Monika Reddy1 , Dr Ranganath Gangavelli2
, Dr Ranganath Gangavelli2 , Priyanka1
, Priyanka1 and Dr P Saikiran1*
and Dr P Saikiran1*
1Department of Medical Imaging Technology, Manipal College of Health Professions, Manipal Academy of Higher Education, Manipal, Karnataka, India.
2Department of Physiotherapy, Manipal College of Health Professions, Manipal Academy of Higher Education, Manipal, Karnataka, India.
Corresponding Author E-mail : saikiran.p@manipal.edu
DOI : https://dx.doi.org/10.13005/bpj/2203
Abstract
Lumbar spinal stenosis (LSS) is abnormal narrowing of spinal canal of lumbar vertebrae causing compression of neural tissue which leads to a neurologic deficit. LSS is diagnosed based on clinical symptoms of patient and it is confirmed using MRI (Magnetic Resonance Imaging). The aim of the study is to determine the association between MRI lumbar spinal canal and foraminal dimensions in on neurological claudication symptomology. A total of 89 patients (45 males ,44 females, age range: 20-60 years) referred for MRI Lumbar spine were included in this prospective study. Patients were categorized into symptomatic (49 cases) and asymptomatic (40 controls) based on Edinburgh claudication questionnaire (ECQ). The Antero-posterior diameter of dural sac, Transverse diameter of dural sac, Cross sectional area of dural sac, Cross sectional area of lateral recess, Lateral recess depth, Angle of lateral recess, Ligamentous interfacet distance was measured from L3 to S1 on Axial T2 weighted MRI images. The strength of association between MRI measurements and clinical symptoms were assessed using logistic regression analysis and Cramer’s V test. The Phi coefficient value for the lumbar spinal canal, foraminal dimensions with neurogenic claudication symptomology based on ECQ was 0.108 & 0.207 respectively, which showed weak positive correlation. Our study concludes that MRI measurements of lumbar spinal canal and foraminal dimensions denoting LSS were found to show weak positive correlation with clinical symptoms assessed based on Edinburgh claudication questionnaire.
Keywords
Forminal Stenosis; Lumbar Spinal Stenosis; Lumbar Spine; Magnetic Resonance Imaging; Neurogenic Claudication
Download this article as:| Copy the following to cite this article: Reddy M. M, Gangavelli R, Priyanka P, Saikiran P. Influence of Lumbar Spinal Canal Dimensions on Neurological Claudication Symptomatology- A Case Control Study. Biomed Pharmacol J 2021;14(2). |
| Copy the following to cite this URL: Reddy M. M, Gangavelli R, Priyanka P, Saikiran P. Influence of Lumbar Spinal Canal Dimensions on Neurological Claudication Symptomatology- A Case Control Study. Biomed Pharmacol J 2021;14(2). Available from: https://bit.ly/3xkqfWv |
Introduction
Spinal canal in each vertebrae allows the passage of spinal cord. Lumbar spinal stenosis (LSS) is abnormal narrowing of the spinal canal of lumbar vertebrae causing compression of neural tissue which leads to a neurologic deficit. stenosis is divided into two types central and lateral. Central stenosis is caused by the compression of Dural sac whereas lateral stenosis is caused by compression of nerve root in lateral recess in neural foramen. LSS is caused due to congenital, degenerative or combination of both. It will also be caused due to thickening of ligaments and bulging of discs. Spinal stenosis more often in women than in men.1-5 Neurogenic claudication is a common symptom of LSS which causes impingement or inflammation of nerves arising from the spinal cord. In some cases, it is precipitated by walking or prolonged standing which can be relieved by sitting and get worse while lumbar extension. 6,7
LSS is diagnosed based on the clinical symptoms of the patient and it is confirmed using MRI. The antero-posterior diameter of spinal canal measuring 12 mm on MRI considered as ‘relative stenosis’ where less than 10 mm is the ‘absolute or definitive stenosis’. However, recent studies have stated that patients with symptoms of LSS have normal canal diameter and require correlation with clinical symptoms for improving the diagnosis of LSS. 8-14 Hence, this study was undertaken to determine the association between lumbar spinal canal and forminal dimensions on neurological claudication symptomatic and asymptomatic patients.
Materials and Methods
The current study was case control cross sectional prospective study conducted in Department of Radio diagnosis and Imaging on patients who were referred for MRI Lumbar spine. The study approval was obtained from Institutional Research Committee and Institutional Ethics Committee (IEC: 65/2018), CTRI/2019/07/020192.
A total of 89 patients with age ranging from 20 to 60 years were included in the study. The patients were divided into cases and controls based on Edinburgh claudication questionnaire (ECQ). The cases were symptomatic patients having symptoms of neurogenic claudication and the controls were asymptomatic patients without symptoms of neurogenic claudication. Patients with surgical history of spine, diagnosed spinal anomalies, scoliosis, history of spinal trauma, and pott’s spine were excluded from the study. Informed consent was obtained from all the patients in English and local language.
Magnetic Resonance Imaging Measurements
MRI Lumbar spine was performed on 1.5 Tesla (Signa HDxt 1.5 T, GE Healthcare). Standard protocol included Sagittal T2, T1, Short Tau Inversion Recovery (STIR) and Axial T1, T2 images.
The axial T2 images were transferred to Picture Archiving and Communication System (PACS) Monitor. All measurements were done from on Axial T2 weighted images at the disc level from L3-S1 Vertebrae using measurement tools. The linear measurements were noted in millimeters (mm), angle in degrees, and area is measured in millimeter square (mm2).
The Following MRI Measurements were Done on Axial T2 Images
Antero-posterior diameter of dural sac was measured as distance between centre of vertebral body and middle of spinous process at the dural sac border. Transverse diameter of dural sac was measured as the distance between the lateral end of dural sac at lateral recess. Ligamentous intrafacet distance was measured as distance between the inner part of ligament joining space of facet joints. Lateral recess depth was measured as distance between superior process and pedicle upper part. Lateral recess angle was measured as the angle between the lines passing parallel through the upper and lower end of lateral recess [Figure 1]. Cross sectional area of dural sac and right and left lateral canals were measured on Axial images as shown in Figure 2.
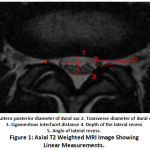 |
Figure 1: Axial T2 Weighted MRI Image Showing Linear Measurements. |
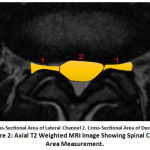 |
Figure 2: Axial T2 Weighted MRI Image Showing Spinal Canal Area Measurement. |
The measurements were taken by two readers who were blinded to the symptoms and measured at different time periods. All the measurements taken were compared with the gold standard cutoff values to determine status of stenosis at each level of spine and categorized as stenotic and non-stenotic patients (Table 1).
Table 1: Showing the Cut – off Values for MRI Measurements from Literature.
| MRI Measurements | Cut-Off Values from Literature |
| AP diameter of dural sac | < 10 mm (absolute stenosis) (9) (13) (16) |
| Transverse diameter of dural sac | < 15 mm (16) |
| Cross-sectional area of dural sac | <100 mm2 (9) (16) |
| Cross-sectional area of lateral recess | – |
| Ligamentous interfacet distance | < 12 mm (10) (13) |
| Depth of lateral recess | < 3.6 mm (13) |
| Angle of lateral recess | < 30º (10) (13) (16) |
Statistical Analysis
The statistical analysis for data was performed using Statistical Package for Social Sciences (SPSS) version 20.0. The strength of association between clinical symptoms and MRI measurements were assessed using logistic regression analysis and Cramer’s V test. Intra and Interobserver variability of MRI measurements were performed using students t-test and kappa value
Results
A total of 89 patients (45 males and 44 females, mean age 40±10.1 years) were included in this study. Based on the ECQ, 49 were found to be symptomatic (cases) and 40 were found to be asymptomatic (controls). In symptomatic patients 38 had unilateral claudication, 11 had bilateral claudication (Table 2). The mean and standard deviation for the MRI measurements at three different levels were given in (Table 3).
Table 2: Distribution of Claudication in Symptomatic Patients.
| Claudication Side | No. of Patients |
| Right unilateral | 17 |
| Left unilateral | 21 |
| Bilateral | 11 |
Table 3: Mean and Standard Deviation of all the MRI Measurements at Three Different Levels of Lumbar Spine.
| MRI Variable | Level of spine | Mean ± SD | p-value | |
| Controls | Cases | |||
| AP diameter of dural sac (mm) | L3-L4 | 11.3 ± 1.8 | 10.1 ± 2 | < 0.0668 |
| L4-L5 | 10.3 ± 3.1 | 8.2 ± 2.9 | < 0.0816 | |
| L5-S1 | 9 ± 2.8 | 8.5 ± 3.09 | < 0.0431 | |
| Transverse diameter of dural sac (mm) | L3-L4 | 15.9 ± 2.5 | 14.8 ± 3.1 | < 0.0875 |
| L4-L5 | 14.2 ± 3.5 | 11.3 ± 4.4 | < 0.0936 | |
| L5-S1 | 11.8 ± 4.1 | 11 ± 4.4 | < 0.0749 | |
| Cross-sectional area of the dural sac (mm2) | L3-L4 | 131 ± 36 | 110 ± 37 | < 0.0835 |
| L4-L5 | 114 ± 51 | 87.5 ± 42 | < 0.0966 | |
| L5-S1 | 100 ± 51 | 84 ± 50 | < 0.0873 | |
| Left Cross-sectional area of the lateral recess (mm2)
|
L3-L4 | 35 ± 17 | 28 ± 15.9 | < 0.0677 |
| L4-L5 | 31.8 ± 26 | 21.5 ± 19 | < 0.0960 | |
| L5-S1 | 70.7 ± 42 | 52 ± 44.4 | < 0.0881 | |
| Right cross-sectional area of the lateral recess (mm2) | L3-L4 | 35.7 ± 15 | 27.1 ± 16.7 | < 0.0635 |
| L4-L5 | 27.3 ± 22 | 18.5 ± 18.3 | < 0.0724 | |
| L5-S1 | 61.9 ± 37.9 | 47.1 ± 39.7 | < 0.0716 | |
| Left Depth of the lateral recess (mm) | L3-L4 | 5 ± 1.6 | 4.1 ± 1.4 | < 0.0835 |
| L4-L5 | 4.3 ± 2.6 | 3.5 ± 2.5 | < 0.0766 | |
| L5-S1 | 3.5 ± 1.3 | 3 ± 1.7 | < 0.8831 | |
| Right Depth of the lateral recess (mm) | L3-L4 | 4.2 ± 1.3 | 3.6 ± 1.2 | < 0.9354 |
| L4-L5 | 3.6 ± 2 | 2.8 ± 2.2 | < 0.7356 | |
| L5-S1 | 3.4 ± 1.7 | 3.1 ± 1.8 | < 0.0963 | |
| Left Angle of the lateral recess (0) | L3-L4 | 40.3 ± 10.7 | 33.6 ± 14.4 | < 0.0871 |
| L4-L5 | 34.5 ± 18.5 | 27.3 ± 20.7 | < 0.8752 | |
| L5-S1 | 46.5 ± 10.7 | 36.3 ± 19.1 | < 0.5494 | |
| Right Angle of the lateral recess (0) | L3-L4 | 39.4 ± 11.7 | 33 ± 15.4 | < 0.7547 |
| L4-L5 | 35 ± 18.2 | 22.6 ± 20 | < 0.0854 | |
| L5-S1 | 45.3 ± 13.4 | 36.4 ± 19.9 | < 0.7168 | |
| Ligamentous interfacet distance (mm) | L3-L4 | 12.8 ± 1.7 | 11.7 ± 1.8 | < 0.8666 |
| L4-L5 | 13 ± 3.1 | 12.3 ± 2.3 | < 0.0749 | |
| L5-S1 | 13.4 ± 2.5 | 12.5 ± 3.7 | < 0.8831 | |
Based on MRI Lumbar spinal canal measurements in symptomatic cases 45 were found to be stenotic and 4 were found to be non-stenotic whereas in asymptomatic cases 34 were found to be stenotic and 6 were found to be non-stenotic (Table 4). Based on MRI Forminal measurements in symptomatic cases 47 were found to be stenotic and 2 were found to be non-stenotic where as in asymptomatic cases 34 were found to be stenotic and 6 were found to be non-stenotic (Table 5).
Table 4: Showing Classification of Symptomatic and Asymptomatic into Stenotic and Non-Stenotic based on Lumbar Spinal Canal Dimensions.
| MRI Measurements (Based on Lumbar spinal canal dimensions) |
Edinburgh Claudication Questionnaire | |
| Symptomatic (n=49) |
Asymptomatic (n=40) |
|
| Stenotic | 45 | 34 |
| Non-stenotic | 4 | 6 |
Table 5: Showing Classification of Symptomatic and Asymptomatic into Stenotic and Non-Stenotic based on Forminal Dimensions.
| MRI Measurements (Based on Foraminal dimensions) |
Edinburgh Claudication Questionnaire | |
| Symptomatic (n=49) |
Asymptomatic (n=40) |
|
| Stenotic | 47 | 34 |
| Non-stenotic | 2 | 6 |
The Phi coefficient value between the lumbar canal dimensions with neurogenic claudication symptoms based on ECQ was 0.108, which showed weak positive correlation.
The Phi coefficient value between foraminal dimensions with neurogenic claudication symptoms based on ECQ was 0.207, which showed weak positive correlation.
The kappa value was 0.81, which showed agreement of MRI measurements between two readers. There was no statistical difference for the MRI measurements done by Reader as per Student’s t-test.
Discussion
Lumbar spinal stenosis is a most commonly occurring disease in elderly patients affecting their life style and daily activities and it get worsen by time. MRI has become the prime investigation chosen for the diagnosis of LSS because of its better differentiation between the soft tissues. The criteria for diagnosing lumbar spinal stenosis still didn’t develop.8 Recent literature suggested that patients with symptoms of LSS have normal canal diameter and require correlation with clinical symptoms for improving the diagnosis of LSS. 12,13
In our study we measured the association between MRI lumbar spinal canal, foraminal measurements and Clinical symptoms in determining lumbar spinal stenosis.
In our study we used Edinburgh Claudication Questionnaire which had depiction of body chart of lower extremities and found to be helpful in localizing the pain through marking on the diagram by the subjects.
In our study we found weak association between the clinical symptoms and MRI measurements of Lumbar spinal canal and foraminal dimensions in determining lumbar stenosis. Both the symptomatic as well as asymptomatic patients were found to have stenotic measurements. The findings of our study are concordant with the results of study done by Geeta Anasuya et al.9, Ratnakar E Ambade et al.10, Janardhana et al.11, Genvay et al.12 They also reported that correlation of clinical parameter and MRI measurements may not be true in all cases, hence require consideration of clinical parameters while considering the treatment for the patient.
Andrew Hughes et al.13 in their study stated coefficient of stenosis, which showed significant differences between the symptomatic and asymptomatic patients and also showed significant correlation with Oswestry Disability Index (ODI) and Swiss Spinal Stenosis Questionnaire (SSQ). However, in our study we did not assess the coefficient of stenosis with clinical symptoms.
In our study, we also considered the level of measuring of the MRI measurements at mid vertebral level of lumbar spine except for the ligamentous interfacet distance as the cut off value to consider as stenosis is 12 mm but this cut-off value was not correlating with the southern coastal population, which would result in the false positive results. We measured ligamentous interfacet distance as the inner margins of the ligamentum flavum at the facet joining regions were measured at the lower end plate of the body of the vertebrae of the lumbar spine as suggested by Pawar I et. al.8 and Johann Steurer et.al.15
In our study for determining the association of symptoms with spinal canal stenosis we considered three variables namely antero-posterior, transverse diameters of lumbar spinal canal and cross-sectional area of dural sac whereas Hughes et.al.13 considered all the variables for determining only spinal canal stenosis.
Hughes et.al13 mentioned the importance of cross sectional area of lateral recess as it had the ability to determine the lateral recess stenosis. Cross sectional areas of left and right lateral recess was measured at all the levels but these two variables are not considered in the image analysis for producing results of the study because there were no standard cut-off values for these variables provided in earlier studies. In our study, the average standard mean value for cross sectional area of the lateral recess was 33.6 mm2..
There are few limitations in our study. Firstly, needs to be done in larger sample size for improved results and evaluation of coefficient of stenosis. Secondly, we did not calculate the cut-off value of MRI measurements.
Conclusion
From our study we conclude that the MRI measurements of lumbar spinal canal and foraminal dimensions were found to show weak positive correlation with neurological claudication symptomology assessed based on ECQ.
Acknowledgment
Nil
Conflict of Interest
No conflict of interest
Funding Source
This research did not receive any specific grant from funding agencies
References
- Berthelot JM, Bertrand-Vasseur A, Rodet D, Maugars Y, Prost A. Lumbar spinal stenosis: A review. Rev Rhum Engl Ed., 64(5):315-325(1997).
- Radu AS, Menkès CJ. Update on lumbar spinal stenosis. Retrospective study of 62 patients and review of the literature. Rev Rhum Engl Ed.,65(5):337-345(1998).
- Hilibrand AS, Rand N. Degenerative lumbar stenosis: diagnosis and management. Journal of the American Academy of Orthopaedic Surgeons.,7(4):239-249(1999).
CrossRef - Katz JN, Harris MB. Clinical practice: lumbar spinal stenosis. N Engl J Med.,358(8):818-825 (2008)
CrossRef - Epstein JA, Epstein BS, Jones MD. Symptomatic lumbar scoliosis with degenerative changes in the elderly. spine.,4(6):542-547(1979).
CrossRef - Messiah S, Tharian AR, Candido KD, Knezevic NN. Neurogenic Claudication: a Review of Current Understanding and Treatment Options. Curr Pain Headache Rep.,23(5):32(2019).
CrossRef - Ammendoila C, Stuber KJ, Rok E et al. Nonoperative treatment for lumbar spinal stenosis with neurogenic claudication. Cochrane Database of Systemic Reviews.,8:CD010712(2013).
CrossRef - Pawar I, Kohli S, Dalal V, Kumar V, Narang S, Singhal A. Magnetic resonance imaging in the diagnosis of lumbar canal stenosis in Indian patients. Journal of Orthopaedics and Allied Sciences.,2(1):53(2014).
CrossRef - D Geeta Anasuya, A Jayashree, N.L.N. Moorthy, Seema Madan. Anatomical Study of Lumbar Spinal Canal Diameter on MRI to assess Spinal Canal Stenosis. Int J Anat Res.,3(3):1441-1444(2015).
CrossRef - Ambade RE, Mane KK. Clinical evaluation of lumbar spinal stenosis and its correlation with the MRI findings. Indian Journal of Orthopaedics Surgery., 2(3):293-305(2016).
CrossRef - Janardhana AP, Rajagopal, Rao S, Kamath A. Correlation between clinical features and magnetic resonance imaging findings in lumbar disc prolapse. Indian J Orthop.,44(3):263–269(2010).
CrossRef - Genevay S, Atlas SJ, Katz JN. Variation in eligibility criteria from studies of radiculopathy due to a herniated disc and of neurogenic claudication due to lumbar spinal stenosis: a structured literature review. Spine (Phila Pa 1976).,35(7):803–811(2010).
CrossRef - Hughes A, Makirov SK, Osadchiy V. Measuring spinal canal size in lumbar spinal stenosis: description of method and preliminary results. International journal of spine surgery.,9(3):1-9(2015).
CrossRef - Taylor JR. Growth of human intervertebral discs and vertebral bodies. J Anat.120 (Pt 1):49-68(1975).
- Johann Steurer, Simon Roner, Ralph Gnannt, Juerg Hodler. Quantitative radiologic criteria for the diagnosis of lumbar spinal stenosis: a systematic literature review. BMC Musculoskeletal Disorders.,12:175(2011).
CrossRef







