Department of Basic Medical sciences, Lecturer in Pharmacology, Dar Al Uloom University, Riyadh, KSA.
DOI : https://dx.doi.org/10.13005/bpj/2282
Abstract
Introduction Polypharmacy is most commonly defined as the use of five or more medications daily by an individual. In India, the prevalence of polypharmacy varies from 5.82 % to 93.14% in different states. Concerns about polypharmacy include increased adverse drug reactions, drug interactions, prescribing cascade, and higher costs. Methods It is a non-interventional, observational, descriptive study carried out in 240 patients attending the medicine outpatient department of a tertiary care hospital, over a one-and-a-half-year duration. Results The study was carried out in 240 patients whose mean age was 53.97 ± 7.62 years, out of which 52.5% were male and 47.5% were female. 62% of the study population were from low socioeconomic status and 38 % were from the middle class. The mean duration in years for hypertension and diabetes was 7.1± 4.3years and 7.94+ 4.66 years respectively. Apart from various antihypertensive and antidiabetic medicines prescribed the study population was also prescribed Vitamins (51.6%), Hypolipidemics (42.5%), Miscellaneous (41.6%), Antiplatelets (40%), H2 blockers/PPI (35.8%), and Antibiotics (22.5%). Polypharmacy (5 or more than 5 drugs) was seen in 33.75% of the study population. Conclusion Polypharmacy has been found to be integral in patients suffering from hypertension with coexisting diabetes mellitus and other comorbidities. It is essential to practice judicious prescribing especially in patients with multiple conditions.
Keywords
Adverse effects; Comorbidities; Drug prescription; Multiple drugs
Download this article as:| Copy the following to cite this article: Khan S. Z. A Study of Polypharmacy in Patients with Co-Existing Diabetes Mellitus Type II and Hypertension in a Tertiary Care Center.Biomed Pharmacol J 2021;14(4). |
| Copy the following to cite this URL: Khan S. Z. A Study of Polypharmacy in Patients with Co-Existing Diabetes Mellitus Type II and Hypertension in a Tertiary Care Center.Biomed Pharmacol J 2021;14(4). Available from: https://bit.ly/3nlArKv |
Introduction
Polypharmacy is most commonly defined as the use of five or more medications daily by an individual. Some studies also generally define polypharmacy as the use of multiple concurrent medications or simultaneous long-term use of different drugs by the same individual.1 In India, the prevalence of polypharmacy varies from 5.82 % to 93.14% in different states, the highest being in Uttaranchal and least in West Bengal.2 India bearing the dubious distinction of being the diabetes capital of the world according to the Diabetes Foundation of India, the number of people with diabetes mellitus in India are 62 million, which is set to rise to 79.4 million by 2030.3 Globally 50 % of the population with diabetes mellitus have co-existing hypertension. The co-existence of diabetes mellitus and hypertension is also important as they are multiplicative risk factors for macro and microvascular diseases, resulting in increased risks of cardiac death, coronary artery disease, congestive cardiac failure, cerebrovascular disease, and peripheral vascular disease. To tackle the complications of diabetes mellitus type II and hypertension, additional drugs are prescribed leading to polypharmacy. Between the determinants of polypharmacy increased age was highlighted as a major one, as aging is characterized by the presence of multiple independent chronic diseases in the same person, a fact that is almost always accompanied by multiple drug use.4 Concerns about polypharmacy include increased adverse drug reactions, drug interactions, prescribing cascade, and higher costs.5 Polypharmacy is often associated with a decreased quality of life, including decreased mobility and cognition especially in the elderly.6 Periodic evaluation of polypharmacy studies needs to be carried out to enable suitable modifications in the prescription of drugs to increase the therapeutic benefit and decrease the adverse effects of this concoction of medicines. This study aims to analyze the polypharmacy in patients with co-existing diabetes mellitus type II and hypertension in a tertiary care center.
Material and Methods
Source of data
Patients with co-existing hypertension and diabetes mellitus attending the medicine department of Owaisi Hospital and Research center. (OHRC) Hyderabad.
Inclusion Criteria
Patients with co-existing hypertension and diabetes mellitus type II (with or without associated chronic complications).
Patient who gave informed consent.
Patients of 40-70 years age group of either sex.
Exclusion Criteria
Patients with type-1 diabetes mellitus.
Patients who did not give informed consent.
Patients aged less than 40 years and more than 70 years.
Gestational diabetes mellitus.
Acute complications like diabetic ketoacidosis and infection.
Methods of Collection of Data
Study design – Non-interventional, observational, descriptive study
Study duration -1 year 6 months (January 2015 – June 2016)
Sample size -240 patients
Place of study – Owaisi Hospital and Research Centre, Telangana.
Statistical analysis -Descriptive statistical analysis has been carried out in the present study. Results on continuous measurements are presented on Mean ± SD (Min-Max) and results on categorical measurements are presented in Number (%).
Statistical Software: The Statistical software namely SPSS 22.0, and R Environment Ver.2.11.1 were used for the analysis of the data, and Microsoft Word and Excel have been used to generate graphs, tables, etc.
Methodology
After obtaining clearance and approval from the institutional ethical committee, 240 cases of hypertension and co-existing diabetes mellitus (with or without associated chronic complications) as diagnosed by a physician, fulfilling the above-mentioned criteria and who gave informed consent were included in the study. Details from the case records were noted using study proforma.
The results obtained were analyzed under the following headings
Age and gender-wise distribution of patients with hypertension and co-existing diabetes mellitus
Duration of diabetes mellitus and hypertension.
Class-wise distribution of antidiabetic agents and antihypertensive agents prescribed.
Percentage of drugs prescribed for other co-morbid conditions.
Percentage of patients with polypharmacy (5 or >5 drugs/prescription)
Results
The present non-interventional, prospective, observational study was done at the Medicine department of Owaisi Hospital and Research Centre, for 1 year 6 months and a total of 240 case records were collected and were analyzed and arranged in appropriate tables.
Epidemiological profile
Age distribution
Table 1: Age distribution of patients studied.
| Age in years | Number of patients | % of patients |
| 40-45 | 40 | 16.6 |
| 46-50 | 54 | 22.5 |
| 51-55 | 26 | 10.3 |
| 56-60 | 66 | 27.5 |
| 61-65 | 43 | 17.9 |
| 66-70 | 11 | 4.5 |
| Total | 240 | 100 |
Table I shows the age wise distribution of hypertension with co-existing diabetes mellitus patients. The mean age of the study population was 53.97 ± 7.62 years.
 |
Graph 1: Age-wise distribution of study population |
Gender-wise distribution
Table 2: Gender distribution of patients studied.
| Gender | Number of patients | % of patients |
| Male | 126 | 52.5 |
| Female | 114 | 47.5 |
| Total | 240 | 100.0 |
Table II shows the gender wise distribution in the study population. Out of 240 patients studied, 52.5% were male and 47.5% were female.
 |
Graph 2: Socio-economic status of patients studied. |
Socio-economic status
Table 3: Socio-economic status of patients studied. (According to Prasad classification).
| Socio-economic status | Number of patients | % of patients |
| Low | 148 | 62 |
| Middle | 92 | 38 |
| High | 0 | 0.0 |
| Total | 240 | 100.0 |
Table III shows the socio-economic status of patients studied. In the study population 62% were from low socio-economic status and 38 % were from middle class.
Duration of type-2 diabetes mellitus in years
Table 4: Duration of type-2 diabetes mellitus in years.
| Duration of DM in years | Number of patients | % of patients |
| 1-5 years | 92 | 38.3 |
| 6-10 years | 73 | 30.4 |
| 11-15 years | 59 | 24.5 |
| >15 years | 16 | 6.6 |
| Total | 240 | 100.0 |
Table IV shows the duration of type-2 diabetes mellitus in the study population with mean duration being 7.94+ 4.66 years.
 |
Graph 3: Duration of type-2 diabetes mellitus in years |
Duration of hypertension
Table 5: Duration of hypertension in years
| Duration of Hypertension in years | Number of patients | % of patients |
| 1-5 years | 104 | 43.3 |
| 6-10 years | 86 | 35.8 |
| 11-15 years | 38 | 15.8 |
| >15 years | 12 | 5 |
| Total | 240 | 100.0 |
Table V shows the duration of hypertension in the study population with mean duration being 7.1± 4.3years.
 |
Graph 4: Duration of hypertension in years. |
Drug Data
Prescription of antidiabetic drugs
Table 6: Antidiabetic drugs prescribed.
| Antidiabetic drugs | Number of patients | % of patients |
| 1. Metformin | 186 | 77.5 |
| 2. Glimepiride | 69 | 32.1 |
| 3. Gliclazide | 34 | 14.1 |
| 4. Glipizide | 24 | 10 |
| 5. Glibenclamide | 58 | 24.2 |
| 6. Insulin | 70 | 29.1 |
| 7. Acarbose | 8 | 3 |
| 8. Voglibose | 39 | 16.25 |
| 9. Pioglitazone | 39 | 16.25 |
Table VI shows the individual antidiabetic drugs prescribed in the study population in the descending order, Metformin (77.5%), Glimepiride (32.1%), Insulin (29.1%), Glibenclamide (24.2%), Gliclazide (14.1%), Voglibose and Pioglitazone (16.25% each) and least common prescribed was Acarbose (3%).
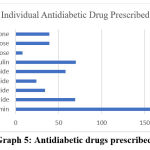 |
Graph 5: Antidiabetic drugs prescribed. |
Prescription of antihypertensive drugs
Table 7: Antihypertensive drugs prescribed.
| Antihypertensive Drugs | Number of patients(n=240) | % of patients |
| 1. Prazosin | 3 | 1.25 |
| 2. Atenolol | 45 | 18.75 |
| 3. Metoprolol | 29 | 12.0 |
| 4. Nebivolol | 3 | 1.25 |
| 5. Enalapril | 78 | 32.5 |
| 6. Ramipril | 55 | 22.9 |
| 7. Losartan | 25 | 10.4 |
| 8. Telmisartan | 21 | 8.7 |
| 9. Olmesartan | 5 | 2 |
| 10. Nifedipine | 2 | 0.8 |
| 11. Amlodipine | 102 | 42.5 |
| 12. Hydrochlorothiazide | 24 | 10 |
Table VII shows the antihypertensive drugs prescribed in the study population in the following descending order, Amlodipine (42.5%), Enalapril (32.5%), Ramipril (22.9%), Atenolol (18.75%), Metoprolol (12%), Losartan (10.4 %), Hydrochlorothiazide (10%), Telmisartan (8.7%), Olmesartan (2%), Nebivolol and Prazosin (1.25% each) and Nifedipine (0.8%).
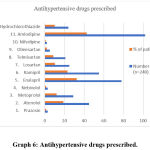 |
Graph 6: Antihypertensive drugs prescribed. |
Drugs prescribed for comorbid conditions
Table 8: Patients prescribed with drugs for other co-morbid conditions.
| Drug category | Number of patients (n=240) | % |
| 1. Antiplatelets | 96 | 40 |
| 2. Hypolipidemics | 102 | 42.5 |
| 3. Antibiotics | 54 | 22.5 |
| 4. H2 blockers/PPI | 86 | 35.8 |
| 5. Vitamins (Neutraceuticals) | 124 | 51.6 |
| 6. Miscellaneous | 100 | 41.6 |
Table VIII shows the drugs prescribed for other co-morbid conditions in the study population. Drugs for other co-morbid conditions were prescribed in the following descending order: Vitamins (51.6%), Hypolipidemics (42.5%), Miscellaneous (41.6%), Antiplatelets (40%), H2 blockers/PPI (35.8%), and Antibiotics (22.5%).
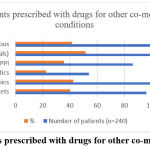 |
Graph 7: Patients prescribed with drugs for other co-morbid conditions. |
Number of drugs prescribed per encounter
Table 9: Number of drugs prescribed per encounter.
| Number of Drugs Prescribed per Encounter | Number of patients (n=240) | % of Patients |
| Two drugs | 35 | 14.5 |
| Three drugs | 58 | 24.1 |
| Four drugs | 66 | 27.5 |
| 5 or more drugs | 81 | 33.75 |
Table IX shows the number of drugs prescribed/ patient/encounter. Polypharmacy (5 or more than 5 drugs) was seen in 33.75% of study population.
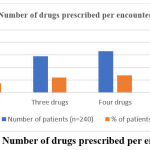 |
Graph 8: Number of drugs prescribed per encounter. |
Discussion
In the present study, polypharmacy was observed in 33.75% of the study population. The probable reason for prescribing more drugs in diabetic hypertensive patients is that these are chronic diseases in which, hypertension is usually associated with other co-morbidities like cardiovascular, cerebrovascular, renal morbidity, and mortality whereas diabetic complications cause heart attack, stroke, blindness, and kidney disease. These serious and chronic metabolic disorders have a significant impact on the health, quality of life, and life expectancy of patients, as well as on the health care systems. and for the better management of these conditions more drugs are prescribed.7 Many studies have demonstrated the need to prevent complications of hypertension with coexisting diabetes mellitus not just with tight glycemic and blood pressure control, but also control of other factors associated with increased risk of cardiovascular complications like Coronary artery disease and Hyperlipidemia. In the present study, Lipid-lowering drugs were prescribed to 42.5% of the study population. Evidence now exists about the benefits of statins in reducing cardiovascular events in diabetic patients independent of lipid levels.8 H2 blockers/ PPI were prescribed to 35.8% of the study population which indicates the high incidence of acid peptic disease in the study population.9 Antiplatelets were prescribed to 40% of the study subjects. This shows the presumed high risk of cardiovascular complications like Ischemic heart disease in diabetic hypertensive patients. 5000 patients were followed for 12 years in the MRFIT trial and it was found that the occurrence of cardiovascular disease (CVD) was up to three times more in diabetic men than nondiabetic controls, irrespective of systolic pressure, age, cholesterol, ethnic group, or use of tobacco. The same study also confirmed that systolic HTN, elevated cholesterol, and cigarette smoking were independent predictors of mortality and that the presence of at least one of these risk factors had a greater impact on increasing CVD mortality in patients with diabetes than in those without diabetes.10 Overuse of vitamins (51.6%) was also observed in this study. Several reasons can be attributed to the upsurge in the use of dietary supplements for the management of diseases. Diabetes and hypertension represent a huge financial cost to the government and affected individuals, which is predicted to increase over the next 20 years. Not everyone can afford the latest technology and advancements in the treatment of these diseases, dietary supplements and pharmacological interventions are therefore necessary.11 In this study polypharmacy is about 33.75%, which is similar to a cross-sectional analysis of the Survey of Health, Ageing, and Retirement in Europe (SHARE) database which showed that the prevalence of polypharmacy, defined as taking five or more medications concurrently in older adults aged 65 years or more, was between 26.3% and 39.9% among 17 European countries and Israel.12 Another study done by Agrawal and Nagpur revealed that ≤4 number of drugs were prescribed to 74% population, 5–9 number of drugs were prescribed to 25% population which is similar to this study in which ≤4 drugs were prescribed to 66.25% of the study population and 5-9 drugs were prescribed to 33.75% of the study population.13 One Canadian study, which enrolled nursing home residents, reported polypharmacy employment in 214 patients with type 2 diabetes mellitus and arterial hypertension, with 48% of these patients having been prescribed at least nine drugs. More non-antidiabetic drugs were prescribed in patients with overtreated diabetes (those receiving at least one antidiabetic drug, with an HbA1c ≤ 7.5%). The authors concluded that the aggressive treatment of cardiovascular risk factors raises the risk of polypharmacy, especially in frail patients.14 Observational studies have shown that polypharmacy is associated with increased side effects, harmful drug interactions, medication non-adherence, and functional and cognitive decline, and frailty.15 It has also been reported to be associated with other important adverse health outcomes such as the increased risk of hospitalization and mortality.16 However, no validated tool or strategy has been proven superior in improving polypharmacy-related patient outcomes. Also, no one validated tool assesses all aspects of potentially inappropriate medication use or polypharmacy.17 Based on a 2018 Cochrane review, it is unclear if interventions to reduce inappropriate polypharmacy improve patient-oriented outcomes.17
Conclusion
Polypharmacy has been found to be integral in patients with coexisting hypertension, diabetes mellitus type II, and other comorbidities. It is essential to practice judicious prescribing especially in patients with multiple conditions. Moreover, the Physicians should identify and prioritize medications to discontinue and discuss potential deprescribing with the patient.18-19 Three professional organizations in the American Board of Internal Medicine Foundation’s Choosing Wisely campaign (American Geriatrics Society, American Society of Health-System Pharmacists, and American Psychiatric Association) specifically mention polypharmacy and the need to review medications regularly, question the utility of adding new medications, and deprescribe when appropriate.[19] The necessity for immediate and effective polypharmacy management has been prioritized to decrease the risks and costs of prescriptions, especially in developing countries. There is a need for larger studies that follow patients throughout life to improve understanding of factors predicting polypharmacy and allow detection of vulnerable people at earlier stages.20 Distinguishing between appropriate and inappropriate polypharmacy is necessary and more studies are needed to apply this approach.
Acknowledgment
I would like to thank Professor and Head of the Medicine department, Owaisi hospital and research center, Dr. Siraj and Dr. Mohammed Mohsin, Professor and Head of the Department of Pharmacology, Deccan college of medical sciences for their support.
Conflict of interest
None
Funding sources
None
References
- Masnoon, Nashwa; Shakib, Sepehr; Kalisch-Ellett, Lisa; Caughey, Gillian E. (October 2017). “What is polypharmacy? A systematic review of definitions”. BMC Geriatrics. 17(1):230. doi:1186/s12877-017-0621-2. ISSN 1471-2318. PMC 5635569. PMID 29017448
CrossRef - Sharma P, Gupta N L, Chauhan H S. Prevalence of Polypharmacy: Comparing the status of Indian states. Indian j Community Fam Med[serial online] 2019 :5:4-9. Available from: https://www.icfm.org/text.asp?2019/5/1/4/262114
CrossRef - Seema Abhijeet, Cowall. The current status of diabetes mellitus in India – NCBI. Australasian medical journal 2014;7(1) 45-48
CrossRef - Linjakumpu, S. Hartikainen, T. Klaukka, J. Veijola, S.-L. Kivelä, and R. Isoaho, “Use of medications and polypharmacy are increasing among the elderly,” Journal of Clinical Epidemiology, vol. 55, no. 8, pp. 809–817, 2002.View at: Publisher Site| Google Scholar
CrossRef - Haider SI, Johnell K, Weitoft GR, Thorslund M, Fastbom J (January 2009). “The influence of educational level on polypharmacy and inappropriate drug use: a register-based study of more than 600,000 older people”. Journal of the American Geriatrics Society. 57(1): 62–9. doi:1111/j.1532-5415.2008.02040.x. PMID 19054196. S2CID 205703844
CrossRef - “Polypharmacy in Elderly Patients“ (PDF). Vumc.nl. Archived from the original (PDF)on 22 January 2016. Retrieved 16 January 2015.
- Afolayan AJ, Wintola OA. Dietary supplements in the management of hypertension and diabetes – a review. Afr J Tradit Complement Altern Med. 2014;11(3):248-258. Published 2014 Apr 3. doi:10.4314/ajtcam.v11i3.35
CrossRef - Bishnu H. Subedi, MD, Rajesh Tota-Maharaj, et al. The Role of Statins in Diabetes Treatment.Diabetes Spectrum 2013Aug; 26 (3): https://doi.org/10.2337/diaspect.26.3.156
CrossRef - Xiong X, Chen J, He M, Wu T, Yang H. Helicobacter pylori infection and the prevalence of hypertension in Chinese adults: The Dongfeng- Tongji cohort. J Clin Hypertens. 2020;22:1389-1395.
CrossRef - Multiple risk factor intervention trial. Risk factor changes and mortality results. Multiple Risk Factor Intervention Trial Research Group. JAMA 1982; 248:1465–1477.
CrossRef - Bastaki S. Review: Diabetes mellitus and its treatments. Int J Dia Metabol. 2005;13:111–134.
CrossRef - Midão L, Giardini A, Menditto E, et al. Polypharmacy prevalence among older adults based on the survey of health, ageing and retirement in Europe. Arch Gerontol Geriatr2018; 78: 213–220. [PubMed] [Google Scholar] CrossRef
- Agrawal RK, Nagpure S. A study on polypharmacy and drug interactions among elderly hypertensive patients admitted in a tertiary care hospital. Int J Health Allied Sci 2018;7:222.
- McCracken R., McCormack J., McGregor M.J., Wong S.T., Garrison S. Associations between polypharmacy and treatment intensity for hypertension and diabetes: A cross-sectional study of nursing home patients in British Columbia, Canada. BMJ Open. 2017;7:e017430. doi: 10.1136/bmjopen-2017-017430.
CrossRef - Maher RL, Hanlon J, Hajjar ER. Clinical consequences of polypharmacy in elderly. Expert Opin Drug Saf2014; 13: 57–65.
CrossRef - Leelakanok N, Holcombe AL, Lund BC, et al. Association between polypharmacy and death: a systematic review and meta-analysis. J Am Pharm Assoc (2003)2017; 57: 729–738.e10. [PubMed] [Google Scholar] CrossRef
- Rankin A, Cadogan CA, Patterson SM, et al. Interventions to improve the appropriate use of polypharmacy for older people. Cochrane Database Syst Rev. 2018;(9):CD008165.
CrossRef - Scott IA, Hilmer SN, Reeve E, et al. Reducing inappropriate polypharmacy: the process of deprescribing. JAMA Intern Med. 2015;175(5):827–834.
CrossRef - Choosing Wisely. An initiative of the ABIM Foundation. http://www.choosingwisely.org. Accessed May, 2021.
- Khezrian M, McNeil CJ, Murray AD, Myint PK. An overview of prevalence, determinants and health outcomes of polypharmacy. Ther Adv Drug Saf. 2020;11:2042098620933741. Published 2020 Jun 12. doi:10.1177/2042098620933741
CrossRef









