Dani Mihir Tusharbhai 1* , Mohan Baliga1
, Mohan Baliga1 , Shaila Kamath2
, Shaila Kamath2  and Aananya Mishra1
and Aananya Mishra1
1Department of Oral and Maxillofacial Surgery, Manipal College of Dental Sciences, Mangalore, Manipal Academy of Higher Education, India.
2Department of Anesthesiology, Kasturba Medical College, Mangalore, Manipal Academy of Higher Education, India.
Corresponding Author E-mail: mihirdani26@gmail.com
DOI : https://dx.doi.org/10.13005/bpj/2428
Abstract
Background: Total intravenous anesthesia (TIVA) is a technique where drugs are administered intravenously for the induction and maintenance of anesthesia instead of volatile drugs, avoiding some of the drawbacks of inhalation anesthesia providing rapid and complete recovery making it suitable for daycare surgeries. Aim: To compare the intraoperative and postoperative hemodynamic patterns, postoperative recovery time, and unwanted consequences such as post-operative nausea and vomiting (PONV) in various maxillofacial procedures using a combination of two drug regimens, namely propofol-ketamine and propofol-fentanyl. Patient & methods: 40 patients between the age group of 18-40 years of either gender were randomly divided into two groups with propofol-ketamine (group 1, n=20) and propofol-fentanyl (group 2, n=20) who underwent various surgical procedures like cyst enucleation, open reduction and internal fixation (ORIF) of facial fractures, orthognathic procedures such as maxillary or mandibular segmental osteotomy and genioplasty with the procedure lasting 60 to 75 minutes. This study compared the total amount of propofol, time of the infusion, and hemodynamic parameters like mean pulse rate (PR), oxygen saturation level (SpO2), systolic blood pressure (SBP) & diastolic blood pressure (DBP), emergence time & recovery time, undesirable sequels like postoperative nausea and vomiting (PONV) and any other side effects between both the groups. Results were analyzed statistically using an independent t-test and chi-square test. Results: A comparison of two groups revealed a significant rise in systolic blood pressure in group 1 as compared to group 2 and group 2 showed better emergence time & recovery time with fewer incidences of postoperative nausea and vomiting and other side effects. Conclusion: Since the propofol-fentanyl provided significantly good results it can be considered as an alternative to gaseous anesthetic agents in various maxillofacial surgical procedures mentioned in the materials with the surgical procedure lasting 60-75 minutes.
Keywords
Fentanyl; Intravenous anesthesia; Ketamine; Maxillofacial Surgical Procedures; Propofol
Download this article as:| Copy the following to cite this article: Tusharbhai D. M, Baliga M, Kamath S, Mishra A. Comparison of Propofol-Fentanyl Versus Propofol-Ketamine Combination as Total Intravenous Anesthesia in Maxillofacial Surgical Procedures – A Prospective Randomized Controlled Study. Biomed Pharmacol J 2022;15(2) |
| Copy the following to cite this URL: Tusharbhai D. M, Baliga M, Kamath S, Mishra A. Comparison of Propofol-Fentanyl Versus Propofol-Ketamine Combination as Total Intravenous Anesthesia in Maxillofacial Surgical Procedures – A Prospective Randomized Controlled Study. Biomed Pharmacol J 2022;15(2). Available from: https://bit.ly/3Ow3bwh |
Introduction
Various Maxillofacial surgeries are executed globally under general anesthesia amid which volatile agents have remained the conventional choice for the maintenance of anesthesia, often imperiled to added stress to the patients, increased side effects, the higher cost feature and uneasiness for the patient. Economic constraints including prolonged hospital stays have encouraged both the surgeons and anesthesiologists for the alteration and improvements in the existing anesthetic procedures. 1
Ever since GA’s establishment in surgery, its recent variation total intravenous anesthesia has undergone lots of evolution. Total intravenous anesthesia (TIVA) is a technique where drugs are administered intravenously instead of volatile drugs. The benefits of TIVA includes it evades several shortcomings of inhalation anesthesia while delivering rapid and painstaking recovery in addition to fewer incidence of post-operative nausea and vomiting (PONV), which makes it convenient for daycare surgeries. It is relatively less noxious and it diminishes the risk of malignant hyperthermia and environmental hazards such as ozone depletion in stratosphere and greenhouse warming in the troposphere. 2,3 As compared to inhalational anesthesia, TIVA has numerous benefits such as no operational room pollution, marginal cardiac depression, minor neuro-humoral response, and reduced oxygen consumption. 4
In the current era, TIVA has added more popularity with the development of newer induction agents, amnestic agents and opioids and along with advances of automated infusion pumps including target-controlled infusion system (TCI) and syringe pumps. 5
Several drugs have been tried in the search for an ideal intravenous drug but none of the single-agent can deliver all properties, hence various combinations of different drugs are advocated to offer balanced in TIVA. 6, 7
This randomized study was aimed to compare and evaluate the combination of two drugs regimen i.e. propofol-ketamine and propofol-fentanyl for total intravenous anesthesia in terms of intraoperative and postoperative hemodynamic profile, postoperative recovery and undesirable sequels like PONV and other side effects in various maxillofacial procedures.
Materials and Methods
After obtaining the ethical committee approval (Ref. No. 17096) a prospective randomized study was carried out from November 2017 to June 2019 in our hospital.
The sample size was calculated using the formula:
With 95% confidence level and 90% power, 40 participants with the age group between 18-40 years were divided into two groups.
Group 1 contained propofol-ketamine (N =20)
Group 2 contained propofol-fentanyl (N =20)
For randomization of the study population, a toss of coin method to decide whether to use group 1 or group 2.
Inclusion criteria consist of patients with American Society of Anesthesiologists (ASA) status I & II, who underwent various maxillofacial procedures such as cystic enucleation (5 patients in each group), open and internal reduction (ORIF) of facial fractures (12 patients in each group) and segmental maxillary or mandibular osteotomy and genioplasty (3 patients in each group) with procedure lasting for 60-75 minutes. Exclusion criteria were patients with a history of allergy to the given drug, patients having immune-compromised state and suffering from cardiovascular disease and renal disease and with obstructive sleep apnea (OSA).
All the patients received tablet pantoprazole 40 mg along with tablet alprazolam 0.25 mg night before and 2 h before as a premedication. After the initial surgical evaluation, all the patients were evaluated by an anesthetist, assessing the patient’s medical condition and nil per oral status. Various monitors were used including a non-invasive blood pressure cuff (NIBP), electrocardiogram leads (ECG), pulse oximeter along with salter nasal cannula, after which initial vital signs were recorded. 18 gauge IV cannula was placed in the hand to obtain intravenous access for infusing drugs and fluid administration. After securing IV line injection midazolam 0.04mg/kg was injected before induction in each group. Induction of anesthesia in group 1 patients was performed with propofol in a dose of 1.0 mg/kg body weight & ketamine in the dose of 1.0 mg/kg body weight as intravenous boluses. While in group 2, it was performed with propofol in the dose of 1.0 mg/kg body weight & fentanyl 2 μg/kg body weights as intravenous boluses.
Injection succinylcholine in the dose of 1.5 mg/kg body weight was injected as a muscle relaxant in both the groups prior to intubation, after which patients were intubated with endotracheal intubation technique. Thereafter hemodynamic parameters were recorded at every 1 minute for the initial 5 minutes. Maintenance of anesthesia in group I was done with propofol in the dose of 2.0 mg/kg/hour & ketamine in the dose of 1.5 mg/kg/hour, while in group II, propofol in the dose of 2.0 mg/kg/hour & fentanyl 1.5 μg/kg/hour were administered for maintenance. Hemodynamic parameters were recorded every 10 minutes until the procedure is completed, with all the patients being ventilated with 100% oxygen. The infused drugs were terminated 5 minutes prior to the end of the surgical procedure. For the reversal of neuromuscular blockade injection neostigmine in the dose of 0.05 mg/kg body weight and injection glycopyrrolate in the dose of 10 μg/kg body weight were injected over duration of 2 to 4 minutes. Extubation was carried out when the patients were able to retain rhythmic respiration & ample tidal volume.
Following Extubation, the patients were asked to open eyes by anesthetist every minute until the patient was able to obey. The time elapsed for the patient to open the eyes after cessation of the infusion was noted as the emergence time. After Extubation, the patients were shifted to post-anesthetic care room where recovery time was recorded along with the physiological parameters were also recorded every 5 minutes up to 20 minutes. Any untoward sequel or any adverse events such as post-operative nausea, vomiting, awareness of procedure or any excitatory movements that occurred in the recovery was recorded and addressed accordingly by the surgeon and the anesthetists. After that patients were given appropriate postsurgical instructions and analgesics were administered as required for pain control.
Results
This study compared the total amount of propofol, time of the infusion, hemodynamic parameters like mean pulse rate (PR), oxygen saturation level (SpO2), systolic blood pressure (SBP) & diastolic blood pressure (DBP), emergence time & recovery time, undesirable sequels like postoperative nausea and vomiting (PONV) and any other side effects between both the groups. 22 males & 18 females belonging to ASA grade I & II in the age group of 18 to 40 years were part of the study & the results obtained were statistically analyzed using SPSS version 17. Statistical analysis was done by independent t-test & Pearson’s chi-squared test.
Comparison of age distribution, time of infusion and total propofol infused in both the group showed statistically no significant difference (Table 1).
Table 1: Comparison of age, average time infusion and total propofol infusion between two groups.
| Parameters | Group | Mean | SD | P Value |
| Age
(Year) |
1 | 35.15 | 8.24 | 0.895 |
| 2 | 35.55 | 10.69
|
||
| Average Infusion
(min)
|
1 | 53.00 | 8.01 | 0.846 |
| 2 | 53.50 | 8.12 | ||
| Total
Propofol (mg) |
1 | 120.00 | 26.75 | 0.735 |
| 2 | 117.50 | 18.88 |
Abbreviations: SD, Standard Deviation; min, minutes; µg, microgram.
Comparison of oxygen saturation level showed higher values in group 2 both preoperatively and intraoperatively, while postoperatively it is higher in group 1. However, there was statistically no significant difference in oxygen saturation level between the 2 groups. (Table 2).
Table 2: Comparison of oxygen saturation of both the groups.
| Variable | Group | Mean | SD | P Value |
| Oxygen Saturation Preoperative | 1 | 98.750 | 1.164 | 0.178 |
| 2 | 99.200 | 0.894
|
||
| Oxygen Saturation Intraoperative | 1 | 99.900 | 0.308 | 0.163 |
| 2 | 100.000 | 0.000
|
||
| Oxygen Saturation
Postoperative |
1 | 99.850 | 0.366 | 1 |
| 2 | 99.850 | 0.489 |
Abbreviations: SD, Standard Deviation
Comparison of SBP between both the groups at pre-induction it was higher in group 1and was statistically non- significant with a P-value of 0.054. From 1 minute (1M) of induction to 20 minutes (20M) intraoperatively shows a statistically highly significant difference with P value ˂ 0.05 with group 2 providing better values. While at 30 and 40 minutes intraoperatively shows no statistically significant difference among the two groups and at 50 minutes the comparison showed a statistically significant difference with P-value 0.013. Also comparing the systolic blood pressure postoperatively showed statistically no significant difference (Graph 1) and (Table 3).
Table 3: Comparison of systolic blood pressure of both the groups at different stages of anesthesia.
| Parameter | GROUP | N | Mean | Std. Deviation | P VALUE |
| Systolic Blood Pressure Pre-induction | GROUP 1 | 20 | 133.750 | 7.461 | 0.054 |
| GROUP 2 | 20 | 129.300 | 6.658 | ||
| Systolic Blood Pressure 1M | GROUP 1 | 20 | 135.700 | 8.603 | 0.007 |
| GROUP 2 | 20 | 128.400 | 7.500 | ||
| Systolic Blood Pressure 2M | GROUP 1 | 20 | 135.250 | 10.721 | 0.009 |
| GROUP 2 | 20 | 126.950 | 8.204 | ||
| Systolic Blood Pressure 3M | GROUP 1 | 20 | 135.700 | 10.367 | 0.009 |
| GROUP 2 | 20 | 128.200 | 5.926 | ||
| Systolic Blood Pressure 4M | GROUP 1 | 20 | 136.000 | 10.084 | 0.006 |
| GROUP 2 | 20 | 128.250 | 5.821 | ||
| Systolic Blood Pressure 5M | GROUP 1 | 20 | 135.350 | 11.944 | 0.018 |
| GROUP 2 | 20 | 127.900 | 5.581 | ||
| Systolic Blood Pressure 10M | GROUP 1 | 20 | 135.250 | 10.939 | 0.006 |
| GROUP 2 | 20 | 126.600 | 7.493 | ||
| Systolic Blood Pressure 20M | GROUP 1 | 20 | 135.100 | 8.717 | 0.037 |
| GROUP 2 | 20 | 130.100 | 5.619 | ||
| Systolic Blood Pressure 30M | GROUP 1 | 20 | 134.600 | 11.330 | 0.114 |
| GROUP 2 | 20 | 130.050 | 5.155 | ||
| Systolic Blood Pressure 40M | GROUP 1 | 20 | 132.550 | 10.039 | 0.358 |
| GROUP 2 | 20 | 130.100 | 6.103 | ||
| Systolic Blood Pressure 50M | GROUP 1 | 16 | 137.560 | 9.838 | 0.013 |
| GROUP 2 | 17 | 129.820 | 6.858 | ||
| Systolic Blood Pressure 60M | GROUP 1 | 10 | 133.500 | 9.925 | 0.448 |
| GROUP 2 | 12 | 130.670 | 7.253 | ||
| Systolic Blood Pressure PO 1M | GROUP 1 | 20 | 135.100 | 8.669 | 0.098 |
| GROUP 2 | 19 | 130.790 | 7.076 | ||
| Systolic Blood Pressure PO 5M | GROUP 1 | 20 | 133.200 | 7.445 | 0.132 |
| GROUP 2 | 20 | 129.300 | 8.535 | ||
| Systolic Blood Pressure PO 10M | GROUP 1 | 20 | 132.700 | 7.767 | 0.094 |
| GROUP 2 | 20 | 128.300 | 8.411 | ||
| Systolic Blood Pressure P0 20M | GROUP 1 | 20 | 129.100 | 8.084 | 0.406 |
| GROUP 2 | 20 | 127.850 | 7.719 |
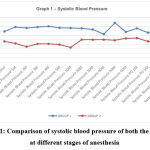 |
Graph 1: Comparison of systolic blood pressure of both the groups at different stages of anesthesia. |
Comparison of DBP between two groups from Pre-induction to 30 minutes (30M) intraoperatively showed statistically no significant difference. While at 40 minutes (40M) comparison shows a statistically significant difference with a P-value of 0.042. Also at 20 minutes postoperatively comparison between two groups shows a statistical difference with a P value of 0.044 (Graph 2) and (Table 4).
Table 4: Comparison of diastolic blood pressure in both the groups.
| Parameter | GROUP | N | Mean | Std. Deviation | P VALUE |
| Diastolic Blood Pressure Pre-induction | GROUP 1 | 20 | 85.850 | 8.580 | 0.295 |
| GROUP 2 | 20 | 88.100 | 3.905 | ||
| Diastolic Blood Pressure 1M | GROUP 1 | 20 | 83.750 | 11.116 | 0.256 |
| GROUP 2 | 20 | 86.950 | 5.316 | ||
| Diastolic Blood Pressure 2M | GROUP 1 | 20 | 86.900 | 9.176 | 0.652 |
| GROUP 2 | 20 | 88.000 | 5.767 | ||
| Diastolic Blood Pressure 3M | GROUP 1 | 20 | 85.750 | 8.168 | 0.399 |
| GROUP 2 | 20 | 87.650 | 5.696 | ||
| Diastolic Blood Pressure 4M | GROUP 1 | 20 | 85.300 | 6.959 | 0.681 |
| GROUP 2 | 20 | 86.100 | 5.119 | ||
| Diastolic Blood Pressure 5M | GROUP 1 | 20 | 86.300 | 9.559 | 0.544 |
| GROUP 2 | 20 | 87.800 | 5.337 | ||
| Diastolic Blood Pressure 10M | GROUP 1 | 20 | 86.750 | 7.745 | 0.246 |
| GROUP 2 | 20 | 89.000 | 3.598 | ||
| Diastolic Blood Pressure 20M | GROUP 1 | 20 | 85.350 | 8.119 | 0.172 |
| GROUP 2 | 20 | 88.250 | 4.447 | ||
| Diastolic Blood Pressure 30M | GROUP 1 | 20 | 84.550 | 9.058 | 0.133 |
| GROUP 2 | 20 | 88.150 | 5.153 | ||
| Diastolic Blood Pressure 40M | GROUP 1 | 20 | 83.800 | 6.354 | 0.042 |
| GROUP 2 | 20 | 87.450 | 4.419 | ||
| Diastolic Blood Pressure 50M | GROUP 1 | 15 | 85.470 | 5.181 | 0.196 |
| GROUP 2 | 17 | 88.060 | 5.815 | ||
| Diastolic Blood Pressure 60M | GROUP 1 | 12 | 86.830 | 6.073 | 0.846 |
| GROUP 2 | 12 | 86.420 | 4.122 | ||
| Diastolic Blood Pressure PO 1M | GROUP 1 | 19 | 86.740 | 5.486 | 0.4 |
| GROUP 2 | 20 | 88.300 | 5.957 | ||
| Diastolic Blood Pressure PO 5M | GROUP 1 | 20 | 86.700 | 4.953 | 0.246 |
| GROUP 2 | 20 | 88.400 | 4.135 | ||
| Diastolic Blood Pressure PO 10M | GROUP 1 | 20 | 85.100 | 4.855 | 0.913 |
| GROUP 2 | 20 | 85.250 | 3.740 | ||
| Diastolic Blood Pressure PO 15M | GROUP 1 | 20 | 83.400 | 3.912 | 0.314 |
| GROUP 2 | 20 | 84.800 | 4.731 | ||
| Diastolic Blood Pressure PO 20M | GROUP 1 | 20 | 80.550 | 3.720 | 0.044 |
| GROUP 2 | 20 | 83.200 | 4.312 |
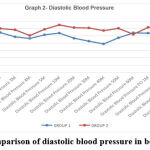 |
Graph 2: Comparison of diastolic blood pressure in both the groups. |
Comparison of the mean pulse rate between the two groups from pre-induction to postoperatively 20 minutes shows a statistically non-significant difference with P value ˂ 0.05 (Graph 3) and (Table 5).
Table 5: Comparison of mean pulse rate between the groups.
| Parameter | GROUP | N | Mean | Std. Deviation | P VALUE |
| Pulse Rate Pre-induction | GROUP 1 | 20 | 81.600 | 8.840 | 0.215 |
| GROUP 2 | 20 | 78.300 | 7.651 | ||
| Pulse Rate 1M | GROUP 1 | 20 | 80.400 | 6.533 | 0.896 |
| GROUP 2 | 20 | 80.700 | 7.855 | ||
| Pulse Rate 2M | GROUP 1 | 20 | 78.700 | 9.493 | 0.329 |
| GROUP 2 | 20 | 81.500 | 8.382 | ||
| Pulse Rate 3M | GROUP 1 | 20 | 78.950 | 10.050 | 0.264 |
| GROUP 2 | 20 | 82.000 | 6.561 | ||
| Pulse Rate 4M | GROUP 1 | 20 | 77.700 | 9.734 | 0.401 |
| GROUP 2 | 20 | 80.000 | 7.226 | ||
| Pulse Rate 5M | GROUP 1 | 20 | 78.700 | 9.565 | 0.603 |
| GROUP 2 | 20 | 80.150 | 7.822 | ||
| Pulse Rate 10M | GROUP 1 | 20 | 79.200 | 9.671 | 0.693 |
| GROUP 2 | 20 | 78.150 | 6.784 | ||
| Pulse Rate 20M | GROUP 1 | 20 | 77.850 | 8.580 | 0.857 |
| GROUP 2 | 20 | 78.300 | 7.079 | ||
| Pulse Rate 30M | GROUP 1 | 20 | 75.700 | 8.323 | 0.731 |
| GROUP 2 | 20 | 76.600 | 8.127 | ||
| Pulse Rate 40M | GROUP 1 | 20 | 74.450 | 7.437 | 0.458 |
| GROUP 2 | 20 | 76.300 | 8.144 | ||
| Pulse Rate 50M | GROUP 1 | 16 | 74.000 | 8.319 | 0.205 |
| GROUP 2 | 16 | 77.440 | 6.572 | ||
| Pulse Rate 60M | GROUP 1 | 10 | 74.400 | 7.749 | 0.752 |
| GROUP 2 | 11 | 75.640 | 9.698 | ||
| Pulse Rate PO 1M | GROUP 1 | 20 | 73.800 | 7.571 | 0.313 |
| GROUP 2 | 20 | 76.200 | 7.274 | ||
| Pulse Rate PO 5M | GROUP 1 | 20 | 71.300 | 7.841 | 0.178 |
| GROUP 2 | 20 | 74.500 | 6.871 | ||
| Pulse Rate PO 10M | GROUP 1 | 20 | 70.600 | 6.524 | 0.208 |
| GROUP 2 | 20 | 73.250 | 6.552 | ||
| Pulse Rate PO 15M | GROUP 1 | 20 | 71.100 | 7.532 | 0.749 |
| GROUP 2 | 20 | 71.800 | 6.135 | ||
| Pulse Rate PO 20M | GROUP 1 | 20 | 70.150 | 7.206 | 0.716 |
| GROUP 2 | 20 | 71.000 | 7.469 |
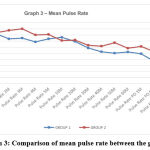 |
Graph 3: Comparison of mean pulse rate between the groups. |
Comparison of emergence time & recovery time between both the groups was done using independent t-test, which showed emergence time and recovery time (in minutes) was higher in group 1 and was statistically non-significant with a P-value of 0.211 and 0.003 (Graph 4).
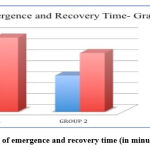 |
Graph 4: Comparison of emergence and recovery time (in minutes) of both the groups. |
Comparison of postoperative incidence of nausea among two groups showed that one patient in group 1 and two patients in group 2 had an incidence of postoperative nausea which is statistically non-significant with a P-value of 0.548. While Comparing the incidence of postoperative vomiting revealed only one patient in group 1 had an incidence of postoperative vomiting which is statistically non-significant while in group 2 none of the patient had an incidence of postoperative vomiting (Table 6).
Table 6: Comparison of post-operative side effects in both the groups.
| Parameters | Group | Absent count | Present count | P value |
| Nausea | 1
2 |
18
19 |
2
1 |
0.548 |
| Vomiting | 1
2 |
19
20 |
1
0 |
0.311 |
| Excitatory Movements | 1
2 |
18
19 |
2
1 |
0.548 |
| Awareness of procedure | 1
2 |
20
20 |
0
0 |
– |
Comparison of postoperative excitatory movements was done using the chi-square test showed 2 patients had an incidence of excitatory movements in group 1 and only 1 patient in group 2 had an incidence of postoperative excitatory movements. The data is statistically non-significant with a P-value of 0.54.Comparison of postoperative awareness between the two groups showed no incidence of postoperative awareness of procedure (Table 6).
Comparison of surgeon satisfaction at the end of the procedure between two groups showed group 1 had a mean value of 7.45 with SD± 0.75 and group 2 had a mean value of 7.95 with SD± 0.82. It is higher in group 2 and was statistically non-significant having P-value of 0.053 (Table 7)
Table 7: Comparison of surgeon’s satisfaction of both the groups.
| Parameter | Group | Mean | SD | P Value |
| Surgeon’s Satisfaction | 1 | 7.450 | 0.759 | 0.053 |
| 2 | 7.950 | 0.826 |
Abbreviations: SD, Standard Deviation
Discussion
Total intravenous anesthesia is evolved in recent years that induces anesthesia, along with amnesia and loss of consciousness for several surgical procedures.8 The accessibility of rapid & short-acting sedative-hypnotic, analgesics & muscle relaxants has refocused the consideration of balanced anesthesia by intravenous route.9Lately TIVA has become more prevalent, beneficial and favorable for two main reasons- the first one is its pharmacokinetics & pharmacodynamics effects of drugs like propofol and recent short-acting various opioids that make it apt for intravenous administration. And the second reason being the newer infusion techniques &latest drug delivery methods like TCI & automated infusion pumps. 10, 11
In the present study two-drug regimen, propofol-ketamine (group 1) and propofol-fentanyl (group 2) for TIVA were compared for a number of maxillofacial surgical procedures. Group 1 showed statistically no significant variation in HR & DBP throughout induction & maintenance of anesthetic procedure in comparison to group 2. But while comparing systolic blood pressure between both the groups statistically significant difference was observed with P values higher in group 1 than group 2.
Comparison of demographic data was quite similar to other studies and doesn’t show any significant difference. The mean duration time for cystic enucleation of jaws was 40-52 minutes, while mean duration time for ORIF was 51-63 minutes and for segmental maxillary and mandibular osteotomy was 58-69 minutes respectively. Our study compared the oxygen saturation between both the groups preoperatively, intraoperatively and postoperatively which showed statistically non-significant, which is clinically relevant as none of our patients had apnea intraoperatively and postoperatively.
A similar study was done where the combination of two drugs viz. propofol-ketamine & propofol-fentanyl as an I.V. anesthesia were compared on 18 patients who undertook non-cardiac surgical procedure, where they observed a decrease in both the SBP & DBP after induction, in patients who received propofol & fentanyl which were very similar to our study. And their results stated as propofol-ketamine as hemodynamically stable drug combination as compared to propofol-fentanyl without the need for additional analgesics. 12
Another study was done where they compared the two-drug combinations using propofol–ketamine & propofol–fentanyl for TIVA on 100 patients with the age group of 20-50 years in patients who underwent elective surgery, where Propofol–fentanyl drug combination resulted in a significantly higher drop in HR (9.28% VS 0.23%) and SBP (7.94% VS 0.12%) and DBP (8.10% VS 0.35%) as compared to propofol–ketamine drug combination. They stated that Propofol–ketamine drug combination resulted in the stable hemodynamic profile during maintenance phase whereas propofol–fentanyl was related with a mild rise in HR and SBP & DBP 13 which in contrast to our study results where propofol-fentanyl combinations showed better hemodynamic stability both during induction and maintenance phase with very fewer side effects.
Comparing the surgeon satisfaction between two groups, showed that group 2 had higher satisfaction scores and ease of performing surgery and there were minimal side effects noted by the operating surgeon with good patient compliance. Whereas comparing the postoperative awareness and excitatory movements between both the groups shows no incidence of postoperative awareness. Moreover out of 40 patients only 2 patients in propofol- ketamine and 1 patient in propofol-fentanyl group had an incidence of excitatory movements.
TIVA can be used in ASA grade I and II without any intra and postoperative complications, however, continuous monitoring of the patient during the entire procedure can be considered as a limitation.
Conclusion
In conclusion we found that propofol-fentanyl combination has the advantage of offering better in terms of hemodynamic stability and postoperative recovery profile along with minimal complications like PONV, awareness of the procedure and excitatory movements with surgeon’s satisfaction in various maxillofacial procedures. Maintaining hemodynamic stability, reducing pain on injection with propofol and preventing PONV, in TIVA technique is a contentious subject and there is no perfect method to reduce it. Propofol-Fentanyl drug combination showed good results. Hence it can be considered as a novel alternative to gaseous anesthetic agents in various maxillofacial surgical procedures lasting 60-75 minutes.
Acknowledgments: None
Conflict of Interest
We have no conflicts of interest.
Funding Sources
There is no funding source.
References
- Bajwa SJ, Sharma V, Sharma R, Singh AP. Anesthesia for day-care surgeries: Current perspectives. Medical Journal of Dr. DY Patil University. 2017 Jul 1;10(4):327.
CrossRef - Morgan M. Total intravenous anaesthesia. Anaesthesia. 1983 Jul;38(S1):1-9.
CrossRef - Regmi NK, Khatri S, Datta PK. Comparison of Propofol-Ketamine Combination with Propofol-Butorphanol Combination for Total Intravenous Anaesthesia on Short Surgical Procedures. Journal of Nepalgunj Medical College. 2014;12(2):34-9.
CrossRef - Robert FJ. Total intravenous anesthesia. Anaesthesiology. 1996;84:149-51.
- Miller RD. Miller’s Anesthesia. In: Kazuhiko Fukuda, editor. Opioids. 7th ed. Churchill Livingstone Elsevier; 2011. pp. 802-3.
- Hernandez C, Parramon F, Garcia-Velasco P, Vilaplana J, García C, Villalonga A. Comparative study of 3 techniques for total intravenous anesthesia: midazolam-ketamine, propofol-ketamine, and propofol-fentanyl. Revista espanola de anestesiologia y reanimacion. 1999 Apr;46(4):154-8.
- Subrahmanyam M, Sreelakshmi B. Comparison of total intravenous anaesthesia using propofol with or without sufentanil in laparoscopic cholecystectomies. Indian journal of anaesthesia. 2009 Aug;53(4):467.
- Rao AR, Kumar SV, Bindu AH. Comparative Study between Propofol and Propofol with Ketamine in Ambulatory Anaesthesia. Journal of Dental and Medical Sciences. 2015 Feb;14(2):1-9.
- Jakobsson J, Davidson S, Andreen M, Westgreen M. Opioid supplementation to propofol anaesthesia for outpatient abortion: a comparison between alfentanil, fentanyl and placebo. Acta anaesthesiologica scandinavica. 1991 Nov;35(8):767-70.
CrossRef - Al-Rifai Z, Mulvey D. Principles of total intravenous anaesthesia: basic pharmacokinetics and model descriptions. Bja Education. 2016 Mar 1;16(3):92-7.
CrossRef - Puri GD. Target controlled infusion total intravenous anaesthesia and Indian patients: Do we need our own data?. Indian journal of anaesthesia. 2018 Apr;62(4):245.
CrossRef - Guit JB, Koning HM, Coster ML, Niemeijer RP, Mackie DP. Ketamine as analgesic for total intravenous anaesthesia with propofol. Anaesthesia. 1991 Jan;46(1):24-7.
CrossRef - Bajwa SJ, Bajwa SK, Kaur J. Comparison of two drug combinations in total intravenous anesthesia: Propofol–ketamine and propofol–fentanyl. Saudi journal of anesthesia. 2010 May;4(2):72.
CrossRef