Nimish S. Narkar , Teja Deshpande
, Teja Deshpande , B. T. Rane*
, B. T. Rane* , Revati Kothari
, Revati Kothari , A. V. Tilak
, A. V. Tilak , and Harshavardhan Bhide
, and Harshavardhan Bhide
Department of Pharmacology, Dr. D. Y. Patil Medical College, Hospital and Research Centre, Dr. D. Y. PatilVidyapeeth, Pimpri, Pune, India – 411018
Corresponding Author Email id:bt.rane@yahoo.comDOI : https://dx.doi.org/10.13005/bpj/2197
Abstract
Hypertension is a leading cause of cardiovascular morbidity and mortality. Although known as disease of old age, younger population is at increasing risk due to various factors including obesityand diabetes. Antihypertensive drug treatment being the only measure to control the raised blood pressure, large number of patients remain untreated or inadequately treated. Prescription pattern studies are needed to optimize and control the drug treatment. Present study was done with the aim to study the prescription pattern of antihypertensive drugs in a tertiary care hospital in western India.Pattern of drugs prescribed whether in combination or as single drug in various comorbidities were the objectives of the study. It was observed that ARB was the most commonly prescribed drug (41.5%) either alone or in combination. Multidrug therapy being the preferred treatment (56%), combination of ARB, CCB and Diuretic was the most common (35.7%). Diabetes mellitus was the most commonly associated comorbidity in hypertensive patients (39%), with ARB and CCB as the preferred antihypertensive drugs used in them. The treatment prescribed seemed to be specific to age, comorbidity and was in accordance with national and international guidelinesincluding the Indian Guidelines on Hypertension.
Keywords
Antihypertensive drugs; Hypertension; Prescription pattern.
Download this article as:| Copy the following to cite this article: Narkar N. S, Deshpande T, Rane B. T, Kothari R, Tilak A. V, Bhide H. Pattern of Antihypertensive Drugs Prescribed in a Tertiary Care Hospital in Western India. Biomed Pharmacol J 2021;14(2). |
| Copy the following to cite this URL: Narkar N. S, Deshpande T, Rane B. T, Kothari R, Tilak A. V, Bhide H. Pattern of Antihypertensive Drugs Prescribed in a Tertiary Care Hospital in Western India. Biomed Pharmacol J 2021;14(2). Available from: https://bit.ly/3xgjqVB |
Introduction
Hypertension can be defined as sustained rise in blood pressure of 140/90 mmHg or more. This emphasizes medical attention in patients with high risk of hypertension-related cardiovascular disease (CVD).1
Hypertension is themost common cause for increasing the risk of cardiovascular diseases and renal disorders. Although treatment with antihypertensive drugs lowers the risks, huge part of the population with hypertension fall under the category of either being not treated or under inadequately treated group.2
Non-pharmacologic interventions are considered first to manage the raised BP.3The initial first-line drug treatment for stage 1 of hypertension includes angiotensin converting enzyme (ACE) inhibitors or angiotensin receptor blockers (ARBs), thiazide diuretics and calcium channel blockers (CCBs). Two first-line drugs belonging to different classes are recommended in patients of stage 2 hypertension.3
Combination of drugs belonging to different classes with distinct mechanisms of action helps in attaining effective BP control with minimum side effects.4Administration of antihypertensive drugs with once a day dosage improves the patient compliance. Although the treatment with antihypertensive drugs is usually life-long, an effort should be made to reduce the dose of antihypertensive drugs and/or its number after effective control of BP (step-down therapy).4
Studies on prescription pattern of antihypertensive drugs are important for optimization of drug therapy and drug control in individuals with hypertension. This will help in guiding the current and the future doctors in their prescribing patterns of antihypertensive as well as other concomitant drugs. With this background, the present research was aimed at studying the prescription pattern of antihypertensive drugs in a tertiary care hospital in western India with objectives to study overall prescribing pattern of various class of antihypertensive drugs either as single drug or in combinations and studying various associated comorbidities and the drugs used in them.
Material and Methods
This observational study, after obtaining ethical clearance, was conducted in a tertiary care hospital in Maharashtra, India from January 2019 to December 2019 with a sample size of 200. Adults in the age group of 18 – 70 years with known case of or newly diagnosed cases of hypertension who are on antihypertensive drugswere included in the study while pregnant and lactating females and patients with unreliable history were excluded.
Prescription pattern of antihypertensive drugs were categorized according to age, gender, class of drug, single or multidrug treatment and comorbidity and the drugs used in them. Data was collected and entered in Microsoft Excel and analysis was done using WinPepi software (Version 11.65)5. Categorical variable was expressed in terms of frequency and percentage and graphs were prepared using Microsoft excel sheet.
Observations and Results
A total of 200 patients were recruited for the present study who were prescribed antihypertensive drugs. Their prescriptions were evaluated to study their prescribing patterns. The observations of this study are as follows.
Distribution of Cases According to Gender And Age:
Out of total 200 cases, 115 (57.5%) were male and 85 (42.5%) were female.Among 200 cases, a maximum of 77 i.e. 38.5% of the total cases were in the age group of 51 – 60 years and the least number of cases were observed in the age group of 18 – 20 and 21 – 30 i.e. only one in each groups accounting to a total of 1%. 29.5% cases were in fifth decade, 16.5% in fourth and 14.5% in seventh decade of life.
Distribution of Cases According to the Class of Drug
Table 1 and figure 1show distribution of study cases according to the class of antihypertensive drugs prescribed. Angiotensin Receptor Blockers (ARBs) was the most prescribed class of drug accounting to 41.5% of the total drugs prescribed i.e. 164 cases were on ARBs.Telmisartan was the drug prescribed from this class of antihypertensive drugs. This was followed by Calcium Channel Blockers (CCBs) i.e. Amlodipine in 100 cases (25.3%). Prescriptions with Diuretics, Hydrochlorothiazide being the drug prescribed from this class, were 77 in number, making it 19.5% of the total. 23 (05.8%) had Enalapril, an ACE-Is, 21 (05.3%) had Metoprolol, a β – blockers and 10 (02.6%) hadPrazosin, anα – blockers in their prescriptions.
These drugs were either prescribed as a single drug or in combination with other antihypertensive agents. If the combination therapy was being prescribed, then the Fixed Dose Combinations (FDCs) were preferred.
ARBs being the top on the list, which was prescribed to 164 cases either as a single drug or in combination with other antihypertensive agents, 32.9% of it, was prescribed in 51 – 60 years of age, 32.3% in 41 – 50 years, 20.1% in 31-40 years, 13.5% in 61 – 70 years. The single cases in each age group of 18 – 20 and 21 – 30 years received 0.6% of the share.Of 100 prescriptions with CCBs, 58 were in 51 – 60 years, 28 in 61 – 70 years and 14 in 41 – 50 years.In 77 prescriptions, diuretics were prescribed. 18.2% were in 41 – 50 years, 49.4% in 51 – 60 years and 32.4% in 61 – 70 years.Among 23 prescriptions with ACE-Is, 21.7% were in 41 – 50 years, 65.2% in 51 – 60 years and 13.1% in 61 – 70 years.21 prescriptions had β-blockers, 52.4% were in 51 – 60 years and the rest 47.6% in 61 – 70 years of age.α-blockers were prescribed to 10 cases of 51 – 60 years and 61 – 70 years. 5 in each age group received the same.
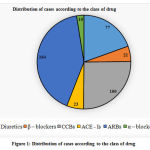 |
Figure 1: Distribution of cases according to the class of drug. |
Table 1: Distribution of cases according to the class of drug
| Class of drugs prescribed | Cases | Percentage |
| Diuretics (Hydrochlorothiazide) | 77 | 19.5 |
| β – blockers (Metoprolol) | 21 | 05.3 |
| CCBs (Amlodipine) | 100 | 25.3 |
| ACE – Is (Enalapril) | 23 | 05.8 |
| ARBs (Telmisartan) | 164 | 41.5 |
| α – blockers (Prazosin) | 10 | 02.6 |
| Total | 395 | 100 |
Distribution of Cases According to the Number of Drugs Prescribed
Table 2 shows distribution of study cases according to the total number of antihypertensive drugs prescribed. Among 200 cases, 88 cases were on monotherapy i.e., 44% cases were prescribed single antihypertensive agent. 47 cases (23.5%) were prescribed two antihypertensive drugs. Three and four drugs were prescribed to 46 (23%) and 19 (9.5%) cases respectively.
All cases upto 40 years of age were prescribed single antihypertensive drug. While among 41 – 50 years cases, 71.2% were on single drug, 11.9% were on two drugs and 16.9% were on three drug for the treatment of hypertension.In the age group of 51 – 60 years, 14.3% cases were prescribed one drug. 44.1% were on two drugs, 32.5% were on three drugs and 9.1% were on four antihypertensive drugs.In the 29 cases lying in the age group of 61 – 70 years, 20.7% were on two drugs for hypertension. 37.9% and 41.4% of cases were prescribed three and four antihypertensive drugs respectively.
Table 2: Distribution of cases according to the number of drugs prescribed
| No. of anti-HTN drugs prescribed | Cases | Percentage |
| One | 88 | 44 |
| Two | 47 | 23.5 |
| Three | 46 | 23 |
| Four | 19 | 9.5 |
| Total | 200 | 100.0 |
Distribution of Cases According to he Various Combinations of Drugs Used
Table 3 shows the distribution of study cases according to the various combinations of antihypertensive drugs used.Most commonly combined two drugs were from the class, CCB and ARB, used in 16.9% of total 112 patients on combination therapy.Major chunk of 35.7% in 112 prescriptions comprised of the combination of three drugs from the diuretic, CCB and ARB class of antihypertensive agents.α-blocker was used in combination with diuretic, CCB and ARB in 8.9% of the cases on multidrug therapy to control the raised BP.
Table 3: Distribution of cases according to the various combinations of antihypertensive drugs used
| Combinations of antihypertensive drugs | Cases | Percentage |
| CCB + ARB | 19 | 16.9 |
| Diuretic + ACE-I | 10 | 8.9 |
| CCB + ACE-I | 07 | 6.3 |
| β-blocker + CCB | 07 | 6.2 |
| Diuretic + ARB | 04 | 3.6 |
| Diuretic + CCB + ARB | 40 | 35.7 |
| Diuretic + β-blocker + ACE-I | 03 | 2.7 |
| β-blocker + CCB + ARB | 02 | 1.8 |
| Diuretic + CCB + ACE-I | 01 | 0.9 |
| Diuretic + CCB + ARB + α-blocker | 10 | 8.9 |
| Diuretic + β-blocker + CCB + ARB | 09 | 8.1 |
| Total | 112 | 100.0 |
Distribution of Cases According to the Associated Co-Morbidity
Table 4 shows distribution of study cases according to the associated co-morbid condition.Diabetes mellitus was the most common co-morbid disorder, associated in 39% of the study population with hypertension. Dyslipidaemia was associated in 24%, while 23.5% of the patients were obese.9% were having history of IHD and 5% were having CCF. Past history of stroke (CVD) was present on 1.5% of the cases, while 1% were asthmatics.In 78 cases of diabetes, only 48 (24%) cases were solely having DM. The remaining total of 36 (18%) cases were having dyslipidaemia and obesity along with DM.12 (6%) cases out of 18 were having dyslipidaemia and IHD both, while the remainder 6 cases (3%) were having history of only IHD.39% of the remaining cases were free from any associated co-morbid condition. All the patients with the association of co-morbid condition were on treatment of the respective disorder.
DM being the most commonly associated co-morbid condition, i.e. 78 cases in 200, 60.3% were from age group of 51 – 60 years. 20.5% in 61 – 70 years and 19.2% in 41 – 50 years age group were diabetics. Dyslipidaemia was the second most common disorder associated with hypertension. Out of 48 patients with the disorder, major chunk of 58.4% were in the age group of 51 – 60 years. In each age groups, 41 – 50 years and 61 – 70 years, 20.8% cases were having dyslipidaemia. Obesity followed dyslipidaemia in the total count which accounted for 47 cases. 44.7% cases were obese in the age group of 51 – 60 years. 21.3% cases were obese in 41 – 50 years of age. 17% obese lied in the age of 31 – 40 years and 12.8% in 61 – 70 years. The only single cases in each age groups of 18 – 20 and 21 – 30 years were found to be obese.In 18 patients of IHD, 55.6% were aged 61 and above while the remaining 44.4% were between 51 and 60 years of age.CCF was the co-morbidity in 10 cases, of which 7 were in 51 – 60 years and 3 in 41 – 50 years. History of stroke and bronchial asthma was found in 3 and 2 cases respectively.78 patients were not having any associated co-morbid condition.
Table 4: Distribution of cases according to the associated co-morbid condition
| Associated co-morbidity | Cases | Percentage |
| Diabetes mellitus (DM) | 78 | 39 |
| Ischemic heart disease (IHD) | 18 | 9 |
| Dyslipidaemia | 48 | 24 |
| Cerebrovascular disease (CVD) | 03 | 1.5 |
| Congestive cardiac failure (CCF) | 10 | 5 |
| Bronchial Asthma (BA) | 02 | 1 |
| Obesity | 47 | 23.5 |
| No co-morbidity | 78 | 39 |
Prescription Pattern of Drugs Among Associated Co-Morbidity
Table 5 shows prescription pattern of various classes of antihypertensive drugs among study cases with associated co-morbidity.
Out of total 78 patients of DM, 64.1% were on diuretics, 85.9% on CCB, 20.5% on ACE-Is, 85.9% on ARBs and 10.2% on α-blockers.All the 18 IHD patients were prescribed β-blockers and CCBs while 44.4% were having an addition of diuretics in their prescriptions.81.3% cases of dyslipidaemia were on diuretics, 25% on β-blockers, 87.5% on ARBs and 20.8% on α-blockers. CCBs were prescribed to all the patients of dyslipidaemia.The 3 patients with history of stroke were prescribed both diuretics and ACE-Is while both the asthmatics were prescribed CCB alone.Among the 10 patients of CCF, all were advised diuretics and ACE-Is. Two patients among them were additionally on β-blockers.Each and every obese individual was on ARBs. 76.6% of them were prescribed additional diuretic agent. CCBs were also one of the drug included in 76.6% of the prescriptions.In the 78 solely hypertensive individuals, without any co-morbidity, 96.2% were on ARBs, 16.7% on CCBs and 6.4% on diuretics.All these classes of drugs were either prescribed alone or in combination of two or more drugs.
Among 78 diabetics, 11.6% were on monotherapy, 26.9% on two drugs, 48.7% on three drugs and 12.8% on four drugs. 48 patients had dyslipidaemia, of which, 12.5% were on two drugs, 58.3% on three drugs and 29.2% on four drugs. All the 3 patients with history of stroke were on two antihypertensive drugs, while single drug was prescribed to both the asthmatics. Among the 10 cases of CCF, 7 received two drugs and the remaining 3 were prescribed three drugs for hypertension. Among 47 obese individuals, 57.4% received the combination of three drugs. Single drug was prescribed to 21.3% of obese cases. The rest 21.3% cases had four antihypertensive drugs in their prescriptions. 78 cases in 200 were not having any co-morbidity. 85.9% of them received only one antihypertensive drug whereas, 10.3% and 3.8% had two and three drugs in their prescriptions.
Table 5: Prescription pattern of various antihypertensive drugs among study cases with associated co-morbidity
| Associated co-morbidity
(n) |
Class of the antihypertensive drug prescribed | |||||||||||
| Diuretics | β – blockers | CCBs | ACE – Is | ARBs | α – blockers | |||||||
| n | % | n | % | n | % | n | % | n | % | n | % | |
| DM (78) | 50 | 64.1 | – | – | 67 | 85.9 | 16 | 20.5 | 67 | 85.9 | 08 | 10.2 |
| IHD (18) | 08 | 44.4 | 18 | 100 | 18 | 100 | – | – | 11 | 61.1 | – | – |
| Dyslipidaemia (48) | 39 | 81.3 | 12 | 25.0 | 48 | 100 | – | – | 42 | 87.5 | 10 | 20.8 |
| CVD (3) | 3 | 100 | – | – | – | – | 3 | 100 | – | – | – | – |
| CCF (10) | 10 | 100 | 2 | 20 | – | – | 10 | 100 | – | – | – | – |
| BA (2) | – | – | – | – | 2 | 100 | – | – | – | – | – | – |
| Obesity (47) | 36 | 76.6 | – | – | 36 | 76.6 | – | – | 47 | 100 | – | – |
| No co-morbidity (78) | 5 | 6.4 | – | – | 13 | 16.7 | – | – | 75 | 96.2 | – | – |
| Total | 77 | 19.5 | 21 | 05.3 | 100 | 25.3 | 23 | 05.8 | 164 | 41.5 | 10 | 02.6 |
Discussion
Hypertension is a long term disease condition with increasing prevalence world-wide as well as in India. However, the cause remains uncertain in many, grouping them under the tag of primary or essential hypertension. It’s an independent factor which predisposes to many morbidity leading to target organ damage. With the rise in BP levels, increased are the chances of mortality. The INTERHEART 6 and INTERSTROKE 7 study also revealed the same.
Hypertension, which was considered to be the disease of old age, is now commonly turning up in young adults between the age of 18 years and 40 years. This may be attributed to various risk factors. This younger age group living with the disease condition, may have a huge impact on the society with regards to the health and economic aspects of the nation. Thus, to prevent or to combat this disease condition, guidelines have been developed for management of hypertension.
Indian Hypertension Guidelines 4 suggest that gradual BP reduction should be done with low doses of drugs. Drugs of choice depends on the age of the patient, any concomitant co-morbidity, socio-economic considerations etc. Combination of two or more drugs in low doses may attribute synergism and cause fewer side effects. Since, the therapy for hypertension control is lifelong, fixed dose combinations with longer half-life should be considered to maintain the patients’ compliance.4
This study was conducted in 200 patients who had antihypertensive drugs advised in their prescriptions. Their prescriptions were studied to understand the pattern of prescriptions of the drugs to control hypertension.
Socio-Demographic Profile of Cases
In the present study, out of 200 patients, 115 (57.5%) were male and 85 (42.5%) were female.
The similar findings were observed in a study by Datta S. (2017)8 Also the studies by Sharma A et al (2017)9, Vashishta K. (2018)10 and Ajmery S et al (2017) 11. reported male predominance of hypertension. However, a study conducted by Oluseyi A et al (2017) 12 reported female preponderance, which was in contradiction to our study.
In our study, maximum number of hypertensive patients, i.e. 38.5% were in the age group of 51 – 60 years, followed by 29.5% in 41 – 50 years.
This finding of our study was in accordance with the studies by Sharma A et al (2017)9, Vashishta K. (2018)10 and Ajmery S et al (2017)11; where more than half of the patients were found to be hypertensive in the age group of 41 and above. But, Oluseyi A et al (2017)12 reported that individuals aged 60 years or more were hypertensive compared to less than 60 years. Sub-Saharan African study by Olanrewaju TO et al (2010)13 also concluded that hypertension is common disorder in the patients aged 51 – 60 years of age.
Two patients in our study, aged 20 and 29 years, were the only patients in the age group of 18 – 20 and 21 – 30 years respectively who were hypertensive. This finding was attributed to obesity in those individuals, which may be due to faulty food habits, as neither of them gave positive family history of obesity.
Concomitant Co-Morbid Conditions Among Cases
Diabetes mellitus was the most commonly associated co-morbidity in the hypertensive individuals. 39% of them were diabetic, of which 18% were obese and had dyslipidaemia. All these were common among males in the age group of 51 – 60 years. Other co-morbid conditions like IHD, CCF, stroke, bronchial asthma were also present in less than 17% of the study population in the age group of 41 – 70 years.
In agreement with Datta’s (2017)8 findings, diabetes was the most commonly associated disorder in patients with hypertension, as observed in this study as well as a study in north India by Sharma A. et al (2017).9
However, Datta S. (2017)8 stated that DM was followed by IHD, CVD, CCF, dyslipidaemia and asthma in decreasing order, while our study revealed that after diabetes, dyslipidaemia, obesity, IHD, CCF, CVD and asthma were prevalent in descending order.
It can be derived that, early control of hypertension and the associated co-morbid condition can improve the quality of life of the patients by reducing their risk of morbidity and mortality.
Prescribing Pattern of Antihypertensive Drugs
ARBs were the most commonly prescribed antihypertensive class of drugs i.e. 41.5% among the total drugs prescribed, either as single drug or in combination. This was followed by CCBs (25.3%), diuretics (19.5%), ACE-Is (5.8%), β – blockers (5.3%) and α – blockers (2.6%). Combination of two or more drugs was prescribed in 56% of the cases i.e. 112 cases, whereas 44% prescriptions were having a single antihypertensive drug. Among these 56% individuals, the combination of diuretic, CCB and ARB was the most commonly prescribed. 35.7% of the prescriptions were having this combination. This was followed by the prescriptions having CCB and ARB accounting for 16.9%. α-blocker was used along with diuretic, CCB and ARB in 8.9% of the cases on multidrug therapy.
It was also observed in our study that, 85.9% of the diabetics received ARBs and CCBs, while 64.1% were on diuretics.Telmisartan was the prescribed drug among the ARBs. The ONTARGET14trial also concluded that the use of Telmisartan is beneficial in diabetic patients. Also, the ASCOT 15trial summarizes that, the use of Amlodipine, a CCB, which was the drug prescribed in the present study from this class and Perindopril, an ACE-I are cardioprotective and also reduces the new-onset diabetes mellitus and renal impairment along with decreasing the BP.
All the patients who had altered lipid levels received CCBs. 87.5% additionally received ARBs and diuretics were prescribed in 81.3% of them. Indian Guidelines On Hypertension4also recommends the use of CCBs & ACE-Is in the patients with hypertension in dyslipidaemia. ARBs were ordered in all the obese individuals. Inclusion of diuretics and CCBs were done in 76.6% of the obese.
Everyone suffering from IHD were advised β-blockers and CCBs, which was in lines with Indian Guidelines On Hypertension 4. The CAPEstudy 16 also suggests that Amlodipine reduces the cardiovascular mortality and morbidity. ARBs and diuretics were prescribed in 61.1% and 44.4% of the IHD patients, respectively. All the patients of stroke and heart failure received diuretics and ACE-Is, while both asthmatics in the study were prescribed the CCBs. 96.2% of the individuals exclusively having hypertension were advised ARBs, whereas CCBs were prescribed to 16.7% of them. Only 6.4% of them received diuretics.
Datta S. (2017)8 concluded that CCBs were the most commonly used antihypertensive drug and the combination of drugs was most frequently prescribed rather than a single drug. Also, Sharma A. et al (2017)9 quotes that multidrug therapy was more commonly advised than monotherapy, but diuretics were the most prescribed drugs followed by CCBs. Except the class of the drug used commonly, our study is in agreement with theirs in regards to the number of drugs prescribed.
This south Indian study (2017)8 mentions that CCBs appeared repeatedly in 64.8% of prescriptions of diabetics, which is closely equivalent to our study results. Nevertheless, ARBs and diuretics were less commonly advised in diabetics. It also reported that the usage of CCBs was in 63.6% of patients with dyslipidaemia, which goes along with our finding. However, the percentage of ARBs and diuretics in their prescription is dissimilar to that of ours.
Datta S. (2017)8 also states that CCBs were advised in 73% of IHD patients which is close to our finding, but β-blockers were used in just 37.1% of IHD patients which is distinct from our reports. The south Indian patients (2017)8 with CCF were often prescribed diuretics (93.7%) followed by β-blockers (75%), which is partially analogous to our findings of using diuretics in CCF patients. Furthermore, usage of CCBs in asthmatics is kindred with our study.
A study in Jammu (2012)17also observed that combination therapy was the most commonly prescribed in which, majority had CCB and ACE-I, which is distinct from our study. ACE-I was the commonly prescribed class of drug, which also contradicts our study findings.
Vashishta K. (2018)10 studied that monotherapy was more common than multidrug therapy for hypertension, with intensive prescription of CCBs. This finding in Telangana (2018)10 counters that of ours. Also, they stated that the combination of ARB and diuretic was frequent, which is in contrast to our results.
The study in Nigeria, by Oluseyi A et al (2017)12 reported that the multidrug therapy was common and diuretics was the frequently used class of drug. Similar findings were reported by Bakare OQ et al (2016)18in Nigeria itself. Oluseyi A et al (2017)12 also averred that diuretics were combined with ACE-I or ARB very habitually. However, these findings were different in a way when compared to ours.
In agreement to our study findings, Ajmery S. et al (2017)11 had similar results i.e. combination therapy was common and ARBs were the most frequently prescribed drugs.
The variations in these studies may be chalked up to numerous factors; namely age and sex of the patients, various concomitant disorders and the drugs used for them, socioeconomic aspects etc. Aiming at control of raised BP, consideration of all these factors were done in addition to compliance with drug treatment, cogitating safety and efficacy of the drugs being prescribed.
Conclusion
Hypertension is becoming evident in the younger age group. Combination of drugs were used most commonly to keep check on the raised blood pressurePrescribing pattern of antihypertensive drugs seemed to be specific to the age and associated co-morbidity.The pattern of the prescribed drugs was in accordance with the recommended national and international guidelines including the Indian Guidelines on Hypertension.However, a large number of population needs to be studied with regards to the cost burden on the patient and the adherence of the patient to the prescribed treatment, as compliance to the treatment is most important.
Acknowledgement
We are thankful to the staff of Department of Medicine for the support provided
Conflict of Interest
There are no conflicts of interest.
Funding Source
There are no funding Source
References
- Brunton LL. Goodman and Gilman’s The Pharmacological Basis of Therapeutics. 13th New York: McGraw Hill Education Pvt. Ltd; 2018. Thomas Eschenhagen. Chapter 28, Treatment of Hypertension; p. 507-526.
- Kasper DL. Harrison’s Principles of Internal Medicine. 19th USA: McGraw Hill Education;2015. Kotchen TA. Chapter 298, Hypertensive Vascular Disease; p.1611.
- Whelton PK, et al. Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults, Journal of the American College of Cardiology (2017), doi: 10.1016/j.jacc.2017.11.006.
CrossRef - Shah S. Special Issue On Indian Guidelines On Hypertension (I.G.H.)-III. Supplement to JAPI. 2013Feb;61:12-13.
- Abramson, J.H. WINPEPI updated: computer programs for epidemiologists, and their teaching potential. Epidemiologic Perspectives & Innovations 2011, 8:1.
CrossRef - Yusuf S. et al; Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. The Lancet 2004;364(9438):p937-952.
CrossRef - O’Donnell MJ et al. Global and regional effects of potentially modifiable risk factors associated with acute stroke in 32 countries (INTERSTROKE): a case-control study. The Lancet 2016;388(10046):p761-775.
CrossRef - Datta S. Utilization Study of Antihypertensives in a South Indian Tertiary Care Teaching Hospital and Adherence to Standard Treatment Guidelines. J Basic Clin Pharma 2017;8:33-7.
CrossRef - Sharma A. et al. Drug utilization Study on Oral Hypertensive Medication Patients and Assessment of Medication Adherence to JNC-8 Guidelines in North Indian Tertiary Care Hospital: A Cross-Sectional Study. RRJHCP 2017;3(3):5-12.
CrossRef - Vashishta K. Study on drug utilization pattern of antihypertensive medication in tertiary care hospital of Telangana, India. Int J Basic ClinPharmacol2018;7:1770-4.
CrossRef - Ajmery S.et al.Pattern of Anti-hypertensives Usage in Hypertension with or without Comorbidities in a Tertiary Care Hospital.Mymensingh Med J. 2017 Jan;26(1):80-86.
- Oluseyi A. et al. Prescription pattern of antihypertensive medications and blood pressure control among hypertensive outpatients at the University of Benin Teaching Hospital in Benin City, Nigeria. Malawi Med J. 2017 Jun;29(2):113–117.
CrossRef - Olanrewaju TO et al. Antihypertensive drug utilization and conformity to guidelines in a sub-Saharan African hypertensive population.Int J ClinPharmacolTher. 2010 Jan;48(1):68-75.
CrossRef - The ONTARGET investigators. Telmisartan, Ramipril or Both in patients at High Risk for Vascular events. NEJM 2008; 358:1547-1559.
CrossRef - Dahlöf B, Sever PS, Poulter NR, Wedel H, Beevers DG, Caulfield M, et al for the ASCOT investigators. Prevention of cardiovascular events with an antihypertensive regimen of amlodipine adding perindopril as required versus atenolol adding bendroflumethiazide as required, in the Anglo-Scandinavian Cardiac Outcomes Trial-Blood Pressure Lowering Arm (ASCOT-BPLA): a multicenter randomised controlled trial. Lancet 2005;366:895-906.
CrossRef - Detry JM. Amlodipine and the total ischemic burden: circadian anti-ischemia program in Europe (CAPE) trial-methodology, safety and toleration. The Steering Committee members and all of the investigators. Cardiology. 1994;85 Suppl 2:24-30. doi:10.1159/000177044
CrossRef - Dinesh K. et al. Prescribing pattern of antihypertensive drugs in a tertiary care hospital in Jammu- A Descriptive study.JK-Practitioner 2012;17(4):38-41.
- Bakare OQet al. Antihypertensive use, prescription patterns, and cost of medications in a Teaching Hospital in Lagos, Nigeria. Niger J ClinPract2016;19:668-72.
CrossRef








