Sreeshyla HS , Priyanka Nitin,
, Priyanka Nitin, Usha Hegde,
Usha Hegde, Vidya Gowdappa Doddawad
Vidya Gowdappa Doddawad  and Premalatha Bidadi Rajashekaraiah
and Premalatha Bidadi Rajashekaraiah
Department of Oral Pathology and Microbiology, JSS Dental College and Hospital, A Constituent College of JSS AHER, Mysuru, Karnataka, India.
Corresponding Author E-mail: sreeshylahs@gmail.com
DOI : https://dx.doi.org/10.13005/bpj/2207
Abstract
The clinical presentation of typical lipomas is often characteristic. But the variations of lipoma based on the associated stroma poses a challenging picture with clinical diagnosis varying from benign tumors, various inflammatory and reactive lesions, salivary gland lesions, to few peripheral odontogenic lesions. Only a thorough clinical and pathological evaluation and correlation will help in arriving at a conclusive diagnosis, in understanding the behaviour, planning the treatment and predicting the prognosis of the lesion. One such case of lipoma presenting as an unassuming swelling clinically, but showing exuberant vascular component occurring on buccal mucosa is presented. A review of this variant of lipoma is discussed in comparison with the present case.
Keywords
Angiolipoma; Lipoma; Neoplasm; Oral Tumor; Vascular
Download this article as:| Copy the following to cite this article: Sreeshyla HS, Nitin P, Hegde U, Doddawad V. G, Rajashekaraiah P. B. Non Infiltrating Oral Angiolipoma – Report of A Rare Case with Review. Biomed Pharmacol J 2021;14(2). |
| Copy the following to cite this URL: Sreeshyla HS, Nitin P, Hegde U, Doddawad V. G, Rajashekaraiah P. B. Non Infiltrating Oral Angiolipoma – Report of A Rare Case with Review. Biomed Pharmacol J 2021;14(2). Available from: https://bit.ly/3AyPbLW |
Introduction
Angiolipomas are benign tumors of adipocytic origin with marked degree of vascularization.1,2 It was first reported by Bowen in 1912. They represent 6% to 17% of all lipomas.3 Angiolipoma occurs most commonly among young people usually involving trunk and extremities. It is rarely seen in the head and neck region.1
Case History
A male patient aged 64 years reported to the hospital with a complaint of swelling and pain over right buccal mucosa since 15 days. The swelling was associated with difficulty in chewing and dryness of the mouth. Clinical examination revealed a solitary, soft non-tender, non-pulsatile swelling on right buccal mucosa extending antero-posteriorly from 46 to ramus region. Mucosa overlying the swelling was normal in colour with no areas of pigmentation, ulceration or sinus opening. There was no local rise of temperature and salivary duct orifice was patent. Patient was diabetic and hypertensive since 8 months and was under medication for the same. Extraoral examination showed no gross facial deformity. Regional lymphnodes were not palpable.
A provisional diagnosis of lipoma was made with leiomyoma, neurilemmoma and epidermoid cyst as differential diagnosis. Surgical excision of the lesion was done. The gross specimen was yellow to creamish white in colour and soft in consistency [Figure 1]. Microscopically the tissue sections revealed epithelium and connective tissue stroma. Epithelium was parakeratinized stratified squamous in nature. Connective tissue stroma consisted of well circumscribed tumor mass composed of sheets of adipocytes amidst numerous blood vessels, proliferating endothelial cells, hemorrhagic areas and few mast cells. The lesion was very well contained and circumscribed, however, a definite capsule could not be appreciated [Figure2,3]. Scant inflammatory cells were noted. Based on the histopathological features, a final diagnosis of angiolipoma was given. Patient was under regular follow up and is disease free since 4 years.
Discussion
Lipomas are the most common neoplasms arising from adipose tissue. They usually show slow growth, are soft in nature and appear as asymptomatic masses with about 13% prevalence in the head and neck region including tongue, palate, cheek, parotid gland, neck and larynx.4,5 They account for about 1–5% of all neoplasms of the oral cavity. Benign lipomatous tumors include classic lipoma, lipoma variants, hamartomatous lesions, diffuse lipomatous proliferations and hibernomas.6,7 The lipomas are subclassified into angiolipoma, spindle cell lipoma, chondrolipoma, myelolipoma, myxolipoma, myolipoma, and lipoblastoma/lipoblastomatosis based on the associated stromal components.4,8
Lipoma with predominant vascular components are entitled as Angiolipoma.1,8 They account for 6% to 17% of all lipomas and rarely occur in the head and neck region.3 They are predominantly seen on the forearms, upper arms, thighs and anterior abdominal wall and occur rarely on face, scalp, palms and soles.9 Intraorally they have affinity for occurrence on buccal mucosa and lip.1,5 Their occurrence is also reported in palate, tongue, salivary gland and intraosseously in the jaws.1,4,6 Angiomyolipoma, angiofibrolipoma and sialoangiolipomas admixed with muscle, fibrous and glandular component respectively are stated.1,5,8
Although angiolipomas are noted in mean age of 37 years, their occurrence is reported in a wide age range from 4 months to 76 years.1,4 The lesion shows an equal gender predilection, however, a male to female ratio of 1.4:1 has been reported.1,3 They usually present clinically as painless, well-defined, non-ulcerated, soft, round, mobile, subcutaneous mass and rarely can present with a polypoid morphology.3,4 They are usually tender on palpation, predominantly during the initial growth period.7 The size of well encapsulated angiolipomas can vary from 1 to 4 cm.9 Angiolipoma needs to be differentiated from haemangioma, lymphangioma, lipoma, leiomyoma, mucocele, neurilemmoma, kaposi’s sarcoma and liposarcoma.2,4,9 In our case a painful lesion on buccal mucosa was presented in a 64year old male patient.
Angiolipomas can be infiltrating or non-infiltrating type. Non-infiltrating is the more common type, is encapsulated, usually occurs in younger individuals and doesn’t show any recurrence.2,4,9 It has occurred in multiple sites in 79% of cases.7 Infiltrating angiolipoma is rare with infiltration of the surrounding structures, predominantly the skeletal muscle.7 They are non-encapsulated, occur in older individuals, usually recur after surgery and has shown high recurrence in 35 to 50% of cases. Intermuscular and intramuscular are the two anatomical variants. They occur most commonly in the trunk and extremities. Very few cases are reported in the head and neck region but are extremely rare in oral cavity. Documented sites of head and neck region are palate, cheek, tongue, jaw, neck, parotid, nose, eyelid, paranasal sinuses, and parapharynx.4 Infiltrating angiolipomas can also lead to muscular pain and neural deficits.4 Its behaviour mimics a locally aggressive tumor.7 The present case was a non-infiltrating type of angiolipoma.
The etiology and pathogenesis of angiolipoma is not clear. Factors like history of trauma, vascular transformation in congenital lipoma, lipomatous hormonal differentiation during puberty, central hemangioma undergoing fatty degeneration, hyperplasia of fat associated with an increase in vascular spaces, diabetes mellitus induced by hypercholesterolaemia and obesity, or a true neoplasm, familial or genetic link such as abnormality of chromosome 12 and radiation are considered.2,3,5,9 Another theory states that an angiolipoma initially originates as a congenital lipoma and later it undergoes vascular proliferation. This theory has gained more support due to the considerable correlation of etiopathogenesis with that of histopathology and disease behaviour. The hormones at puberty may bring about embryonic sequestration of multipotential cells that differentiate into a simple lipoma.5 In case of trauma induced etiology, adipose tissue may prolapse through fascia after trauma resulting in a direct impaction or it can be result of soft tissue trauma that induces haematoma formation, followed by cytokines mediated differentiation which causes proliferation of preadipocytes, activating to adipocytes, deposition of adipose tissue, resulting further in lipoma formation. However, trauma is not a common finding in many cases of angiolipoma.5 No obvious etiology could be elicited in the present case.
Very few mast cells were noted in our case and literature indicates that they are usually found in angiolipoma and are localized around blood vessels and adipocytes. The available reports suggest that there are 10 times higher mast cells in angiolipomas than classic lipomas.3,5,6 The mast cells are usually present surrounding the blood vessels, they express high levels of VEGF. VEGF is an essential growth factor for vasculogenesis.5,7 It is also speculated that these mast cells are responsible for simultaneous expression of factors such as VEGF, IFN-γ, TNFα, IL6 and ICAM-1. This might suggest that the morphological features observed in these tumors could be associated with inflammatory stimuli that is mediated by mast cell-derived endothelial alteration and followed subsequently by leukocyte transmigration.3
Histopathologically, although there is definite evidence of tumor formation, the presence of capsule is not mandatory. Characteristically the mature lipocytes form 50% of the tumor. The tumor also shows 15%–40% of angiomatous proliferation consisting of many small to medium sized congested blood vessels having fibrin thrombi. The endothelial cells may be plump and there may be presence of numerous mast cells.3,4,6,9 The angiomatous element is predominantly present in the subcapsular peripheral areas.3 Its hypothesized that a simple lipoma may eventually transfom into angiolipoma through capillary and fibrous proliferation from the periphery.6 Histologically the non infiltrating and infiltrating type are similar, however, the later may have no identifiable capsule and rarely, there may be pleomorphism, atypia, or mitotic figures.4,9 Histological features in our case were similar to as mentioned above, indicating of non infiltrating angiolipoma.
The treatment of choice for angiolipomas is the surgical excision.9 As infiltrating angiolipomas demonstrate high risk of recurrence, wide resection is recommended.7 Radiotherapy is advisable in cases of inadequate excision.2 The other alternative treatment involves the use of carbon dioxide laser or liposuction.9 Recurrence varies with the type. While non-infiltrating type show better prognosis, the infiltrating type can recur and the recurrence rate is 35–50%. There is no evidence of malignant transformation.9 Our case was treated with surgical excision and the follow up of the case since 4 years is uneventful.
 |
Figure 1: Macroscopic Appearance of the Specimen. |
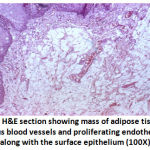 |
Figure 2: H and E section showing mass of adipose tissue with numerous blood vessels and proliferating endothelial cells along with the surface epithelium (100X) |
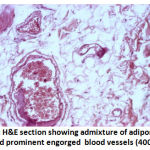 |
Figure 3: H and E section showing admixture of adipose tissue and prominent engorged blood vessels (400X) |
Conclusion
As angiolipomas of the head and neck are rare, the comprehensive clinical data is sparse. The present case adds yet another case of non-infiltrating angiolipoma to the literature. However, the molecular mechanism needs to be explored to understand this lesion better. The recommended treatment of surgical excision as treatment in the present case sufficed and the follow up of the case for 4 years has been uneventful.
Acknowledgement
None
Conflict of Interest
None
Funding Source
None
References
- Shetty S.R, Al-Bayati S.A.A.F, Khazi S.S and Manchala S.R. Clinical features of oral angiolipoma-A review. Romanian journal of military medicine., 2017; CXX: 22-26.
- Chandrasekaran D, Chinna Swami R, Narasimhan M, Kumar A.E.N and Natarajan P. Non Infiltrating Angiolipoma of the Palate in Geriatric Patient: A Case Report with Review of Literature. Journal of Clinical and Diagnostic Research., 2016; 10(1): ZD01-ZD02.
CrossRef - Silva-Junior G.O, Picciani B.L, Costa R.C, Barbosa S.M, Silvares M.G and Souza R.B et al., Oral soft-tissue angiolipoma: report of two cases of rare oral lipomatous lesion with emphasis on morphological and immunohistochemical features. Journal of Oral Science., 2013; 55: 85-88.
CrossRef - Shahi A.K, Ash H, Chatterji K and Singh R. Cellular infiltrative angiolipoma of cheek in an infant. Natl J Maxillofac Surg., 2014; 5: 202-5.
CrossRef - Sah K, Kadam A, Sunita J.D and Chandra S. Noninfiltrating angiolipoma of the upper lip: A rare entity. J Oral Maxillofac Pathol., 2012; 16: 103-6.
CrossRef - Hemavathy S, Roy S, Kiresur A. Intraosseous angiolipoma of the mandible. J Oral MaxillofacPathol., 2012; 16: 283-7.
CrossRef - Ohnishi Y, Watanabe M, Fujii T, Yasui H, Kubo H and Kakudo K. Infiltrating angiolipoma of the lower lip: A case report and literature review. Oncology Letters., 2015; 9: 833-836.
CrossRef - Brkic A, Ozcamur C, Gürkan-Koseoglu B, Olgac V. Angiofibrolipoma of the buccal mucosa: a case report. Journal of Oral Science., 2010; 52: 173-176.
CrossRef - Shah V.S, Harish M, Patel J.R and Shah N. Infiltrating angiolipoma of the cheek. BMJ Case Rep. 2013;1-5 doi:10.1136/bcr-2013-200041.
CrossRef








