to hypoxic conditions. Due to hypoxic environment in the placenta along with increased sEng levels in maternal circulation tempted to effect vascular functioning by increasing in vascular permeability, endothelial dysfunction. The placental hypoxia leads to placental ischemia6. Due to imbalance in the pathway leads to lose control over the trophoblastic invasion of cells and leads to discrepancy which will induce hypertension, which is a cardinal feature in PE 2,7. Due to complexity in PE etiology is imprecise. So many studies have paved a way for different diagnostic markers but none has concluded with specific diagnostic and prognostic markers. So we hypothesized that there will be a relation between increased levels in sEnd to the gestational weeks in maternal serum of normotensive pregnant women and preeclamptic women. In PE or with suspected PE there will be elevated levels of sEnd have been proven by many studies, but with gestational weeks comparison are hardly few studies are there. So this study aim is to compare the maternal serum soluble endoglin (sEnd) levels in pre-eclamptic & normotensive pregnant women in early and late gestational weeks.
Materials and Methods
Study center
This study was conducted in the Sri Devaraj Urs Academy of Higher Education and Research in R.L.Jalappa Hospital and Research Centre in the Department of Obstetrics & Gynaecology. After the doctoral committee approval with the number: SDUAHER/ KLR/ CEC/61/2020-2021, the study subjects were collected along with the written informed consent from each subject.
Study details
In this case-control study, 348 pregnant women were involved, out of these 16% withdrawn from the study. The details were 10% of pregnant women were shifted to their home town for delivery (parents’ house). About 4% of subjects were not concerned to give sample but shared the history and the remaining 2% developed gestational diabetes at late gestational weeks 8.In this study, 150 pregnant women were diagnosed with PE, based on the American College of Obstetrics and Gynaecologists in the Department of Obstetrics & Gynecology in R. L. Jalappa Hospital & Research Centre 8,9. The 150 were cases who were diagnosed as PE and other 150 were controls considered as normotensive pregnant women.
Included in the study
Cases: Pregnant women who were diagnosed with PE ≥ 20th week of gestation, both primigravida and multigravida with early and late gestational weeks of the reproductive age (18-40 years).
Controls: The healthy pregnant women ≥ 20th week of gestation no obstetric and medical complications till delivery, primigravida and multigravida with early and late gestational weeks 8, spontaneous vaginal delivery.
Elimination Measures
Cases: Pregnant women with gestational hypertension, chronic hypertension, gestational diabetes, previous history of more than 2 abortions, previous pregnancy with an anomalous fetus, and thrombophilia like disorders 8.
Methodology: Explained in figure1 8
 |
Figure 1: Sample collection |
Data analysis and Statistical Interpretation
The statistical analysis of data was performed by using Statistical Packages for Social Sciences Software SPSS (version 22.0; SPSS Inc, Chicago, IL, USA). Due to non-distribution in variance, the statistical data (mean, median) was analysed by the Mann-Whitney U test (non-parametric test). The sensitivity (true positive) and specificity (false positive) were interpreted as receiver-operating characteristics of area under curves using SPSS (version 22.0; SPSS Inc, Chicago, IL, USA)
Results
The statistical analysis of samples (cases and controls) were calculated by using the Statistical Packages for Social Sciences software SPSS (version 22.0; SPSS Inc, Chicago, IL, USA). Out of 300 subjects, the pregnant women with early gestational weeks were 46 and late gestation was 254 participants and according to gravida status primigravida were 149 and multigravida were 151, the details were given in Table 1. The severe PE was 68% and the remaining were mild PE described in Table 1. Maternal age, gestational weeks, systolic, and diastolic blood pressures in cases and controls were analyzed by the Mann-Whitney U test explained in Table 2. Due to non-distribution in data, the statistical significance of the maternal sEng levels in cases and controls were analyzed by the non-parametric Mann-Whitney U test explained in Table 3. By comparing cases and controls the maternal serum sEng levels were significantly higher in PE cases (z value =8.71).The p-value is significant with ≤0.0001 especially if we compare with early and late gestational weeks in late gestational weeks the sEng levels were highly significant. The AUC curve value is 0.87 with 89% and 83% sensitivity and specificity were observed with a cut off value of ≥8 ng/ml in Table 3 and figure2. If the value of maternal serum sEnd levels were ≥8 ng/ml are prone to PE. In 52.6% primigravida were PE patients so this reveals PE is more prone to primigravidae. The median values of maternal age in cases and controls there was no much difference between early and late gestation, but in gestational age, we found a difference in late & early PE. In late PE the gestational weeks are 37 and in subjects with early PE were 30 weeks only and if you compare with controls the late gestation extended to 39 weeks. So this proves that due to PE there were more chances of pre-term delivery which affects fetal growth. If we compare the serum sEng levels in early and late PE, in early gestational weeks of PE the serum sEng levels are high in Table 2.
Table 1: Gravida status and gestational weeks of subjects participated in Case – Control study.
| Gravida status | Number of Cases (n=1 50) | Number of Controls (n=150) |
| Primigravida | 79 (52.6%) | 70 (46.6%) |
| Multigravida | 71 (47.3%) | 80 (53.3%) |
| Early Gestation | 36 (24%) | 10 (6.6%) |
| Late Gestation | 114 (76%) | 140 (93.3%) |
| Severe PE | 102 (68%) | ————- |
| Mild PE | 48 (32%) | ————- |
n- Number of subjects, Cases- Preeclamptic pregnant women and Controls – Normotensive pregnant women, PE- Preeclampsia
Table 2: Statistical Outcomes in Early and Late Preeclamptic Women (Cases) vs Early and Late Normotensive Pregnant Women (Controls).
| Content | Gestational Weeks | Median± SE | P value |
| Maternal Age | Early Gestational Weeks in PE cases | 25 ± 0.616 | 0.1336 |
| Early Gestational Weeks in controls | 23 ± 1.13 | ||
| Late Gestational Weeks in PE cases | 24 ± 0.40 | 0.1141 | |
| Late Gestational Weeks in controls | 24 ± 0.267 | ||
| Soluble Endoglin levels | Early Gestational Weeks in PE cases | 31340 ±11180 | *0.00001 |
| Early Gestational Weeks in controls | 640 ± 195 | ||
| Late Gestational Weeks in PE cases | 21270± 1660 | *0.00001 | |
| Late Gestational Weeks in controls | 480 ±85 | ||
| Systolic Blood Pressure | Early Gestational Weeks in PE cases | 160±4.18 |
*0.00001 |
| Early Gestational Weeks in controls | 115±4.216 | ||
| Late Gestational Weeks in PE cases | 110±3.39 | *0.00001 | |
| Late Gestational Weeks in controls | 120±0.757 | ||
| Diastolic Blood Pressure | Early Gestational Weeks in PE cases | 110±3.39 | *0.00001 |
| Early Gestational Weeks in controls | 70 ± 2.62 | ||
| Late Gestational Weeks in PE cases | 100 ± 1.44 | *0.00001 | |
| Late Gestational Weeks in controls | 70 ± 0.586 | ||
| Gestational Age | Early Gestational Weeks in PE cases | 30 ±0.384 | 0.8807 |
| Early Gestational Weeks in controls | 29.5 ±0.87 | ||
| Late Gestational Weeks in PE cases | 37 ± 0.180 | *0.00001 |
*Significant with p value ≤ 0.0001, SE- Standard Error,
Number of subjects involved in the study were as follows:
Early Gestational Weeks in PE cases n=36; Early Gestational Weeks in controls n=10;
Late Gestational Weeks in PE cases n=114; Late Gestational Weeks in controls n=140
Table 3: Angiogenic Marker- Soluble Endoglin Statistical Values.
| Content | Median ± SE | IQ Range | AUC value | Sensitivity | Specificity | Cut -off value | P-value |
| In both cases & controls | 88.25 ± 5.17 | 138-37.25=100.75 | 0.87 | 89% | 83% | pg/ml | U= 4705 Z=8.71 *0.0001 |
| PE | 29.7 ± 5.66 | 160.3 -102 = 58.37 | NA | NA | NA | NA | |
| Controls | 50 ± 8.03 | 81.125-20.87= 60.25 | NA | NA | NA | NA |
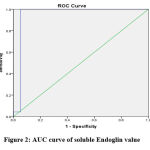 |
Figure 2: AUC curve of soluble Endoglin value |
Discussion
The endoglin function is to maintain vascular tone. Due to PE there will be increased levels of circulating endoglin levels which are associated with vasoconstriction, resulting in decreased blood flow, hints to placental hypoxia leading to placental ischemia which stimulates to release sEnd into the maternal blood flow 6,10,11. The increased concentration of sEnd leads towards placental ischemia eventually leads to endothelial damage. According to Akbar et al in their study mentioned that increased sEnd levels was observed at 12-16 weeks before the onset of PE6. According to the Kosinska-Kaczynska et al in a review stated that sEnd increased levels were significant at 31 to 35 gestational weeks 12. According to the study by Gaber et al concluded that sEnd can be a predictive marker of PE at 15– 18 gestational weeks. If with a cutoff value of >7 ng/ ml, 94% chances are there to develop PE13. In a review piloted by Chen states that the sEnd cut off value ranges from 4.1 to 33 ng/ml 14. The present study results match with Gaber and Chen studies, the cut off values are similar with the present study population. In a study performed by Ali and his colleague’s states that sEnd levels were significant in PE group with mean value 9.1+44.3-171. A study performed in Romania stated that sEnd levels are not so relevant for diagnostic use in PE of Romanian population15. A study with 43 PE women was performed in Brazil found that sEnd levels remained constantly high in severe PE. But in the present study was performed by comparing to gestational ages in PE. In early PE the sEnd concentration levels were significant than late PE, but definitely there was an increase in serum sEnd concentrations between normotensive and PE pregnant women. A study piloted by Hirashima et al on 56 PE women, states that in the early onset of PE the sEnd levels were high compared to late onset of PE. In our study also sEnd levels median ± SE in late onset is 2127± 1660 and in early the onset median ± SE is 3134 ±11180 matches with the present study but with a sample size of 300 pregnant women17. In a study performed by Khalil et al proved that plasma levels of sEnd are a diagnostic marker in late gestational PE18. Another study performed in Indonesian population states that serum sEnd levels are a diagnostic marker in early onset PE6. The sEnd levels were significantly increased in severe PE with AUC of 0.94, a cut-off value of 20.4 and are a noble diagnostic marker in Iranian population for PE19. In the Italian population, a study was performed and states that sEnd levels are significant with AUC 0.88 and no difference in sEnd levels in early & late PE20. In the Egyptian population at 13 weeks of gestation, sEnd levels were increased in high exposure of PE subjects along with early onset PE. In Levine et al studies proved that sEnd levels can be an early investigative indicator in the Egyptian and American populations 21, 22. A study was conducted by Lai et al and their observations revealed that sEnd levels were more significant at early gestational weeks. So the maternal sEnd levels can be an early prognostic marker23. In the Japanese population observed that sEnd levels can be a diagnostic marker in PE with mean significant levels of 60.9 ± 28.8 24. Cui et al piloted a study with 110 PE and 62 normotensive pregnant women observations were increasing sEnd levels are matching with the severity of PE and a similar study results was observed by Venkatesha et al also 25, 26.
From Northern part of India 3 studies were performed and only one study was piloted from southern part of India. Present study is initial study in south eastern part of India with 300 sample size. The details of these studies are as follows: In North India, Sachan et al from Lucknow performed on 30 subjects the study revealed that sEnd is a unique marker to evaluate diagnostic and prognostic accuracy in PE women with cut-off value ≥ 6.26 ng/mL. This present study matches with Sachan et al study by a similar range but in present study the range of sEnd concentration was 8 ng/ml with 300 sample size 27. Duhan et al from Haryana conducted a study on 100 subjects in PE and normotensive pregnant women, sEnd levels range from 2.54 ng/ml to 7.06 ng/ml and the levels were significant in PE. The present study matches with the above studies with cut off value 8 ng/ ml and with more sample size28. In south India, Archana et al from Kanchi Tamil Nadu a study was analyzed on 35 pregnant women with increased serum sEnd levels in late-onset PE29. A study from Chandigarh by Agarwal et al conducted on sEnd levels ranges from 84.9±38.8 vs 13.2 ± 6.3ngml–15. In Plasma s-Eng levels can be a useful predictive & diagnostic marker30.Based on all these studies the present study states, sEnd levels are statistically significant in late PE and if the serum levels are ≥8 ng/ml are prone to PE in south eastern part of India. The north Indian studies from Lucknow & Haryana, a south Indian study from Tamil Nadu states that sEnd is a diagnostic marker in PE. But a change in the present study is with 300 sample size. This stands the first study in south-east part of Karnataka, India.
Conclusion
To conclude sEnd levels were elevated in the PE pregnant women than normotensive pregnant women. If we relate the serum sEnd along with gestational stages of PE, in early stages of PE the maternal serum sEnd secretions were significantly elevated. So it can be used as an early predictor marker. In conclusion the maternal serum sEnd level can be a diagnostic marker for PE, especially in South- East part of Indian -Kolar population.
Acknowledgment
A warm gratitude to Mrs.Jyothi, Mrs.Maya, and other sisters of the OBG department for assisting in completion of this project.
Ethical Clearance
Central Ethics committee of Sri Devaraj Urs Academy of Higher Education and Research Center with No: SDUAHER/KLR/CEC/61/2020-21 in Kolar, Karnataka, India.
Conflict of Interest
None of the authors declare conflict of interest.
Funding Sources
There were no funding sources. It is a self-financed project
References
- Bdolah Y, Sukhatme VP, Karumanchi SA. Angiogenic imbalance in the pathophysiology of preeclampsia: newer insights. Semin Nephrol. 2004; 24(6): 548‐556.
CrossRef - Ali SA, Mohammad AI. Comparative Study between Maternal Serum Level of Soluble Endoglin In The Normal Pregnancy And Those Of The Preeclampsia. 2010; 8(3):229–238.
- Aggarwal PK, Chandel N, Jain V, Jha V. The relationship between circulating endothelin-1, soluble fms-like tyrosine kinase-1 and soluble endoglin in preeclampsia. J Hum Hypertens. 2012; 26(4): 236–241.
CrossRef - Yuan H-T, Haig D, Ananth Karumanchi S. Angiogenic factors in the pathogenesis of preeclampsia. Curr Top Dev Biol. 2005; 71: 297–312.
CrossRef - Valensise H, Vasapollo B, Gagliardi G, Novelli G P. Early and Late Preeclampsia | Early and Late Preeclampsia Two Different Maternal Hemodynamic States in the Latent Phase of the Disease. Hypertension. 2008; 52: 873-880.
CrossRef - Akbar A, Herdiyantini M, Aditiawarman A. Comparison of serum soluble edoglin (sEng) level in eary onset preeclampsia, late onset preeclampsia and normal pregnant woman. Maj Obstet Ginekol. 2018 ; 25(1) :10-15.
CrossRef - Li H, Yao J, Chang X, Wu J, Duan T, Wang K. LIFR increases the release of soluble endoglin via the upregulation of MMP14 expression in preeclampsia. Reproduction. 2018 ; 155(3) : 297–306.
CrossRef - Changalvala.K, Kiranmayee.P, Raghuveer CV, Sheela SR, Venkateshu KV, Kalyani.R. Association of sflt-1 as a maternal serum biomarker in preeclampsia: A case–control tertiary care hospital based study.Indian J Med Sci.2021. doi:10.25259/IJMS-354-2020. (Under press)
CrossRef - March MI, Geahchan C, Wenger J, Raghuraman N, Berg A, Haddow H, et al. Circulating Angiogenic Factors and the Risk of Adverse Outcomes among Haitian Women with Preeclampsia. PLoS ONE. 2015; 10(5): e0126815 [Internet]. [cited 2020 May 25]. Available from: https://www.ncbi.nlm.nih.gov/pmc/ articles/PMC4428697/
CrossRef - Schmella MJ, Roberts JM, Conley YP, Ren D, Storvold GL, Ingles SA et al. Endoglin pathway genetic variation in preeclampsia: A validation study in Norwegian and Latina cohorts. Pregnancy Hypertens. 2018; 12: 144– 149.
CrossRef - Blázquez-Medela, A.M., García-Ortiz, L., Gómez-Marcos, M.A. et al. Increased plasma soluble endoglin levels as an indicator of cardiovascular alterations in hypertensive and diabetic patients. BMC Med. 2010; 8: 86.
CrossRef - Kosinska-Kaczynska K, Zgliczynska M, Kozlowski S, Wicherek L. Maternal Serum Placental Growth Factor, Soluble Fms-Like Tyrosine Kinase-1, and Soluble Endoglin in Twin Gestations and the Risk of Preeclampsia—A Systematic Review. J Clin Med. 2020; 9: 183.
CrossRef - Gaber K, Hamdy E, Hanafy A. Soluble Endoglin as a new marker for prediction of pre-eclampsia in early pregnancy. Middle East Fertil Soc J. 2010; 15: 42–46.
CrossRef - Chen Y. Novel Angiogenic Factors for Predicting Preeclampsia: sFlt-1, PlGF, and Soluble Endoglin. Open Clin Chem J. 2009; 2: 1–6.
CrossRef - Rădulescu C, Bacârea A, Huțanu A, Gabor R, Dobreanu M. Placental Growth Factor, Soluble fms-Like Tyrosine Kinase 1, Soluble Endoglin, IL-6, and IL-16 as Biomarkers in Preeclampsia. Mediators Inflamm.2016; 2016: 1–8.
CrossRef - Perucci LO, Gomes KB, Freitas LG, Godoi LC, Alpoim PN, Pinheiro MB et al. Soluble Endoglin, Transforming Growth Factor-Beta 1 and Soluble Tumor Necrosis Factor Alpha Receptors in Different Clinical Manifestations of Preeclampsia. PLoS ONE. 2014; 9: e97632.
CrossRef - Hirashima C, Ohkuchi A, Matsubara S, Suzuki H, Takahashi K, Usui R et al. Alteration of serum soluble endoglin levels after the onset of preeclampsia is more pronounced in women with early-onset. Hypertens Res Off J Jpn Soc Hyperten.s 2008; 31: 1541–1548.
CrossRef - Khalil A, Maiz N, Garcia-Mandujano R, Elkhouli M, Nicolaides KH. Longitudinal changes in maternal soluble endoglin and angiopoietin-2 in women at risk for pre-eclampsia. Ultrasound Obstet Gynecol. 2014; 44 : 402–410.
CrossRef - Nikuei P , Bandar Abbas, Rajaei M, Malekzadeh K, et al. Accuracy of Soluble Endoglin for Diagnosis of Preeclampsia and its Severity. Iran Biomed J. 2017; 21: 312–320.
CrossRef - De Vivo A, Baviera G, Giordano D, Todarello G, Corrado F, D’anna R. Endoglin, PlGF and sFlt-1 as markers for predicting pre-eclampsia. Acta Obstet Gynecol Scand. 2008; 87: 837–842.
CrossRef - Elhawary T, Demerdash, Elbendary. Maternal serum endoglin as an early marker of pre-eclampsia in high-risk patients. Int J Womens Health. 2012; 4(1): 521-525.
CrossRef - Levine RJ, Yu KF, Sibai BM, Thadhani R. Soluble Endoglin and Other Circulating Antiangiogenic Factors in Preeclampsia. N Engl J Med. 2006; 355(10): 992-1005.
CrossRef - Lai J, Syngelaki A, Poon LCY, Nucci M, Nicolaides KH. Maternal Serum Soluble Endoglin at 30-33 Weeks in the Prediction of Preeclampsia. Fetal Diagn Ther. 2013; 33: 149–155.
CrossRef - Masuyama H, Nakatsukasa H, Takamoto N, Hiramatsu Y. Correlation between Soluble Endoglin, Vascular Endothelial Growth Factor Receptor-1, and Adipocytokines in Preeclampsia. J Clin Endocrinol Metab. 2007; 92: 2672–2679.
CrossRef - Cui L, Shu C, Liu Z, Tong W, Cui M, Wei C et al. Serum protein marker panel for predicting preeclampsia. Pregnancy Hypertens. 2018; 14: 279–285.
CrossRef - Venkatesha S, Toporsian M, Lam C, Hanai J, Mammoto T, Kim YM et al. Soluble endoglin contributes to the pathogenesis of preeclampsia. Nat Med. 2006; 12: 642–649.
CrossRef - Sachan R, Patel M, Dhiman S, Gupta P, Sachan P, Shyam R. Diagnostic and prognostic significance of serum soluble endoglin levels in preeclampsia and eclampsia. Adv Biomed Res. 2016; 5: 119.
CrossRef - Duhan N, Sharma D, Garg N, Dahiya K, Sirohiwal D. Comparative evaluation of serum soluble endoglin level in preeclampsia and normotensive pregnant women. Journal of Physiology and Pathophysiology. 2011; 2 (4): 47-51.
CrossRef - Archana A, Brindha G , Sampson U. Studies on serum soluble endoglin: An indicator for preeclampsia. Int J Clin Biochem Res. 2018; 5: 599–603.
CrossRef - 30. Lopez-Novoa JM. Soluble endoglin is an accurate predictor and a pathogenic molecule in pre-eclampsia. Nephrol Dial Transplant.2007; 22: 712–714.
CrossRef








