Giorgio Attina , Stefano Mastrangelo
, Stefano Mastrangelo and Antonio Ruggiero*
and Antonio Ruggiero*
Pediatric Oncology Unit, Fondazione Policlinico Universitario A.Gemelli IRCCS, Universita’ Cattolica Sacro Cuore, Rome, Italy.
Corresponding Author E-mail: antonio.ruggiero@unicatt.it
DOI : https://dx.doi.org/10.13005/bpj/2251
Abstract
Bisphosphonates have found in recent years an increasingly wide application in adult neoplastic diseases and osteoporosis. Their mechanism of action is based on the inhibition of bone turnover favouring, in particular, the mineralization and the reduction of the frequency of the remodelling cycles. The fields of application of bisphosphonates in paediatric age are constantly evolving although new trials are needed to define the schedule of administration and their long-term side effects.
Keywords
Bisphosphonates; Bone; Children
Download this article as:| Copy the following to cite this article: Attina G, Mastrangelo S, Ruggiero A. The Role of Bisphosphonates in Childhood Diseases. Biomed Pharmacol J 2021;14(3). |
| Copy the following to cite this URL: Attina G, Mastrangelo S, Ruggiero A. The Role of Bisphosphonates in Childhood Diseases. Biomed Pharmacol J 2021;14(3).Available from: https://bit.ly/2X2jXxu. |
Introduction
Bisphosphonates have had in recent years an increasingly wide application in neoplastic adult pathologies, such as multiple myeloma and bone metastases from solid tumors 1. From a chemical point of view, bisphosphonates are structural analogues of pyrophosphate. They can be administered orally or parenterally and, when absorbed by hydroxyapatite crystals, act mainly by inhibiting bone resorption. The net effect is to favor mineralization and at the same time reduce the bone turn over 2.
Despite their widespread use in diseases of adult age, there are still few clinical applications in the paediatric field, especially in the oncology area or in children with problems related to chemotherapeutic treatments 3-5. The limitations to their use in paediatric age are based on a potential interaction with the rapid process of remodelling, that is necessary in a growing skeleton, resulting in potential alteration of normal mineralization processes. There is extensive experience on the use and safety of bisphosphonates in adults and numerous clinical studies have been conducted 6,7. On the contrary, there are still very few studies in paediatric age and the experience with the use of bisphosphonates is still minimal, although the fields of application are constantly evolving 8,9.
Bone remodeling
The skeleton represents a metabolically active system that undergoes phenomena of remodelling continuously throughout life. This activity is necessary to maintain the integrity of the skeleton itself, but it also aims to provide homeostasis of calcium and phosphorus, essential elements for the performance of various metabolic functions. Bone remodelling starts from the early stages of foetal life and continues until the completion of bone structure in young adults with the closure of the growth cartilage, while remaining physiologically active in the rest of life. The cells involved in the remodelling process are essentially of two types:osteoblasts, of mesenchymal origin; osteoclasts, of hematopoietic origin.
The remodelling takes place in a series of steps: in the first phase, called “activation”, the osteoblastic cells interact with the cells of the blood supply chain to give rise to osteoclasts, which, in turn, contact the mineralised bone surface and begin the “resorption” phase 6, 10,11.
In this phase, all the components of the bone matrixare degraded, including collagen by hydrogen ions and lysosomal enzymes secreted by osteoclasts. In this way, irregular cavities are formed on the surface of the bone trabeculae (“howship gaps”) or cylindrical channels (“havers channels”) at the level of the cortical bone. At the end of this phase of activity of the osteoclasts begins a phase called “inversion” during which mononucleate cells of the macrophage line are placed on the surface of the bone contributing further to the degradation of the collagen.
The next stage is the synthesis of proteoglycans with the formation of the so-called “cement line” and the release of growth factors: the “formation”phase beginsthat concludes the bone remodelling cycle with the filling of the cavities by the osteoblasts, progressively differentiated from the mesenchymal precursors and with the deposition of a mineralisable matrix 6, 10,11.Bone remodelling recognizes regulation at both systemic and local levels.
At the systemic level
PTH (parathyroid hormone) is particularly active on bone resorption and has a biphasic action with regard to bone formation. In particular, high concentrations inhibit the synthesis of collagen, while its prolongedand intermittent administration produces an increase in bone formation;
1,25 dihydroxyvitamin D acts mainly at the intestinal level favoring the resorption of calcium and phosphates;
calcitonin is an important hormone in skeletal development, but does not play a decisive role in regulating calcium in adult individuals;
estrogens act by altering the production of local factors that regulate the activity of osteoclasts and osteoblasts: in fact,the lack of estrogen leads to a condition in which the resorption exceeds the formation resulting in a decrease in bone mass;
glucocorticoids are needed for bone differentiation during development, but their main effect leads to osteoporosis.
At the local level, numerous cytokines and growth factors produced by macrophage cells, influence the interaction between osteoblasts and osteoclasts 10-12.
In childhood and adolescence the affixingof new bone exceeds the resorption.
Bisphosphonates, through their action on osteoclasts, decrease the frequency of the beginning of the cycles of remodeling. The increase in bone mineral density, observed following treatment with bisphosphonates is due to the insertion of new bone in the spaces that are formed during remodeling.
Structure and mechanism of action
Bisphosphonates are chemically analogous to endogenous pyrophosphate. The presence of a carbon atom, instead of an oxygen atom, at the centre of the molecule gives the drug greater resistance to hydrolysis by alkaline phosphatase [6, 10-12]. The two phosphoric groups are attached directly to the carbon atom from which depart also two lateral (R1) chains R1, usually a hydroxyl that participates in the bond with the mineralized matrix, and R2, responsible for the biological properties of bisphosphonates, including also the antiresorptive activity, which differs considerably for each compound (Figure 1).
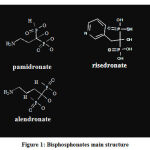 |
Figure 1: Bisphosphonates main structure. |
The presence of the PCP (planar cell polarity) and the presence of hydroxyl groups give the drug a high affinity for hydroxyapatite crystals as well as a rapid and efficient recognition of the bone mineral surface as a target. Therefore, theycan bind to the mineral component, and they are then released from the bone and internalized by osteoclasts, induce the apoptosis of osteoclasts and interfere with osteoclastic activity resulting in loss of bone resorption capacity. At the molecular level, bisphosphonates of structure similar to inorganic pyrophosphate, are incorporated by osteoclasts as nonhydrolyzable analogues of ATP (adenosine triphosphate),and inhibit consequently the activity of intracellular enzymes ATP-dependent causing a functional deficit due to energy depletion.Bisphosphonates containing one or two nitrogen atoms (first or second generation), intervene on the mevalonate pathway, the pathway that leads to the formation of cholesterol. These compounds inhibit the post translational modification (prenylation) of proteins with farnesyl or geranylgeranyl groups, essential for their localization in the membranes and therefore for their biological function. Inhibition of prenylation causes profound,changes in cell morphology, proliferation and translation of signals, and ultimately causes cell death programmed for apoptosis. The result is, for osteoclasts, the impossibility to form vesicles and to organize the “ruffled border” (membrane invagination favouring bone resorption). At the molecular level, the inhibition of osteoclasts leads to important cellular effects, such as: decreasedactivity, inhibition of recruitment, inhibition of osteoblast precursors, damage and apoptosis of osteoblasts. In vitro studies have suggested a potential inhibition action on osteoclasts mediated by osteoblasts. At the tissue level, as a direct effect of these cellular modifications, the suppression of the bone turn-over is registered.
Pharmacokinetic
Bisphosphonates available in clinical practice differ in structure,route of administration and efficacy(Table 1).
Table 1: Bisphosphonates, route of administration and their relative effectiveness
| MEDICATION | ORAL | PARENTERAL | RELATIVE EFFECTIVENESS |
| Etidronate | + | + | 1 |
| Clodronate | + | + | 10 |
| Tiludronate | + | 10 | |
| Pamidronate | + | + | 100 |
| Neridronate | 100 | ||
| Olpadronate | 100-1000 | ||
| Alendronate | + | 100-1000 | |
| Ibandronate | + | 1000-10000 | |
| Risedronate | + | 1000-10000 | |
| Zolendronate | + | >10000 |
The bioavailability of oral preparations is much lower than that of intravenously administered preparations. Bisphosphonates orally administered are characterized by a poor intestinal absorption, not exceeding 10%. For alendronate, for example, one of the most commonly used bisphosphonates, absorption is 0.5-0.7%. Absorption is also strongly hampered by both drinks, excluding water, and foods, in particular those containing calcium (milk and dairy products). Studies carried out on alendronate suggest that absorption is hindered even two hours after a meal and is also reduced by 50% if the drug is taken together with coffee or orange juice. Forthis reason,it is recommended to take this medicine only with water, at least 30 minutes before breakfast 1, 10,13. The bisphosphonates half-life is short. A percentage between 20 and 50% of the absorbed portion is captured by the bone within 12-24 hours, the rest is quickly excreted with urine. Bisphosphonates are deposited in the skeleton and in the remodelling sites, in varying degrees, depending on the bone turnover. They remain for a long time at skeletal level; their elimination isvery slow, and a half-life in the skeleton has been calculated to be of several years 1,14.
Clinical applications
The use of bisphosphonates has been extended to the paediatricage only in the last years and to date they find indication in a series of disorders, grouped essentially in four categories: 1) osteoporosis,localized or generalized; 2) metabolic diseases; 3) heterotopic calcification of soft tissues; 4) resistant hypercalcemia.
Osteoporosis
Osteoporosis is characterized by the loss of bone mass and the integrity of the bone architecture, which becomes fragile and at high risk of fractures with high mortality and morbidity. Idiopathic osteoporosis in children and adolescents is rare; in most cases it is secondary to neurological, endocrine, haematological, gastrointestinal disorders or steroid therapy 15,16.
The suppression of bone resorption with a marked increase in bone mineral density and decrease of biological parameters of bone turn over, such as alkaline phosphatase and urinary hydroxyproline, has been demonstrated in children treated with pamidronate. Adult studies have shown that bisphosphonates are more effective in steroid-induced osteoporosis than vitamin D 17.
It is estimated that about 14% of patients in chronic treatment with glucocorticoids receive therapy for the prevention of osteoporosis; Bone mass alterations are present in more than 40% of patients in chronic glucocorticoid treatment with an incidence of fractures up to 50%. Many aspects are still to be defined regarding the threshold dosage responsible for the reduction of bone mineral density, the importance of the cumulative dose, the use of alternative routes and methods of administration; it is documented that the reduction of bone mineral density is greater in the first 6-12 months of therapy and that the osteopenizing effect is more evident if the treatment exceeds 6 months 15-17.
Forms of premature osteoporosis have also been documented in patients with cystic fibrosis. The pathogenesis is multifactorial. Aetiology can include: hypogonadism, malabsorption, pancreatic insufficiency, calcium and vitamin D deficits, the use of glucocorticoids, and the presence of proinflammatory cytokines. Haworth et al. showed an increase in bone mineral density in patients treated with pamidronate compared to placebo 18. The same results were obtained in patients with thalassemia treated with alendronate.
Also in this circumstance, osteoporosis recognizes a multifactorial pathogenesis: hypogonadism, expansion of the bone marrow, calcium deficiency and vitamin D. Other hematological disorders can be associated with osteopenia. In congenital neutropenia, treatment with G-CSF increases the activity of osteoclasts and therefore bone resorption 15. The results of children treated with etidronate appear encouraging.
Fibrodysplasia
Mccune-Albright syndrome, a form of fibrodysplasia, is characterized by osteolytic lesions at the level of long bones and skull in the presence of hyperproliferation of pre-osteoblasts.
A high bone turn-over is associated with increased alkaline phosphatase and hydroxyproline. Treatment with pamidronate at a dose of 1 mg/kg for three days every four months showed a reduction in alkaline phosphatase and hydroxyproline levels as well as an increase in bone mineral density with a significant reduction in the risk of pathological fractures 19.
Osteogenesis imperfecta
Osteogenesis imperfecta is characterized by the presence of mutations in one of the two genes coding for collagen type I; from the clinical point of view all the tissues that contain it are affected: at the bone level there is a serious and progressive picture of osteoporosis, with the possibility of fractures and serious deformities; tendons and ligaments become lax inducing joint instability; at the level of the teeth dentinogenesis imperfecta occurs; sclerae become thinner and become grey-bluish 21-23.
Glorieux et al. showed that in a group ofchildren aged 3 to 16 with osteogenesis imperfecta, treatment with intravenous pamidronate 6.8 mg/kg weight/year led to an increase in bone density with a significant decrease in fractures (-1,7/year) and improved clinical outcome 24.
Hypercalcemia
Hypercalcemia associated with paediatric cancers is quite rare: it occurs in about 0.2-0.7 % of cancer patients. A neoplasm can cause hypercalcemia by direct invasion of bone by neoplastic cells and consequent destruction of the bone with release of calcium, for tumor secretion of a similar PTH-acting protein or other cytokines stimulating calcium resorption at the bone and kidney levels or for tumor production of 1,25 dihydroxytamin D3, followed by increased intestinal calcium absorption.
The efficacy of bisphosphonates is limited in cases of hypercalcemia induced by similar PTH proteins as the drug is not able to block calcium resorption at the renal level 25-27. In metastatic disease, bisphosphonates, are used for their analgesic effect in addition to reducing the risk of pathological fractures 20.
Adverse effects
Bisphosphonates are well-tolerated drugs when administered orally or intravenously. Common side effects are headache, myalgia, dyspepsia, nausea, and altered bowel habit 28-34. Although the incidence of corrosive esophagitis is low, it can be severe when it occurs. In the case of intravenous administration, may be the thermal rise of 1° C and a flu-likesymptomatology. Metabolic alterations are usually transient: hypocalcemia with hypophosphatemia and secondary increase of PTH and vitamin D may occur, but rarely have significant clinical relevance 1,8,10,35,36.
In children, in particular, the possibility of a potential negative effect of bisphosphonates on the activity of growth cartilage (early welding) was raised. Bisphosphonates could have a potential harmful effect on the growing cartilage: the increase of bone formation and the increased osteoblastic activity in correspondence of the growth cartilage lead to the development of sclerosis although in some studies a gradual decrease or total disappearance of such sclerotic processes has been documented after withdrawal of therapy before closure of the growth cartilage 1,8.
Recently, however, high-dose intravenous bisphosphonates have been identified as a potential risk factor for the development of osteonecrosis of the jaw among patients affected by oncological diseases. Low-dose bisphosphonate use in patients with osteoporosis or other metabolic bone disease has not been causally linked to the development of osteonecrosis of the jaw 37-39.
Conclusions
Bisphosphonates are now widely used in adults suffering from osteoporosis and bone metastases from solid tumors. Reservations about their application in paediatric age, mainly due to possible side effects, have been partially overcome although some criteria regarding minimum dose efficacy, route of administration, the start and duration of treatment, are still to be determined.
Conflict of Interest
The authors certify that they have NO affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript
Funding source
The authors received no specific funding for this work.
References
- Allgrove J. Bisphosphonates. Dis. Child., 1997;76:73-75.
CrossRef - Ezra A, Golomb G. Abministration routes and delivery system of bisphosphonates for the treatment of bone resorption. Adv. Drug. Deliv. Rev., 2002;42:175-195.
CrossRef - Ruggiero A, Ferrara P, Attinà G, Rizzo D, Riccardi R. Renal toxicity and chemotherapy in children with cancer. J. Clin. Pharmacol., 2017;83(12):2605-2614.
CrossRef - Ruggiero A, Triarico S, Trombatore G, Battista A, Dell’acqua F, Rizzari C, Riccardi R. Incidence, clinical features and management of hypersensitivity reactions to chemotherapeutic drugs in children with cancer. Eur. J. Clin. Pharmacol., 2013;69(10):1739-46.
CrossRef - Triarico S, Rinninella E, Cintoni M, Capozza M.A, Mastrangelo S, Mele M.C, Ruggiero A. Impact of malnutrition on survival and infections among pediatric patients with cancer: a retrospective study. Eur. Rev. Med. Pharmacol. Sci., 2019;23(3):1165-1175.
- Russel R.G, Croucher P.I, Rogers M.J. Bisphosphonates: pharmacology, mechanism of action and clinical uses. Osteoporos. Int., 1999;9:S66-S80.
CrossRef - Sato M, Grasser W, Endo N, et al. Bisphosphonate action. Aledronate localization in rat bone and effects on osteoclast ultrastructure. J. Clin. Invest., 1991;88:2095-2105.
CrossRef - Shaw N.J, Bishop N.J. Bisphosphonate treatment of bone disease. Arch. Dis. Child., 2005;90:494-499.
CrossRef - Srivastava T. The role of bisphosphonates in diseases of childhood. Eur, J, Pediatr., 2003;162:735-751
CrossRef - Rodan G.A. Mechanism of action of bisphosphonates. Ann. Rev. Pharmacol. Toxicol.,1998;38:375-388.
CrossRef - Mashiba T, Hirano T, Turner C.H, et al. Suppressed bone turn over by bisphosphonates increase microdamage accumulation and reduced some biochemical properties in dog rib. J. Bone Miner. Res., 2000;15:613-620.
CrossRef - Van Beek E, Hoekstra M, van de Ruit M, Löwik C, Papapoulos S.Structural requirements for bisphosphonates action in vitro. J. Bone Miner. Res., 1994;9:1875-1882.
CrossRef - Chiaretti A, Ruggiero A, Barone G, et al. Propofol/alfentanil and propofol/ketamine procedural sedation in children with acute lymphoblastic leukaemia: safety, efficacy and their correlation with pain neuromediator expression. Eur. J. Cancer Care., 2010;19(2):212-220
CrossRef - Flanagan A.M, Chambers T.J. Inibition of bone resorption by bisphosphonates: interaction between phosphonates, osteoclast and bone. Calcif. Tissue Int., 1991;49:407-415.
CrossRef - Bishop N.J, Williams D.M, Compston J.C, et al. Osteoporosis in severe congenital neutropenia treated with granulocyte colony-stimulating factor. Br. J. Haematol., 1995;89:927-928.
CrossRef - Morabito N, Lasco A, Gaudio A, et al. Bisphosphonates in the treatment of thalassemia-induced osteoporosis. Osteoporos. Int., 2002;13:644-649.
CrossRef - Homik J.E, Cranney A, Shea B, et al. A meta-analysis on the use of bisphosphonates in corticosteroid induced osteoporosis. J. Reumatol., 1999;26:1148-1157.
CrossRef - Haworth C.S, Selby P.L, Webb A.K, et al. Severe bone pain after intravenous pamidronate in adult patient with cystic fibrosis. Lancet., 1998;352:1753-1754.
CrossRef - O’Sullivan M, Zacharin M. Intramedullary rodding and bisphosphonate treatment polyostotic fibrous dysplasia associated with the McCune-Albright syndrome. J. Pediatr. Orthop., 2002;22:255-260.
CrossRef - Celin M.R, Simon J.C, Krzak J.J, Fial A.V, Kruger K.M, Smith P.A, Harris G.F. Do Bisphosphonates Alleviate Pain in Children? A Systematic Review. Curr. Osteoporos. Rep., 2020;18(5):486-504.
CrossRef - Dwan K, Phillipi C.A, Steiner R.D, Basel D. Bisphosphonate therapy for osteogenesis imperfecta. Cochrane Database Syst. Rev., 2016;10(10):CD005088.
CrossRef - Constantino C.S, Krzak J.J, Fial A.V, Kruger K.M, Rammer J.R, Radmanovic K, Smith P.A, Harris G.F. Effect of Bisphosphonates on Function and Mobility Among Children With Osteogenesis Imperfecta: A Systematic Review. J.B.M.R. Plus., 2019;3(10):e10216.
CrossRef - Falk M.J, Heeger S, Lynch K.A, et al. Intravenous bisphosphonates therapy in children with osteogenesis imperfecta. Pediatrics,. 2003;111:573-578.
CrossRef - Glorieux F.H, Bishop N.J, Plotkin H, et al. Cyclic administration of pamidronate in children with severe osteogenesis imperfecta. N. Engl. J. Med., 1998;339:947-952.
CrossRef - Roux S, Massicotte M.H, Huot Daneault A, Brazeau-Lamontagne L, Dufresne J. Acute hypercalcemia and excessive bone resorption following anti-RANKL withdrawal: Case report and brief literature review. Bone., 2019;120:482-486.
CrossRef - Kutluk M.T, Hazar V, et al. Childhood cancer and hypercalcemia. report of a case treated with pamidronate. J. Peediatr., 1997;139:828-831.
CrossRef - Illidge T,M, Hussey M, Godden C,W. Malignant hypercalcemia in pregnancy and antenatal administration of intravenous pamidronate. Clin. Oncol.,(R Coll Radiol) 1996;8:257-258.
CrossRef - Ruggiero A, Rizzo D, Catalano M, Coccia P, Triarico S, Attiná G. Acute chemotherapy-induced nausea and vomiting in children with cancer: Still waiting for a common consensus on treatment. J. Int. Med. Res., 2018;46(6):2149-2156.
CrossRef - Ferrara P, Marrone G, Emmanuele V, et al. Homotoxicological remedies versus desmopressin versus placebo in the treatment of enuresis: a randomised, double-blind, controlled trial. Pediatr. Nephrol., 2008;23(2):269-274.
CrossRef - Oryan A, Sahvieh S. Effects of bisphosphonates on osteoporosis: Focus on zoledronate. Life Sci., 2021;264:118681.
CrossRef - Falsini B, Chiaretti A, Barone G, et al. Topical nerve growth factor as a visual rescue strategy in pediatric optic gliomas: a pilot study including electrophysiology. Neural Repair., 2011; 25: 512-520.
CrossRef - Iuvone L, Peruzzi L, Colosimo C, et al. Pretreatment neuropsychological deficits in children with brain tumors. NeuroOncol., 2011;13(5):517-524
CrossRef - Timeus F, Crescenzio N, Longoni D, et al. Paroxysmal nocturnal hemoglobinuria clones in children with acquired aplastic anemia: a multicentre study. PLoS One., 2014;9(7):e101948
CrossRef - Falsini B, Ziccardi L, Lazzareschi I, et al. Longitudinal assessment of childhood optic gliomas: relationship between flicker visual evoked potentials and magnetic resonance imaging findings. J. Neurooncol., 2008; 88: 87-96.
CrossRef - Triarico S, Maurizi P, Mastrangelo S, et al. Improving the Brain Delivery of Chemotherapeutic Drugs in Childhood Brain Tumors. Cancers (Basel)., 2019;11(6):824.
CrossRef - Rinninella E, Ruggiero A, Maurizi P, et al. Clinical tools to assess nutritional risk and malnutrition in hospitalized children and adolescents. Eur. Rev. Med. Pharmacol. Sci., 2017;21(11):2690-2701.
- Li M, Zhong M, Guan C. Bisphosphonates and risk of lung cancer: Protocol for a systematic review and meta-analysis. Medicine (Baltimore)., 2021;100(1):e22839.
CrossRef - Oliveira J.R, Oliveira M.F. Primary brain calcification in patients undergoing treatment with the biphosphanate alendronate. Sci. Rep., 2016;6:22961.
CrossRef - Nicolatou-Galitis O, Schiødt M, Mendes R.A, Ripamonti C, Hope S, Drudge-Coates L, Niepel D, Van den Wyngaert T. Medication-related osteonecrosis of the jaw: definition and best practice for prevention, diagnosis, and treatment. Oral Surg. Oral Med. Oral Pathol. Oral Radiol., 2019;127(2):117-135.
CrossRef - Tsolaki E, Bertazzo S. Pathological Mineralization: The Potential of Mineralomics. Materials (Basel)., 2019;12(19):3126.
CrossRef








