Ratna Agrawal1*  and Bhabagrahi Rath2
and Bhabagrahi Rath2
1Department of Pharmacology, Late BaliRam Kashyap Memorial Government Medical College, Dimrapal, Jagdalpur, Chhattisgarh, India, 494001.
2Department of Pharmacology, V.S.S. Institute of Medical Sciences and Research, Burla, Sambalpur, Odisha, India, 768017.
Corresponding Author E-mail: ratna.arang@gmail.com
DOI : https://dx.doi.org/10.13005/bpj/2217
Abstract
Background and Objectives: Schizophrenia is the commonest and one of the best known mental disorder which usually starts before 25 years of age, leading to significant disability in both behavioural and social life. Usually the person with any mental disability has to face social ignorance, this further leads to deterioration of their health and productivity. The deterioration of the health is not only due to the course of the disease but also may be due to treatment by some of the antipsychotics, which are the main drugs for the schizophrenia management. So, the present study has been designed to determine the effectiveness of typical and atypical antipsychotics in patients with schizophrenia in terms of disability reduction caused by them using WHODAS 2.0. Methods: After taking ethics committee approval and informed consent from study participants this prospective, observational, questionnaire based study has been conducted in the Department of Psychiatry and Pharmacology of V. S.S. Institute of Medical Sciences and Research, Burla, Odisha using WHODAS 2.0 in patients suffering from schizophrenia. Results: Atypical antipsychotics lead to more reduction in disability in patients with schizophrenia than typical antipsychotics both at 6 and 12 month duration. On comparing the various atypical antipsychotics used in the study, there was no significant difference among them. Conclusion: Based on the above findings, it can be concluded that atypical antipsychotics are more effective than typical antipsychotics in terms of disability reduction. The findings may help clinicians to get better insight in the management of schizophrenia.
Keywords
Atypical antipsychotics; Effectiveness study; Schizophrenia; Typical antipsychotics; WHODAS 2.0
Download this article as:| Copy the following to cite this article: Agrawal R, Rath B. Effectiveness Study of Typical and Atypical Antipsychotics on Patients with Schizophrenia using WHO Disability Assessment Schedule (WHODAS 2.0). Biomed Pharmacol J 2021;14(3). |
| Copy the following to cite this URL: Agrawal R, Rath B. Effectiveness Study of Typical and Atypical Antipsychotics on Patients with Schizophrenia using WHO Disability Assessment Schedule (WHODAS 2.0). Biomed Pharmacol J 2021;14(3). Available from: https://bit.ly/3wH8Gyz |
Introduction
Schizophrenia is a clinical syndrome of variable, but profoundly disruptive, psychopathology that involves cognition, emotion, perception and other aspect of behaviour.1 The disorder usually begins before age 25, persists throughout life, and affects persons of all social classes.1 The National Institute of Mental Health reported a lifetime prevalence of schizophrenia is about 0.6 to 1.9 percent.1 The prevalence of schizophrenia in India is about 2.3-2.7/1000 individuals.2, 3
Schizophrenia is associated with significant social and occupational dysfunction.4 Making educational progress and maintaining employment are frequently impaired by avolition or other disorder manifestations.4 Suicidal risk as well as concurrent medical illnesses are also very common among them. Approximately 5%-6% of individuals with schizophrenia die by suicide, about 20% attempt suicide on one or more occasions, and many more have significant suicidal ideation.4 Several studies have shown that up to 80% of all schizophrenia patients have significant concurrent medical illnesses and up to 50% of these may be undiagnosed.1
There are around 65 antipsychotic medications utilized across the world. They are classified into two groups – Typical and Atypical antipsychotics. Both Typical and Atypical antipsychotics are effective in reducing positive and disorganization symptoms but are only minimally effective for negative and cognitive symptoms, which contribute significantly to the disability associated with schizophrenia.5
As schizophrenia contributes to significant disability in society, the present study has been conducted to determine the effectiveness of the two main groups of antipsychotics (typical and atypical) used in its management using WHODAS 2.0 scale. The effectiveness studies, like other types of phase IV studies, can contribute to knowledge about medications and supply relevant information in addition to that gained from phase III trials.6
Materials and Methods
After obtaining the Institutional Ethics Committee clearance and informed consent from participants, this prospective, observational and questionnaire-based study has been conducted on the patients of schizophrenia (inpatient and outpatient) Department of Psychiatry and Department of Pharmacology at V. S. S. Institute of Medical Sciences & Research, Burla, Sambalpur, Odisha from September 2015 to August 2017.
Selection of cases: Convenience sampling.
Inclusion criteria
Patients of schizophrenia aged 18 years or older, diagnosed according to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, and provided written informed consent.7
Exclusion criteria
Patients who were at imminent risk of injury to themselves or others, who had a known hypersensitivity to drugs, or who had been treated with investigational agents within the previous 30 days were not eligible for enrolment.7 Women of childbearing potential who were not using an adequate method of contraception and women who were pregnant or breast feeding were also not eligible for participation.7
Method of study
This was a 24-month, prospective, observational study in patients with schizophrenia who were initiated on various typical and atypical antipsychotics.7 Physicians were allowed to change treatment during the study as clinically warranted.7 Patient recruitment with baseline data collection has been done in the initial 6 months then patients were followed up subsequently every 6 months up to 18 months for WHODAS 2.0 scale.
The DSM-5 Disability Study Group recommended WHODAS 2.0 as the best current measure of disability for routine clinical use and recommended its inclusion in DSM-5.8 WHODAS 2.0 is a patient self-report assessment tool that evaluates the patient’s ability to perform activities in six domains of functioning over the previous 30 days, and uses these to calculate a score representing global disability.9 These domains are: Understanding and communicating Getting around (mobility) Self-care Getting along with people (social and interpersonal functioning) Life activities (home, academic, and occupational functioning) Participation in society (participation in family, social, and community activities).9 WHODAS 2.0 offers several advantages as an instrument for the assessment of functioning. 9 Multiple studies have found WHODAS 2.0 to be reliable, responsive to change, and applicable across geographic regions.9
Statistical analysis
All the scores have been evaluated using Graph pad prism version 6.0 using non- parametric scales, paired t- test (Wilcoxan signed rank test). p-value <0.05 was kept statistically significant.
Results
During the study period, 90 cases of schizophrenia were enrolled into the study during the 6 month recruitment period and were followed up for a period of 18 months while on treatment with typical and atypical antipsychotics.
Demographic profile of study participants
Out of the 90 cases, majority of patients [60 (66.7%)] belonged to the middle (25 to 45 yrs) age group, 20 (22.2%) patients were of < 25 yrs age group and rest were elderly (>45 yrs) patients [10 (11.1%)], with the age ranging from 19-70 years. Schizophrenia has been noted more in males as majority of the population, 60 (66.7%) were males and 30 (33.3%) were females. Educational status of enrolled patients was also below standard as only 10 (11.1%) patients had studied above 12th standard and rest 80 (88.89%) had studied below 12th standard. Out of 90 patients, 64 (71.1%) were married and 26 (28.9%) were unmarried.
Majority of patients belonged to low socio-economic status and were either unemployed or labourers or farmers. 26 (28.9%) out of 90 patients were unemployed, 16 (17.8%) patients were labourers, 10 (11.1%) were farmers, 22 (24.4%) patients were housewives, 14 (15.6%) were self employed and only 2 (2.2%) patients were in service as depicted in Figure 1. The antipsychotics prescribed to schizophrenia patients were trifluoperazine and chlorpromazine (typical antipsychotics) and olanzapine, risperidone, clozapine and amisulpiride (atypical antipsychotics).
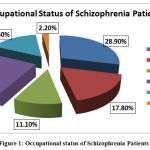 |
Figure 1: Occupational status of Schizophrenia Patients. |
Result of assessment of Schizophrenia Patients by WHODAS 2.0
At baseline, out of 90 patients 58 patients were receiving typical antipsychotics and rest 32 patients were taking atypical antipsychotics. At the end of 6 months, 16 patients out of 58 who were receiving typical antipsychotics were switched to atypical antipsychotics and 4 patients out of 32 patients who were taking atypical antipsychotics were switched to typical agents due to side effects, so total number of patients in typical antipsychotic group was 46 and in atypical group were 44. At the end of 12 months, 30 patients out of remaining 46 patients (typical antipsychotic group) were switched to atypical antipsychotics, so atypical group contained 74 patients and typical antipsychotic group contained 16 patients. After that no change had been made in the treatment of patients, the same treatment was continued till the completion of the study period.
The comparison of effectiveness of typical and atypical antipsychotics was made by noting the reduction in the level of disability using WHODAS 2.0 scale by using non parametric, paired t- test (Wilcoxan signed rank test). The scale showed significant improvement with atypical antipsychotics as compared to typical antipsychotics both after 6 and 12 month duration as presented in Table 1 and Table 2.
Table 1: WHODAS 2.0 Scale Scores during Treatment with Typical and Atypical Antipsychotics on 6 month Duration.
|
Sl No.
|
Scale
|
Mean score after 6 month of therapy with Typical antipsychotics (Mean± SEM) |
Mean score after 6 month of therapy with Atypical antipsychotics (Mean± SEM) |
Level of significance
|
| 1. | WHODAS 2.0 Scale | 3.44± 0.25 | 2.74± 0.21 | 0.0078** |
* p< 0.05 = Statistically Significant, **p< 0.01 = Highly Significant, ***p< 0.001= Very Highly Significant
Table 2: WHODAS 2.0 Scale Scores during Treatment with Typical and Atypical Antipsychotics on 12 month Duration.
|
Sl No.
|
Scale
|
Mean score after next 6 month of therapy with Typical antipsychotics (Mean± SEM) |
Mean score after next 6 month of therapy with Atypical antipsychotics (Mean± SEM) |
Level of significance
|
| 1. | WHODAS 2.0 Scale | 2.46± 0.46 | 1.92± 0.42 | 0.0001**** |
* p< 0.05 = Statistically Significant, **p< 0.01 = Highly Significant, ***p< 0.001= Very Highly Significant
As atypical antipsychotics showed better improvement as compared to typical antipsychotics, comparison was made among the atypical antipsychotics (olanzapine, risperidone, amisulpiride and clozapine) used in the study by using WHODAS 2.0. By comparing the atypical antipsychotics on the basis of WHODAS 2.0 scale score using Kruskall Wallis test, there was no statistically significant difference among the atypical antipsychotics as shown in Table 3.
Table 3: Comparison of Atypical Antipsychotics at different time intervals by using WHODAS 2.0 scale.
| Month | Olanzapine | Risperidone | Amisulpiride | Clozapine | p value
|
| 6 month | 3.18 | 3.24 | 2.12 | 3.81 | 0.139 |
| 12 month | 2.57 | 2.36 | 1.82 | 2.91 | |
| 18 month | 1.98 | 1.9 | 1.5 | 2.53 | |
| Mean± SEM | 2.57± 0.35 | 2.50± 0.39 | 1.81± 0.18 | 3.08±0.38 |
*p< 0.05 = Statistically Significant
Discussion
This prospective, observational study aimed to determine the effectiveness of the two main groups of antipsychotics (typical and atypical) used in its management using WHODAS 2.0 scale in schizophrenia patients. The demographic characteristics in terms of age, sex and marital status of the study participants corroborates with the study conducted by Cortesi et al.10 The occupational status of patients was found unsatisfactory in the present study and poor occupational status is directly related to low socio-economic status, poor treatment adherence and poor patient care, leading to poor prognosis and quality of life. A meta-analysis conducted by Holla et al including three studies from India showed better socio- occupational status as compared to this study. The reason may be that, the studies were conducted in Agra, Chandigarh and Chennai, which are more developed states as compared to Odisha and so provide higher opportunity of education and employment.11, 12
Comparison of effectiveness of typical and atypical antipsychotics based on disability reduction by WHODAS 2.0 showed more reduction in disability level by atypical antipsychotics both at 6 and 12 month duration. The results of the study corroborates with the study conducted by Ravanic et al which also found that atypical antipsychotics, in long term (five years) showed better effectiveness in chronic schizophrenia with positive and negative symptoms than typical antipsychotics as per scores of psychometric instruments like GWB (General Well- Being scale), PANSS (Positive And Negative Syndrome Scale) and CGI.13
Comparison among all the atypical antipsychotics used in the study (olanzapine, risperidone, amisulpiride, clozapine) by using scores of WHODAS 2.0 showed that there was no statistically significant difference among all the atypical antipsychotics used. The results corroborate with Mcevoy et al and Swartz et al, where comparison among olanzapine, risperidone and quetiapine showed no statistically significant improvement in PANSS total score after 12 month follow-up study.14, 15, 16
This study had some limitations that should be mentioned. With its relatively small sample size, selection bias could not be ruled out. The effectiveness of newer atypical antipsychotics like aripiprazole, paliperidone and quetiapine etc. could not be measured because their higher cost prohibited clinicians (government hospital based study) to prescribe them.
Conclusion
Based on the above findings, it can be concluded that atypical antipsychotics are more effective than typical antipsychotics in terms of disability reduction. While among different atypical antipsychotics available, they can be prescribed depending upon the individual patient’s need, compliance and tolerability. The findings of the study may contribute in existing data regarding effectiveness of various available antipsychotics for the treatment of schizophrenia and may help prescribers in evidence based prescribing. But, further more pragmatic studies are required to get better knowledge about newer atypical antipsychotics.
Acknowledgement
Authors are thankful to the Dr. R. K. Shukla, Head of the Department, Psychiatry, V.S.S. Institute of Medical Sciences and Research, Burla, Sambalpur, Odisha for providing constant support for recruitment of study participants.
Conflict of Interest
None declared.
Funding source
None declared.
References
- Grebb JA, Caroly SP, Sussman N, editors. Kaplan & Sadock’s Synopsis of Psychiatry: Behavioral Sciences/ Clinical psychiatry, 10th Edition. Lippincott Williams & Wilkins; 2007:467-68.
- Madhav S. Epidemiological study of prevalence of mental disorders in India. Indian J Community Med 2001;26:198.
- Reddy VM, Chandrashekar CR. Prevalence of mental and behavioural disorders in India: A meta-analysis. Indian J Psychiatry 1998;40:149-57.
- Diagnostic and Statistical Manual of Mental Disorders, 5th Edition. England: American Psychiatric Association; 2013. Available at: https://www.psychiatry.org/psychiatrists/practice/dsm. Accessed on 30 December 2019.
- Tandon R, Nasrallah HA, Keshvana MS. Schizophrenia, “just the facts” 5: treatment and prevention: past, present and future. Schizopher Res. 2010;122(1-3):1-23.
CrossRef - Moller HJ. Effectiveness studies: advantages and disadvantages. Dialogues Clin Neurosci 2011;13:199-207.
CrossRef - Agrawal R, Rath B, Shukla RK, Mohapatra S. Effectiveness analysis of antipsychotics in schizophrenia using psychometric scales: an observational study. Int J Basic Clin Pharmacol 2020;9:305-9.
CrossRef - American Psychiatric Association: Insurance implications of DSM-5. Available at http://www.psychiatry.org/dsm5. [Accessed on March 18, 2020]
- Gold LH. DSM-5 and the Assessment of Functioning: The World Health Organization Disability Assessment Schedule 2.0 (WHODAS 2.0). J Am Acad Psychiatry Law 2014;42(2):173–81.
- Cortesi PA, Mencacci C, Luigi F, Pirfo E, Berto P, Sturkenboom CJM, et al. Compliance, persistence, costs and quality of life in young patients treated with antipsychotic drugs: results from the COMETA study. BMC Psychiatry. 2013;13:244-471.
CrossRef - Holla B, Thirthalli J. Course and outcome of schizophrenia in Asian countries: Review of research in the past three decades. Asian Journal of Psychiatry 2015; 14: 3- 12.
CrossRef - Jablenskey A, Sartorious N, Ernberg G, Anker M, Korten A, Cooper JE et al. Schizophrenia: Manifestations, incidence and course in different cultures: A WHO ten country study. Psychological Medicine, Monograph supplement 1992: 20: 1- 97.
CrossRef - Ravanic DB, Dejanovic SMD, Janjic V, Jovic SD, Milovanovic DR, Jakovljevic V et al. Effectiveness of clozapine, haloperidol and chlorpromazine in schizophrenia during a five- year period. Arq Neuropsiquiatr. 2009;67(2):195-202.
CrossRef - McEvovy JP, Liberman JA, Perkins DO et al. Efficacy and tolerability of olanzapine, quetiapine and risperidone in the treatment of early psychosis: A randomized, double blind 52- week comparison. Am J Psychiatry 2007; 164: 1050- 60.
CrossRef - Swartz MS, Perkins KO, Stroup TS, Davis SM, Capuano G, Rosenheck RA et al. Effects of antipsychotic medication on psychosocial functioning in patients with chronic schizophrenia: Findings from the NIMH CATIE study. Am J Psychiatry 2007; 164: 415- 27.
CrossRef - Johnson E, Jorgenson HA. Effectiveness of second generation antipsychotics: a systematic review of randomized trials. BMC Psychiatry 2008;8: 31.
CrossRef







