Ibrahim Hani Hussein* , Abbas Ali Mansour
, Abbas Ali Mansour , Hussein Ali Nwayyir
, Hussein Ali Nwayyir , Ammar Mohammed Saeed Abdullah Almomin
, Ammar Mohammed Saeed Abdullah Almomin , Nassar Taha Yaseen Alibrahim
, Nassar Taha Yaseen Alibrahim , Haider Ayad Alidrisi
, Haider Ayad Alidrisi , Dheyaa Kadhim Jabbar Al-Waeli
, Dheyaa Kadhim Jabbar Al-Waeli , Ibrahim Abbood Zaboon
, Ibrahim Abbood Zaboon , Rudha Naser Hussein
, Rudha Naser Hussein , Adel Gassab Mohammed
, Adel Gassab Mohammed , Muayad Baheer Kadhim
, Muayad Baheer Kadhim and Ali Hussain Ali Alhamza
and Ali Hussain Ali Alhamza
Faiha Specialized Diabetes, Endocrine and Metabolism Center (FDEMC), College of Medicine, University of Basrah, Basrah, Iraq.
Corresponding Author E-mail: ibrahim.hani@fdemc.iq
DOI : https://dx.doi.org/10.13005/bpj/2317
Abstract
Background: People from our region need a higher dose of vitamin D to maintain their serum 25(OH)D levels at concentrations greater than 20 ng/mL. This study aimed to obtain real data on vitamin D status in Basrah. Methods: Retrospective data analysis of patients seen over 2 years from May 2017 to the end of May 2019 at the Faiha Specialized Diabetes, Endocrine and Metabolism Centre (FDEMC) in Basrah, a tertiary referring center of southern Iraq. Results: The cohort included 3692 persons. Vitamin D deficiency was evident among 62.5% of the studied persons (66.5% of women and 48.7% of men). Univariate analysis for factors associated with vitamin D deficiency found it was significantly associated with female sex (OR, 2.095; 95% CI, 1.793 to 2.448; P<0.0001), age less than 44 years (OR, 2.6; 95% CI, 2.328 to 3.065; P<0.0001), nonmarried status (including single, widow and divorced) (OR, 0.768; 95% CI, 0.656 to 0.900; P<0.0001), nulliparous or unmarried status (OR, 0.684; 95% CI, 0.583 to 0.803; P<0.0001), housewife status (OR, 0.806; 95% CI, 0.673 to 0.967; P=0.020), and rural status (OR, 1.195; 95% CI, 1.034 to 1.382; P=0.016). No significant association was found between vitamin D deficiency and BMI. In multivariate logistic regression analyses, only female sex (OR, 0.513; 95% CI, 0.437 to 0.603; P<0.0001) and age less than 44 years (OR, 2.662; 95% CI, 2.252 to 3.147; P<0.0001), nulliparous or unmarried (OR, 0.814; 95% CI, 0.680 to 0.973; P=0.024) and rural residency (OR, 0.773; 95% CI, 0.647 to 0.924; P<0.0001) remained significantly associated. Conclusion: Women, a younger age, nulliparous, and a rural residency were associated with vitamin D deficiency.
Keywords
Adults; Iraq; Vitamin D status
Download this article as:| Copy the following to cite this article: Hussein I. H, Mansour A. A, Nwayyir H. A, Almomin A. M. S. A, Alibrahim N. T. Y. Alidrisi H. A, Al-Waeli D. K. J, Zaboon I. A, Hussein R. N, Mohammed A. G, Kadhim M. B, Alhamza A. H. A. Real-Life Data on Total Vitamin D3 (25-Hydroxyvitamin D) Concentrations in Basrah, Iraq. Biomed Pharmacol J 2021;14(4) |
| Copy the following to cite this URL: Hussein I. H, Mansour A. A, Nwayyir H. A, Almomin A. M. S. A, Alibrahim N. T. Y. Alidrisi H. A, Al-Waeli D. K. J, Zaboon I. A, Hussein R. N, Mohammed A. G, Kadhim M. B, Alhamza A. H. A. Real-Life Data on Total Vitamin D3 (25-Hydroxyvitamin D) Concentrations in Basrah, Iraq. Biomed Pharmacol J 2021;14(4). Available from: https://bit.ly/3BFtY37 |
Introduction
Vitamin D is no longer considered a pure nutritional supplement involved only in bone and calcium metabolism. It is also clearly involved in the pathogenesis of many diseases, although it is not a single causative factor of any.1
There is a high but silent prevalence of vitamin D deficiency in the Middle East/North Africa, the MENA WHO region. People from this area need a higher dose of vitamin D to maintain their serum 25(OH)D levels at more than 20 ng/mL, which is the minimal level of vitamin D accepted by western countries.(2) For that reason, experts recommend higher doses of vitamin D supplements, up to 1000–2000 IU/d, to overcome this state of hypovitaminosis D.2, 3
Increasing dietary intake of fortified foods with adequate sun exposure is a recommendation by the local health authorities in the Gulf region to compensate for the problem of vitamin D deficiency in that area.3 Unfortunately, there are many problems with the standardization of the assays of serum vitamin D and the cut-off levels defined as vitamin D deficiency.4
This study aimed to obtain real data on vitamin D status in Basrah.
Methods
Setting
Retrospective data analysis of patients seen over 2 years from May 2017 to the end of May 2019 at the Faiha Specialized Diabetes, Endocrine and Metabolism Center (FDEMC) in Basrah, a tertiary referring center of from southern Iraq. The study was approved by the Ethical Committee of Faiha Specialized Diabetes, Endocrine and Metabolism Center (FDEMC) with a reference number 56/35/22 in 19/03/2017.
Participants
Inclusion criteria: non-pregnant adults who are apparently healthy and undergoing screening for diseases at the center.
Exclusion criteria: Pregnant or lactating women, age under 18 years, estimated GFR <60, those known to have childhood rickets, osteomalacia or malabsorption, and patients with any bone fracture at any time in life.
For each patient, a blood sample was taken and 5 cc of blood was placed in a tube with a gel activator for immediate centrifugation, and the vitamin D assay was performed within 2 hours of blood sampling.
Vitamin D assay
Serum 25(OH)D concentrations were assayed by a Cobas e411 (Roche Diagnostics GmbH, Mannheim, Germany) using the principle of electrochemiluminescence (Roche ELECSYS). The total vitamin D measuring range was 3.00–700 ng/mL, with an intraassay precision of 0.5 and 0.7 ng/mL SD and 5, 3, 2.5, and 1.7% CV. The interassay precision was ≤ 1.7 ng/mL SD < 11.5% CV. The assay was performed on the platform according to the manufacturer’s recommendations. Vitamin D sufficiency was defined as serum 25-hydroxyvitamin D (25(OH)D) ≥ 30 ng/mL, vitamin D insufficiency 20–29.9 ng/mL, vitamin D deficiency < 20 ng/mL, and severe vitamin D deficiency < 12 ng/mL.4-7
Statistical analysis
Data were entered an Excel sheet and then into IBM SPSS version 25 for Windows. Data are expressed as percentages or means ± SDs. The analysis was performed with χ2 tests. Binary logistic regression analysis was used to identify variables that were independently associated with vitamin D deficiency. Vitamin D sufficiency and insufficiency were considered as one group, and vitamin D deficiency was considered as the second group for comparison. The independent variables used in this study were sex, age less than or greater than 44 years, marital status (married or not, which includes single, widowed and divorced), parity (divided into parous women who previously gave birth and those who never have), residency (rural or urban), occupation (employed, housewife, retired, self-employed and student) and for women (housewife or not), and BMI (less than, equal to, or greater than 25 kg/m2).
Results
Baseline characteristics are presented in Table 1. The cohort involved 3692 persons. The mean age for the whole study was 43.9±14.8 years (42.9±14.7 years for women and 47.4±14.7 years for men). Women constituted 77.1% (2848 patients) of this cohort. The majority of women were housewives (74.2%). Most of the persons were married (75.5%), and 68.4% were from urban Basrah.
Table 1: Baseline characteristics.
| Variables | Women No. (%) 2848(77.1%) | Men No. (%)
844(22.9%) |
Total No. (%) =3692(100%) | |
| Age (years) mean ±SD | 42.9±14.7 | 47.4±14.7 | 43.9±14.8 | |
| Occupation | Employed | 541(19.0) | 383(45.4) | 924(25.0) |
| Housewife | 2114(74.2) | NA | 2114(57.3) | |
| Retired | 37(1.3) | 115(13.6) | 152(4.1) | |
| Self employed | 25(0.9) | 267(31.6) | 292(7.9) | |
| Student | 131(4.6) | 23 (2.7) | 154(4.2) | |
| Unemployed | 0(0.0) | 56 (6.6) | 56(1.5) | |
| Marital state | Married | 2054(72.1) | 734(87.0) | 2788(75.5) |
| Single | 467(16.4) | 93 (11.0) | 560(15.2) | |
| Widow | 262(9.2) | 11(1.3) | 273(7.4) | |
| Divorced | 65(2.3) | 6 (0.7) | 71(1.9) | |
| Residency | Urban | 1941(68.2) | 584(69.2) | 2525 (68.4) |
| Rural | 907(31.8) | 260(30.8) | 1167 (31.6) | |
Vitamin D deficiency was evident among 62.5% of the studied persons. Approximately 66.5% of women (1895/2848) and 48.7% of men (411/844) had a P value <0.001, as shown in Table 2 and Figure 1.
Table 2: Factors associated with vitamin D deficiency among 3692 persons.
| Variables | Vitamin D status | Total | P Value | |||
| Vitamin D sufficiency n=969
|
Vitamin D insufficiency
n=417 |
Vitamin D deficiency
n=2306 |
3692 | |||
| Gender | Women n (%) | 639(22.4) | 314 (11.0) | 1895(66.5) | 2848(100) | <0.001 |
| Men n (%) | 330(38.6) | 103 (12.2) | 411 (48.7) | 844(100) | ||
| Age years | Age less than 44 years n (%) | 282(15.7) | 186 (10.4) | 1329 (74) | 1797 (100) | <0.001 |
| Age 44 years and more n (%) | 687(36.3) | 231 (12.2) | 977 (51.6) | 1895(100) | ||
| Marital status | Married | 785 (27.2) | 330(11.8) | 1700(61.0) | 2788 (100.0) |
<0.001 |
| Single | 87(15.5) | 55(9.8) | 418 (74.6) | 560 (100.0) | ||
| Widow | 105(38.5) | 25(9.2) | 143(52.4) | 273(100.0) | ||
| Divorced | 19(26.8) | 7(9.9) | 45 (63.4) | 71(100.0) | ||
| Parity
|
Parous women | 425(26.2) | 176(10.9) | 1021(62.9) | 1622 (100) | <0.001 |
| Nulliparous or not married | 214 (17.2) | 183(11.3) | 874(71.3) | 1226 (100) | ||
| Residency | Rural | 282 (24.1) | 124 (10.6) | 762 (65.3) | 1167(100.0) | 0.052 |
| Urban | 688(27.3) | 293 (11.6) | 1544(61.1) | 2525(100.0) | ||
| Occupation | Employed | 244 (26.4) | 121 (13.1) | 559(60.5) | 924(100) | <0.001 |
| Housewife | 502 (23.7) | 231(10.9) | 1381(65.3) | 2114(100.0) | ||
| Retired | 84 (55.3) | 21 (13.8) | 47(30.9) | 152 (100.0) | ||
| Self employed | 117(40.1) | 36(12.3) | 139 (47.6) | 292 (100.0) | ||
| Student | 16(10.4) | 6(3.9) | 48(85.7) | 154 (100.0) | ||
| Unemployed | 6(10.4) | 2(3.9) | 48(85.7) | 56(100.0) | ||
| BMI kg/m2 | less than 25 | 152(27.5) | 59(10.7) | 341(61.8) | 552(100.0) | 0.620 |
| 25 and above | 482(26.4) | 197(12.2) | 996(61.4) | 1621(100.0) | ||
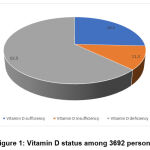 |
Figure 1: Vitamin D status among 3692 persons |
Vitamin D insufficiency was observed in 11.3%, approximately 11.0% of women (314/2848) and 12.2% of men (103/844).
Vitamin D sufficiency was seen in 26.2% (among them, 22.4% were women [639/2848], and 39.0% were men [330/844]).
Severe deficiency (level < 12 ng/mL) was seen among 1133/3692 (30.6%) patients in this cohort.
Most vitamin D deficiency was seen in patients aged less than 44 years vs. those aged 44 years and older (73.8% vs. 51.5%) with a P value <0.001.
There was no statistically significant difference between vitamin D deficiency among overweight or obese persons (although there were 1519 (41.1%) patients with missed BMI data).
Among single persons and married individuals, 74.6% (418/560) and 61.0% (1700/2788) had vitamin D deficiency, respectively (P value <0.001).
Nulliparous or unmarried women were more likely to have vitamin D deficiency in 71.3% (874/1226) vs. 62.9% (1021/1622) of parous women.
Among students and housewives, vitamin D deficiency was seen among 85.7% and 65.2%, respectively.
There was no difference in vitamin D deficiency among those living in rural or urban areas (65.1% vs 61.1%).
Univariate analysis for factors associated with vitamin D deficiency (Table 3) was conducted. It was significantly associated with women (OR, 2.095; 95% CI, 1.793 to 2.448; P<0.0001), age less than 44 years (OR, 2.6; 95% CI, 2.328 to 3.065; P<0.0001), nonmarried (including single, widow and divorced) (OR, 0.768; 95% CI, 0.656 to 0.900; P<0.0001), nulliparous or unmarried (OR, 0.684; 95% CI, 0.583 to 0.803; P<0.0001), housewife (OR, 0.806; 95% CI, 0.673 to 0.967; P=0.020), rural (OR, 1.195; 95% CI, 1.034 to 1.382; P=0.016). No significant association was found between vitamin D deficiency and BMI.
Table 3: Univariate factors associated with vitamin D deficiency among 3692 persons.
|
Variables |
P Value | |||||
| Vitamin D deficiency=2306 | No vitamin D deficiency=1386 | Odd ratio | 95%Confidence interval | |||
| Gender | Women n (%) | 1895(66.5)
|
953(33.5)
|
2.095
|
1.793-2.448
|
<0.0001 |
| Men n (%) | 411(48.7) | 433(51.3) | ||||
| Age
|
Age less than 44 years n (%) | 1329(74.0) | 468(26.0) | 2.6
|
2.328-3.065
|
<0.0001 |
| Age 44 years and more n (%) | 977(51.6) | 918 (48.4) | ||||
| Marital status
|
Married | 1700(61.0) | 1088(39.0) | 0.768 | 0.656-0.900 | <0.0001 |
| Non-married | 606(67.0) | 298(33.0) | ||||
| Parity
|
Parous women | 1021(62.9) | 601(37.1) | 0.684 | 0.583-0.803
|
<0.0001 |
| Nulliparous or not married | 874(71.3) | 352(28.7) | ||||
| Occupation
|
Housewife | 1381 (65.3) | 733 (34.7) | 0.806
|
0.673-0.967
|
0.020
|
| Non- housewife | 514(70.0)
|
220(30.0) | ||||
| Residency | Rural | 761 (65.2) | 406 (34.8) | 1.195
|
1.034-1.382
|
0.016
|
| Urban | 1544 (61.1) | 981(38.9) | ||||
| BMI kg/m2
(BMI2) |
Less than 25 | 341(25.5) | 211(25.2) | 1 | 0.831-1.237 | 0.890
|
| 25 and above | 996(61.6) | 625(38.4) | ||||
Factors significantly associated with vitamin D deficiency on univariate analysis were entered multivariate logistic regression analysis. Only female sex (OR, 0.513; 95% CI, 0.437 to 0.603; P<0.0001), age less than 44 years (OR, 2.662; 95% CI, 2.252 to 3.147; P<0.0001), nulliparity or unmarried status (OR, 0.814; 95% CI, 0.680 to 0.973; P=0.024) and rural residency (OR, 0.773; 95% CI, 0.647 to 0.924; P<0.0001) remained significantly associated.
Table 4: Binary logistic regression analyses of the association between vitamin D deficiency
|
|
Odds Ratio | (95% CI) | P |
| Women | 0.513 | 0.437-0.603 | <0.0001 |
| Age less than 44 years | 2.662 | 2.252-3.147 | <0.0001 |
| Non-married | 1.122 | 0.925 -1.361 | 0.244 |
| Nulliparous or not married | 0.814 | 0.680- 0.973 | 0.024 |
| Housewife | 0.933 | 0.768 -1.134 | 0.485 |
| Rural | 0.773 | 0.647- 0.924 | 0.005 |
Discussion
This study represents a good sample for the study of vitamin D status in Basrah. More than 60% were found to have vitamin D deficiency, and it was more prevalent in women than men. Vitamin D deficiency among adults in the Middle East and North Africa (MENA) region is scattered across a wide range between 44 and 96% according to previous studies.2
There are few data on the vitamin D status in the Iraqi population. One study involved a highly selective fibromyalgia group of patients from Basrah, where vitamin D deficiency reached 95% among 160 patients.8 In Babylon, a district in the middle of Iraq, vitamin D deficiency reached 76% among 500 women with severe vitamin D deficiency (<10 ng/mL) found in 19.6%.9
This prevalence of vitamin D deficiency is similar to that of Saudi Arabia.10 In UAE, among 12,346 participants, vitamin D deficiency was observed in 72%.11 In one Jordanian study, vitamin D deficiency was seen in 89.7%.12 Among 960 adult Kuwait persons, vitamin D deficiency was seen in 27%.13 Iran has a prevalence of vitamin D deficiency of 56%.14
Severe vitamin D deficiency (level < 12 ng/mL) was seen in 30.7% of patients in this study cohort, while it was found in 14.1% of people in Qatari, and more than 10% of Europeans.4, 15
Women had a far higher prevalence of vitamin D deficiency than men (66.5% vs 48.7%) in this study. Similar findings were observed in Qatar, Egypt, Saudi Arabia, Jordan and Iran, China, but in the UAE, vitamin D deficiency was equally seen between men and women. 11, 12, 14-17
We found that patients aged less than 44 years in this study were more likely to have vitamin D deficiency. Similar findings were observed in Jordan, Qatar, Egypt, the UAE and China.11, 12, 15-17
Nulliparity or not married status was associated with vitamin D deficiency in our study. This finding was also seen in Jordan and has been attributed to the fact that parous women will more frequently leave their homes.18
We noticed that living in rural areas was a risk factor for vitamin D deficiency. The same finding was observed in Tianjin residents in China.17 This is the opposite of what is seen in Jordan. 18
Study limitations: Wearing hijabs for religious or cultural reasons and their relationship to vitamin D deficiency needs to be studied in the future.
We considered both vitamin D insufficiency and vitamin D sufficiency as normal vitamin D states in this study, based on the recommendations of others.(3)
Conclusion
Women aged less than 44 years, nulliparous or unmarried women, and rural residency were significantly associated with vitamin D deficiency.
Acknowledgments
The authors acknowledge the invaluable assistance of the medical staff of FDEMC.
Conflict of Interest
None.
Funding Source
No current external funding source for this study.
References
- Park JE, Pichiah PBT, Cha YS. Vitamin D and Metabolic Diseases: Growing Roles of Vitamin D. J Obes Metab Syndr. 2018;27(4):223-32. https://doi.org/10.7570/jomes.2018.27.4.223
CrossRef - Chakhtoura M, Rahme M, Chamoun N, El-Hajj Fuleihan G. Vitamin D in the Middle East and North Africa. Bone Rep. 2018;8:135-46. https://dx.doi.org/10.1016%2Fj.bonr.2018.03.004
CrossRef - Al Saleh Y, Beshyah SA, Hussein W, Almadani A, Hassoun A, Al Mamari A, et al. Diagnosis and management of vitamin D deficiency in the Gulf Cooperative Council (GCC) countries: an expert consensus summary statement from the GCC vitamin D advisory board. Arch Osteoporos. 2020;15(1):35 https://doi.org/10.1007/s11657-020-0709-8.
CrossRef - Lips P, Cashman KD, Lamberg-Allardt C, Bischoff-Ferrari HA, Obermayer-Pietsch B, Bianchi ML, et al. Current vitamin D status in European and Middle East countries and strategies to prevent vitamin D deficiency: a position statement of the European Calcified Tissue Society. Eur J Endocrinol. 2019;180(4):P23-P54. https://doi.org/10.1530/EJE-18-0736
CrossRef - Holick MF, Binkley NC, Bischoff-Ferrari HA, Gordon CM, Hanley DA, Heaney RP, et al. Guidelines for preventing and treating vitamin D deficiency and insufficiency revisited. J Clin Endocrinol Metab. 2012;97(4):1153-8. https://doi.org/10.1210/jc.2011-2601
CrossRef - Perez-Barrios C, Hernandez-Alvarez E, Blanco-Navarro I, Perez-Sacristan B, Granado-Lorencio F. Prevalence of hypercalcemia related to hypervitaminosis D in clinical practice. Clin Nutr. 2016;35(6):1354-8. https://doi.org/10.1016/j.clnu.2016.02.017
CrossRef - Medicine Io. Dietary Reference Intakes for Calcium and Vitamin D. Ross AC, Taylor CL, Yaktine AL, Del Valle HB, editors. Washington, DC: The National Academies Press; 2011. 1132 p. https://doi.org/10.17226/13050
CrossRef - Aldaoseri HA, Zubairi MB. Vitamin D deficiency and treatment in Iraqi patients with primary fibromyalgia syndrome. The Egyptian Rheumatologist. 2020;42(1):47-50. https://doi.org/10.1016/j.ejr.2019.05.002
CrossRef - Mahdi M, Hantoosh H, Imran B, Yahya A. Prevalence of vitamin D deficiency in Iraqi female at reproductive age. Medical Journal of Babylon. 2019;16(2). http://www.medjbabylon.org/text.asp?2019/16/2/119/260474
CrossRef - Al-Alyani H, Al-Turki HA, Al-Essa ON, Alani FM, Sadat-Ali M. Vitamin D deficiency in Saudi Arabians: A reality or simply hype: A meta-analysis (2008-2015). J Family Community Med. 2018;25(1):1-4. https://dx.doi.org/10.4103%2Fjfcm.JFCM_73_17
- Al Zarooni AAR, Al Marzouqi FI, Al Darmaki SH, Prinsloo EAM, Nagelkerke N. Prevalence of vitamin D deficiency and associated comorbidities among Abu Dhabi Emirates population. BMC Research Notes. 2019;12(1):503. https://doi.org/10.1186/s13104-019-4536-1
CrossRef - El-Khateeb M, Khader Y, Batieha A, Jaddou H, Hyassat D, Khawaja N, et al. Vitamin D deficiency and associated factors in Jordan. SAGE Open Medicine. 2019;7:2050312119876151. https://doi.org/10.1177%2F2050312119876151
CrossRef - Zhang FF, Al Hooti S, Al Zenki S, Alomirah H, Jamil KM, Rao A, et al. Vitamin D deficiency is associated with high prevalence of diabetes in Kuwaiti adults: results from a national survey. BMC Public Health. 2016;16:100. https://doi.org/10.1186/s12889-016-2758-x
CrossRef - Vatandost S, Jahani M, Afshari A, Amiri MR, Heidarimoghadam R, Mohammadi Y. Prevalence of vitamin D deficiency in Iran: A systematic review and meta-analysis. Nutrition and health. 2018:260106018802968. https://doi.org/10.1177/0260106018802968
CrossRef - Zainel A-JAL, Qotba H, Al Nuaimi A, Syed M. Vitamin D status among adults (18–65 years old) attending primary healthcare centres in Qatar: a cross-sectional analysis of the Electronic Medical Records for the year 2017. BMJ Open. 2019;9(8):e029334. http://dx.doi.org/10.1136/bmjopen-2019-029334
CrossRef - Botros R, Al SH, Mansour H, Guirgis M. High prevalence of severe vitamin D deficiency in Egyptian females. Endocrine Abstracts. 2019. https://doi.org/10.1530/endoabs.63.P473
CrossRef - Fang F, Wei H, Wang K, Tan L, Zhang W, Ding L, et al. High prevalence of vitamin D deficiency and influencing factors among urban and rural residents in Tianjin, China. Archives of Osteoporosis. 2018;13(1):64. https://doi.org/10.1007/s11657-018-0479-8
CrossRef - Nichols EK, Khatib IM, Aburto NJ, Sullivan KM, Scanlon KS, Wirth JP, et al. Vitamin D status and determinants of deficiency among non-pregnant Jordanian women of reproductive age. Eur J Clin Nutr. 2012;66(6):751-6. https://doi.org/10.1038/ejcn.2012.25
CrossRef








