Rakhi T , Ranjan R K
, Ranjan R K , Sonal Bhat
, Sonal Bhat and Sunil B V
and Sunil B V
Department of Anaesthesiology, Kasturba Medical College, Mangaluru, Manipal academy of higher education Mangluru Karnataka, India
Corresponding Author E-mail: sonalbhat27@gmail.com
DOI : https://dx.doi.org/10.13005/bpj/2179
Abstract
Background: To compare the efficacy of saline, lignocaine 2% and Lignocaine 4% in the endotracheal tube cuff to decrease the incidence of post operative cough and sore throat. A unique, efficient and easy method designed to decrease cough and sore throat during emergence. Hence there was a need for the study. Methods: After approval from institutional Ethical Committee, Kasturba Medical college, Mangaluru and written informed consent from 120 patients of A.S.A class I & II, aged between 18-60 years posted for various surgeries were included. Randomization was done into three groups of 40 patients each. Group 1 – Normal saline, group 2 - 2% Lignocaine and group 3 - 4% Lignocaine. Postoperatively patients were assessed for incidence of cough and sore throat pain based on visual analogue scale (VAS) Results: 65% of patients in group 2 and 72% of patients in group 3 were extubated smoothly, whereas only 20% of patients in group 1 had smooth extubation, p<0.001. There was significant difference in sore throat pain and cough in group 2 and 3 when compared to group 1. Conclusion: The incidence of sore throat and cough was significantly reduced with Lignocaine in the endotracheal tube cuff when compared to saline. Lignocaine 4% was found to be far more better than 2% in reducing sore throat.
Keywords
Alkalinised Lignocaine 2%, 4%; Cough; Emergence; Saline; Sore Throat
Download this article as:| Copy the following to cite this article: Rakhi T, Ranjan R. K, Bhat S, Sunil B. V. Comparison Between the Efficacy of Saline, Alkalinised Lignocaine 2% and Alkalinised Lignocaine 4% in the Cuff of Endotracheal Tube to Reduce the Incidence of Cough and Sorethroat During Extubation. Biomed Pharmacol J 2021;14(2). |
| Copy the following to cite this URL: Rakhi T, Ranjan R. K, Bhat S, Sunil B. V. Comparison Between the Efficacy of Saline, Alkalinised Lignocaine 2% and Alkalinised Lignocaine 4% in the Cuff of Endotracheal Tube to Reduce the Incidence of Cough and Sorethroat During Extubation. Biomed Pharmacol J 2021;14(2). Available from: https://bit.ly/3vfU7Sr |
Introduction
Airway management with cuffed endotracheal tube in General Anaesthesia is an important part of an anaesthesiologist’s responsibilities towards patient. Common complications like cough and sore throat are noted at emergence from general anaesthesia due to inflation of the endotracheal tube cuff. Coughing during emergence results in tachycardia, increased blood pressure, increased intracranial and intraocular pressure, surgical blood loss. This can be of significance in vascular, ophthalmic and neurosurgical procedures. Postoperative sore throat is seen in upto 39-86% of patients1. It is due to various factors like inflammation, haemorrhage, ciliary loss and vocal cord oedema. Topical anaesthetics like lignocaine administered in the endotracheal tube cuff represents an innovative technique to decrease the post-operative cough and sore throat2. Hence there was a need for this study. The airway mucosa coming in direct contact with the ET tube cuff can be anesthetised locally with higher doses of lignocaine (200-500 mg) without compromising supra glottic airway reflex3,4.
Materials and Methods
A prospective, randomised control study was done after obtaining Institutional Scientific and Ethics committee approval. 120 ASA class I or II patients, posted for surgical procedure ( minimum 90 minutes of surgical duration or anaesthesia time of > 120 minutes), aged between 18- 60 years were approved far the study. Patients not willing to participate in the study, asthma , severe pulmonary disease like COPD or emphysema, anticipated difficult intubation, subjects on cough suppressants medication, allergic to lignocaine, pregnancy and H/0 previous airway surgeries were eliminated from the study. All patients were visited day before surgery for pre anaesthetic evaluation (PAC) and written consent was obtained for the study. On the day of surgery before shifting to Operation Theatre (OT), pre-anaesthetic (PAC) orders were reconfirmed. In the OT monitors like electrocardiography (ECG), non-invasive blood pressure (NIBP), pulse oxymetry (SpO2) ), were connected and Baseline parameters like heart rate-HR,blood pressure(SBP,DBP,MAP) were documented and intravenous access secured. Patients were pre oxygenated with 100% oxygen for 3 minutes before inducing the patient. Premedication was done using glycopyrrolate 0.2mg/kg, midazolam 0.03 mg/kg along with fentanyl 2 µg/kg. All the Patients were induced with propofol ,and muscle relaxant atracurium 0.5 mg/kg. Endotracheal intubation was done with proper sized cuffed oral endotracheal tube and the cuff was filled with saline or lignocaine according to respective groups. The Quantity of substance filled in the high volume low pressure cuff were adequate not to cause any leak when ventilated.
120 patients were randomly divided in to three groups . endotracheal tube cuff was filled with either saline or lignocaine or lignocaine with sodium bicarbonate . Group 1: 6.5 ml normal saline, Group 2: 6 ml 2% lignocaine Hydrochloride + 0.5 ml 7.5% sodium bicarbonate, and Group 3: 6 ml 4% lignocaine Hydrochloride + 0.5 ml 7.5% sodium bicarbonate. Anaesthesia was managed with nitrous oxide oxygen mixture with isoflurane. After the surgery, glycopyrrolate 0.02mg/kg and neostigmine 0.05 mg/kg was used to reverse residual blockade. Suctioning was done, cuff deflated and patients were extubated once criterias for extubation is met. The cardiovascular responses at extubation were recorded. Just before extubation, patients were assessed for the incidence of cough. Post-operative sore throat pain were assessed based on visual analogue scale(VAS score)during immediate post op, 2nd hour,4th hour and at 24 hour following extubation.
Statistical Analysis
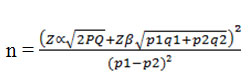
With 95% confidence interval and 80% power with respect to p1 = 3.3 and p2 = 23.3, the sample size was n=120
Zα = 1.96 at 95% Confidence level, Zβ = 0.84 at 80% power, p1 = 3.3; p2 = 23.3, P = p1+ p2/2 = 13.3, q = 100- p
SPSS version 17 was used for analysis. Using ANOVA, Bonferroni’s post hoc test, Chi-square test and Fisher’s exact test, Values were expressed as mean (SD) or median (range). ‘p’ value of ≤ 0.05 was considered as statistically significant.
Results
Factors like age, sex and also the surgery duration were indistinguishable between the groups. 20% of patients in group 1 , 65% of patients in Group 2 and 72% of patients in Group 3 were extubated smoothly, p <0.0001. we experienced laryngospasm in 1 patient in group 1, which was managed appropriately.
Data suggests a significant difference in sore throat pain between group 3, group 2 when compared with group 1. Cough was significantly higher in group 1,when compared to group 2 and 3. Post-operative sore throat pain was found to be greater in the group 1(saline) compared to group 2 (lignocaine 2%) and group 3(lignocaine 4%) during the post-operative 4th hour and increased to reach maximum percentage during the 6th hour and gradually decreased to 5% at the end of 24 hour. There was no much variation between group 2(lignocaine 2%) and group 3(lignocaine 4%) (Graph 1).Visual Analogue Scale(VAS) score was maximum in Group 1 (saline) when compared to Group 2 and 3 in the immediate, 2nd, 4th and 24 hour postoperative period. Kruskal- Wallis test is a non-parametric test, performed to see the differences in the sore throat pain scores in the three groups which showed a significant differences with p value less than 0.001 (Table 1).
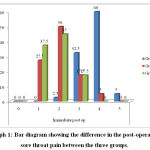 |
Graph 1: Bar diagram showing the difference in the post-operative sore throat pain between the three groups. |
Table 1: Kruskal-Wallis Test and Pairwise comparison by Mann Whitney test comparing post-operative sore throat.
| Pairwise comparison by Mann Whitney test | |||||||
| Kruskal-Wallis Test p value | p value | ||||||
| Immediate post op | Group | Group 1 | 0 | HS | Group 1 VS Group 2 | .000 | HS |
| Group 2 | Group 1 VS Group 3 | .000 | HS | ||||
| Group 3 | Group 2 VS Group 3 | .307 | NS | ||||
| Post op 2 hour | Group | Group 1 | 0 | HS | Group 1 VS Group 2 | .000 | HS |
| Group 2 | Group 1 VS Group 3 | .000 | HS | ||||
| Group 3 | Group 2 VS Group 3 | .110 | NS | ||||
| Post op 4 hour | Group | Group 1 | 0 | HS | Group 1 VS Group 2 | .000 | HS |
| Group 2 | Group 1 VS Group 3 | .000 | HS | ||||
| Group 3 | Group 2 VS Group 3 | .080 | NS | ||||
| Post op 24 hr
|
Group | Group 1 | .000 | HS | Group 1 VS Group 2 | .000 | HS |
| Group 2 | Group 1 VS Group 3 | .000 | HS | ||||
| Group 3 | Group 2 VS Group 3 | .003 | HS | ||||
VS = Very significant HS= Highly significant
Pairwise comparison by Mann-Whitney test shows a highly significant difference between the group 1 versus group 2 and group 3 during the immediate post-operative period, post op 2nd hour, 4th and 24 hour. (Table 1). Heart rate recorded at the time of extubation,5 min,10 min and at the end of 30 min shows a significant difference among the 3 groups. There is considerable decrease in the heart rate in the group 2 (lignocaine 2%) and group 3 (lignocaine 4%) compared to the heart rate in group 1(saline). P value in this ANOVA test is less than 0.001% (Table 2). Results showed that there was a significant decrease in cough in group 2 (lignocaine 2%) and group 3 (lignocaine 4%) compared to group 1 (saline) Number(%) of patients having cough in group 1(saline), 2 (lignocaine 2%) and 3 (lignocaine 4%) was 57.5%,7.5% and 0% respectively (Table 3).
Table 2: One way ANOVA Test, a parametric test was done to compare the differences between the heart rate in the three groups at extubation,5 minute,10 minute and 30 minute post extubation.
| 95% Confidence Interval (Mean) | ||||||||
| N | Mean | Std. Deviation | Lower Bound | Upper Bound | ANOVA test p value | |||
| Extubation | Group 1 | 40 | 100.20 | 5.774 | 98.35 | 102.05 | .000 | HS |
| Group 2 | 40 | 94.75 | 5.513 | 92.99 | 96.51 | |||
| Group 3 | 40 | 95.10 | 4.378 | 93.70 | 96.50 | |||
| 5 min | Group 1 | 40 | 103.80 | 6.236 | 101.81 | 105.79 | .000 | HS |
| Group 2 | 40 | 98.05 | 5.203 | 96.39 | 99.71 | |||
| Group 3 | 40 | 101.95 | 4.579 | 100.49 | 103.41 | |||
| 10 min | Group 1 | 40 | 105.13 | 6.794 | 102.95 | 107.30 | .000 | HS |
| Group 2 | 40 | 96.25 | 5.471 | 94.50 | 98.00 | |||
| Group 3 | 40 | 101.53 | 4.200 | 100.18 | 102.87 | |||
| 30 min | Group 1 | 40 | 101.43 | 7.171 | 99.13 | 103.72 | .000 | HS |
| Group 2 | 40 | 90.63 | 5.182 | 88.97 | 92.28 | |||
| Group 3 | 40 | 91.38 | 5.143 | 89.73 | 93.02 | |||
HS= Highly significant
Table 3: Comparison of group A(saline),group B(lignocaine 2%) and group C(lignocaine 4%)based on the presence of cough in the post operative period.
| Group | Total | ||||||||
| Group 1 | Group 2 | Group 3 | |||||||
| Count | % | Count | % | Count | % | Count | % | ||
| cough | Absent | 17 | 42.5% | 37 | 92.5% | 40 | 100.0% | 94 | 78.3% |
| Present | 23 | 57.5% | 3 | 7.5% | 0 | .0% | 26 | 21.7% | |
| Total | 40 | 100.0% | 40 | 100.0% | 40 | 100.0% | 120 | 100.0% | |
p=0.001, HS = Highly significant
Discussion
The main aim of this study was to compare the best inflating agent between saline, lignocaine 2%, lignocaine 4% that were used to inflate the cuff during anaesthesia. Administration of lignocaine into the endotracheal tube cuff resulted in the diffusion of lignocaine out of the cuff on the tracheal mucosa. During general anaesthesia with nitrous oxide, the pressure inside the cuff increases as the nitrous oxide easily diffuses into the cuff made of polyvinyl chloride than diffusing out of the cuff because of the difference in the pressure across the cuff membrane5. When the endotracheal tube cuff pressure exceeds the capillary perfusion pressure(22mmHg), there is decreased blood supply to the underlying mucosa of the tracheal rings and posterior wall of the trachea resulting in ulceration and postoperative sore throat. By administering liquid medium (saline/ lignocaine), consequences related to hyperinflation can be avoided5,6. Rapidly acting stretch receptors are present throughout the mucosa of tracheal wall. Mechanical stimuli of these receptors are the presumed mechanism for the production of cough. Endotracheal tube intubation, inflation of the cuff and the resulting hyperinflation stimulates the stretch receptors and produces cough during extubation in normal patients. Lignocaine acts on these stretch receptors and blocks the cough reflex. Comparing the present study to an earlier conducted study where intravenous and topical lignocaine were used to decrease the cough during extubation2,4. Lignocaine is a CNS depressant agent and it acts on the cough centre in the medulla and depresses the cough reflex. When given intravenously plasma cancentration of 0.3µg/ml is sufficient to supress cough under general anesthesia and it lasts for a duration of 15-20 minutes. Intravenous lignocaine also results in delayed recovery from anaesthesh5.In another study saline, alkalinised lignocaine and air where compared in decreasing postoperative cough and sore throat where alkalinised lignocaine showed better results which was comparable with our study5,7,8.Alkalinised lignocaine also known to decrease analgesic and sedative requirements in mechanically ventilated patients which was proved in another study 9. One other study concluded that there was no lignocaine overdose,systemic toxicity and endotracheal tube cuff rupture when intracuff lignocaine was used10. Some other studies showed lignocaine when used with dexamethasone produced better results when compared to lignocaine used alone11,12. In the present study we found that there was a statistically significant decrease in the post-operative sore throat and sore throat pain in patients in immediate postoperative period, 2nd hour, 4th hour and 24 hour belonging to group 2 (6ml 2% lignocaine Hydrochloride + 0.5 ml 7.5% sodium bicarbonate) and group 3 (6ml 4% lignocaine Hydrochloride + 0.5ml 7.5% sodium bicarbonate) compared to group 1 (normal saline). The results obtained were similar to the earlier conducted study. The incidence of cough is significantly reduced in the group 2 (6 ml 2% lignocaine Hydrochloride + 0.5 ml 7.5% sodium bicarbonate) and group 3(6ml 4% lignocaine Hydrochloride + 0.5ml 7.5% sodium bicarbonate) compared to group 1(saline). Studies previously have compared intravenous,intracuff lignocaine and saline, but alkalinized 2% and 4% lignocaine had never been studied. Hence there was scope for this study. Filling buffered lignocaine into the endotracheal tube resulted in diffusion of uncharged lignocaine across the cuff 1,13,14. Lignocaine being a weak basic, lipophilic drug binds ardently to the respiratory mucosa to produce the effect.
Conclusion
The incidence of post-operative sorethroat is significantly reduced when lignocaine is administered into the endotracheal tube cuff compared to the saline. On comparing lignocaine 2% and lignocaine 4%, lignocaine 4% was found to be better in reducing the postoperative sorethroat. Administration of lignocaine into the cuff also resulted in significant reduction of cough.
Acknowledgment
We would like to thank Kasturba Medical College, Mangaluru and Manipal University, Manipal, Karnataka, India for their support in conducting this study.
Funding Source
There is no Funding Source
Conflicts of interest
There is no Conflicts of interest
References
- Dollo G, Estebe JP, Le Corre P, et al. Endotracheal tube cuffs filled with lidocaine as a drug delivery system: in vitro and in vivo European Journal of anaesthesia 2001;13:319-23.
CrossRef - Estebe JP, Delahaye S, Le Corre P, et al. Alkalinisation of intra-cuff lidocaine and use of gel lubrication protect against tracheal-tube induced emergence phenomena. British Journal of Anaesthesia 2004:92(3):361-66.
CrossRef - Fagan, Carl, Frizelle, Henry P,Laffey, John; Hannon, Vincent, Carey, Michael;Effects of Alkalinized lignocaine in Endotracheal tube cuff in prevention of cough and sore throat during emergence. Anesthesia & Analgesia 2000;91(1): 201-5.
CrossRef - Yukioka H, Yoshimoto N, Nishimura K, Fujimori M. Intravenous lidocaine as a suppressant of coughing during tracheal intubation Anesthesia Analgesia;1985;64:1189-92.
CrossRef - Jaichandran V V, Angayarkanni N, Coral K, Bhanulakshmi I, Jagadeesh V. Diffusion of lidocaine buffered to an optimal pH across the endotracheal tube cuff An in-vitro study. Indian Journal of Anaesthesia 2008;52(5):536-40.
- Miller’s anaesthesia, Local Anesthetics; Elsevier Saunder; 8th Edition; 2015;1028-54.
- Indu S, Arun M.G, Taznim Mohamed, Suvarna K et al. Effect of intracuff media alkalinised lignocaine, saline and air on endotracheal tube induced emergence phenomenon: A randomised control study. Journal of evidence based medicine and health care.2016; 3:3173-77.
CrossRef - Gaurav Acharya, Rashpal Singh Gill, Prem Chandra Arya, Kishore Kumar Comparison of intracuff lignocaine and air and its related complications. European Journal of pharmaceutical and research; 2016:382-387.
- Ahmed Sobhy Basuni. Intracuff alkalized lidocaine reduces sedative/analgesic requirements for mechanically ventilated patients. Saudi Journal of Anaesthesia;2014: 415-455.
- Fai Lam, Yu-Cih Lin, Hsiao-Chien Tsai,Ta-Liang Chen, Ka-Wai Tam, Chien-Yu Chen et al. Systematic Review and Meta Analysis of Randomised Controlled Trials on Effect of Intracuff Lignocaine on Postoperative Sore Throat and The Emergence Phenomenon 2015 Public library of science 2015; 1371:1-17.
- Raghavan Suresh Babu, Peter Kadamala. MadhuVelayudhan.The effect of intracuff lignocaine versus lignocaine with dexamethasone on endotracheal tube induced emergence phenomenon after general anaesthesia- A comparative study. The Journal of evidence based medicine and healthcare; 5:392-96.
CrossRef - Choon-Kyu Cho, Ji-Eun Kim, Hun-Ju Yang, Tae-Yun Sung, Hee-Uk Kwon, and Po-Soon Kang. The effect of combining lidocaine with dexamethasone for attenuating postoperative sore throat, cough, and hoarseness. Anaesthesia Pain Medicine 2016; 11: 42-8.
CrossRef