Mostafa Hassan Ragab1, Eman Monir Sherif 2, Nadia Badawy Abd- El Gawad3, Safaa Mohamed Elserougy3, Eman Essam Shaban4 and Elham Mohamed Mostafa4
1Environmental and Occupational medicine, department of medical science, Institute of Environmental Studies and Research, Ain Shams University, Cairo, Egypt
2Department of Pediatrics, Pediatric and adolescence diabetes unit, Ain Shams University Egypt
3Environmental and Occupational medicine, National Research Centre, Cairo, Egypt
4Department of Environmental and Occupational medicine, National Research Centre Egypt
Corresponding Author E-mail: elhammostafa@hotmail.com
DOI : https://dx.doi.org/10.13005/bpj/2126
Abstract
Diabetes is one of the commonest chronic diseases worldwide. Vitamin D deficiency showed to be increasing, and have a potential role in autoimmune diseases among which in type 1 diabetes. The aim The aim of the study was to assess the impact of oral vitamin D supplementation on blood glucose (HbA1C) in T1DM patients and to find out the role of vitamin D as a biomarker for follow of T1DM patients compared to HbA1C. Subjects and methods: A randomized interventional clinical study was designed. The study enrolled 60 children patients with T1DM. Only 45 children continued to the end of study. Initial (pre-intake) assessment included history taking, clinical examination, and measurement of serum 25-OH vitamin D3 and serum HbA1C. These children received oral vitamin D supplements for 3 months then post-intake assessment were done again. Results: The study showed that serum vitamin D was deficient among Egyptian children and adolescents with T1DM (mean 11.4±3.4 ng/ml). , 53.33% of the patients had vitamin D deficiency with a 35.6% had insufficiency and 11.11% were VD sufficient. Patients received oral vitamin D supplementation for 3 months after which marked improvement in the levels of serum vitamin D levels and HA1C, 87.5% and 86.5% respectively.
Keywords
Diabetes - Type1 diabetes mellitus (T1DM) -Vitamin D -Ultra-Violet Index
Download this article as:| Copy the following to cite this article: Ragab M. H, Sherif E. M, Gawad N. B. A, Elserougy S. M, Shaban E. E, Mostafa E, M. Influence of Supplementary Vitamin D on the Prognostic Pathway of Type1 Diabetes Among Children.Biomed Pharmacol J 2021;14(1). |
| Copy the following to cite this URL: Ragab M. H, Sherif E. M, Gawad N. B. A, Elserougy S. M, Shaban E. E, Mostafa E, M. Influence of Supplementary Vitamin D on the Prognostic Pathway of Type1 Diabetes Among Children.Biomed Pharmacol J 2021;14(1). Available from: https://bit.ly/2N9Weq9 |
Introduction
Diabetes mellitus ‘DM’ is a multifactorial metabolic disorder characterized by chronic hyperglycemia with disturbances of carbohydrate, fat, and protein metabolism arising from defects in insulin secretion, insulin action, or both. The impact of DM comprises chronic damage, dysfunction, and failure of various organs (1).
Type 1 Diabetes Mellitus (T1DM) is a common endocrine and metabolic condition in childhood and adolescence. The patients require lifelong insulin injections for survival. The overall increase in the incidence of T1DM is around 3% and about 78,000 children under age 15 years develop T1DM worldwide (2). The wide variation in incidence can hardly be explained by genetic factors alone. Environmental factors have long been implicated in the pathogenesis of T1DM both as initiator and potentiator of pancreatic β-cells damage (3).
When using glycosylated hemoglobin (HbA1C) to diagnose DM, it is important to recognize that HbA1C is an indirect measure of average blood glucose levels and to take other factors into consideration that may impact hemoglobin glycation independently of glycemia including age, race and anemia/ hemoglobinopathies (4).
Vitamin D (vit D) is a multi-functional fat-solute metabolite required for human growth and health. The primary source of vitD in (80–90%) is from endogenous biosynthesis in skin cells, a critical step of which is hydroxylation of 7-dehydrocholesterol into cholecalciferol catalyzed by the ultraviolet radiation from sunlight (5). During sun exposure, the ultraviolet B photons are absorbed by the cutaneous 7-dehydrocholesterol to form the split sterol pre-vit D3. However, a variety of factors limit the cutaneous production of vit D3. An increase in skin melanin pigmentation or the topical application of a sunscreen will absorb solar ultraviolet B photons and thereby significantly reduce the production of vit D3 in the skin. Latitude, time of day, and season of the year have a dramatic influence on the cutaneous production of vit D3. Lifestyle factors may also be associated with lower vit D concentrations, such as reduced physical activity, and increased body mass index (BMI) due to deposition of vit D in adipose tissue, where it becomes biologically inactive (6).
The role of vit D in innate immunity is postulated as deficiency can lead to autoimmune conditions, such as type 1 diabetes. Vitamin D and its metabolites as well as constituents of inflammation seem to have important effects on insulin synthesis, secretion and action (7). At the level of the immune system, 1, 25(OH)2 D3 inhibits the differentiation and maturation of dendritic cells and promotes their apoptosis (8). At the level of the pancreatic islets, 1,25(OH)2D3 decrease proinflammatory chemokine and cytokine expression, which are implicated in the pathogenesis of T1DM making β-cells less chemoattractive and less prone to inflammation (9).
Aim
The aim of the study was to assess the impact of oral vitamin D supplementation on blood glucose (HbA1C) in T1DM patients and to find out the role of vitamin D as a biomarker for follow of T1DM patients compared to HbA1C.
Subjects and methods
Environmental recordings
Ultraviolet rays have a known impact on vit D metabolism. Therefore, ultraviolet index (UVI) was recorded throughout the period of the study (September 2019 till end of March 2020) – through daytime hours using website: https://www.accuweather.com/ar/eg/cairo/127164/weather-forecast/127164
Study design
A randomized interventional clinical study was designed using oral vitD supplements for 3 months.
Subjects
The study included 60 children and adolescents with type 1 diabetes (30 males and 30 females) with a final compliance of 45 patients, and an attrition of 15 patients (25% drop out percentage). The patients were attending the Pediatric and Adolescents Diabetes Clinic of Children’s Hospital, Ain Shams University, Egypt, over 7 months period from September 2019 to March 2020. The study protocol was approved by the Medical Research Ethics Committee of National Research Center and patients were included after obtaining informed consents from their legal guardians after explaining the aim and steps of the study.
Criteria of inclusion
Participants are children aged between 6-14 years old of both sexes.
Diabetics with established diagnosis of T1D, according to the International Society For Pediatric and Adolescent Diabetes criteria (ISPAD Consensus Guidelines, 2018)
The patients are otherwise free from any other health problems.
Criteria for exclusion
Symptoms and signs of infection within 1 month of the study.
Receiving vit D or calcium supplements via any route, one year previous to the study.
Methods
All participants were subjected to 1- pre-intake assessment: included detailed history taking, full clinical examination (including weight and height measuring and BMI Percentiles calculation), and laboratory assessments: included serum 25-OH vitamin D3 (using 25-OH vitamin D3 ELISA kit provided by ORGENTEC Diagnostika GmbH, Mainz Germany), and Hb A1C (Using Fine Care FIA meter apparatus for flurorescence immunoassay quantitative tests by Guangzhou Wondfo Biotech Co., China), 2- The patients were given vit D3 supplements in the form of oral drops (vidrops), 1ml per day orally that is equivalent to 2800 IU of cholecalciferol (for 3 months), 3-Follow-up assessment including (history follow up of symptoms and signs, clinical examination, serum vit D assessment and HbA1C measurement) were done after 3 months from the pre-intake assessment. Percentages of vit D categories in T1DM patients in the present study (vit D deficiency, < 12 ng/ml; insufficiency, 12 – 20 ng/ml; sufficiency, > 20 – 150 ng/ml) (10)
Statistical Analysis
SPSS (version 26) statistical package was used for analysis of data. Data was summarized as mean, standard deviation (±SD), count and percent. Shapiro-Wilk test was used for normality testing. Time series chart (sequence plot) of daily UVI recordings throughout study period was drawn. Paired t-test was used for compare means of measured parameters before and after vitamin D supplementation. Independent t-test test was used for comparisons between means of parameters between two different groups. Pearson’s correlation () was done to detect the relation between the parameters. P-value is considered to be significant if p <0.05.
Results
The time series chart (figure 1) showed the variations in UVI on a daily/montly basis throughout 7 months (the period of the study from September 2019 till end of march 2020). The UVI was least on December (mean was 2.9±0.5), that increases gradually towards September and March (means were 6.9±0.3 and 5.9±2.1 respectively). Mean UVI was least at 8 am and 4 pm (1.3) and reaches a peak value at 12 pm with mean of 4.29.
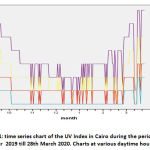 |
Figure 1: time series chart of the UV Index in Cairo during the period from 20th September 2019 till 28th March 2020. Charts at various daytime hours were shown. |
The patients who completed the study were 25 females (55.6%) and 20 males (44.4%). Those below 12 years constituted 67% (30 cases out of 45 enrolled cases).
It was found that 24 patients (53.3%) had vit D deficiency with a mean of 8.8±1.6 ng/ml, 16 patients (35.6%) had insufficiency with a mean of 14.4±2.4 ng/ml and only 5 (11.11%) had vit D sufficient serum levels with a mean of 24.6±1.5 ng/ml.
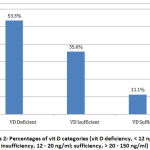 |
Figure 2: Percentages of vit D categories (vit D deficiency, < 12 ng/ml; insufficiency, 12 – 20 ng/ml; sufficiency, > 20 – 150 ng/ml) |
The sex and age groups did not seem to have an effect on pre- and post- intake serum vit D levels and pre- and post- intake HbA1C levels. There were no significant differences between males and females (table 1) and between younger (<12 years) and older (≥12 years) age groups (p>0.05) (table 2).
Table 1: Comparison between males and females as regards serum vit D and HbA1C at pre- and post-intake.
| Test | Sex | Mean | ± SD | P-value |
| Serum vitamin D initial (ng/ml) | Males | 11 | 2.9 | 0.59 |
| Females | 11.6 | 3.8 | ||
| Serum vitamin D post-intake (ng/ml) | Males | 29.3 | 8.4 | 0.72 |
| Females | 30.2 | 8.8 | ||
| HbA1Cinitial (%) | Males | 9 | 1.9 | 0.37 |
| Females | 9.5 | 1.8 | ||
| HbA1C post-intake (%) | Males | 6.8 | 1.7 | 0.26 |
| Females | 7.3 | 1.4 |
SD means standard deviation
Table 2: Comparison between cases <12 years old and cases ≥ 12 years old as regard levels of serum vit D and of HbA1C
| Test | Age | Mean | ± SD | P-value |
| Serum vitamin D initial (ng/ml) | < 12yrs | 11.3 | 3.1 | 0.97 |
| ≥ 12yrs | 11.4 | 4.1 | ||
| Serum vitamin D post-intake (ng/ml) | < 12yrs | 29.9 | 7.7 | 0.91 |
| ≥ 12yrs | 29.6 | 10.3 | ||
| HbA1Cinitial (%) | < 12yrs | 9.1 | 1.8 | 0.39 |
| ≥ 12yrs | 9.6 | 1.9 | ||
| HbA1C post-intake (%) | < 12yrs | 6.9 | 1.6 | 0.56 |
| ≥ 12yrs | 7.3 | 1.6 |
SD means standard deviation
There was a highly significant improvement in the levels of serum vit D and HbA1C after the administration of vit D using paired t-test. Vit D increased from 11.4±3.4 to 29.9±8.5 ng/ml (p-value = 0.00001) and HbA1C dropped from 9.3±1.8 to 7.1±1.6 % (p-value = 0.00001) table (3). Results of correlation between serum vit D and HbA1C confirmed results of paired t-tests as there was a highly significant negative correlation between HbA1C and serum vit D ( r = -0.54, p = 0.00001).
Table 3: Comparison between mean levels of pre- and post-intake serum vit D as regards serum vit D and HbA1C (oral vit D intake for three months).
| Test | Mean | ± SD | Paired T-Test | P_value |
| Serum vitamin D (ng/ml) (initial) | 11.4 | 3.4 | 17.6 | 0.00001 |
| Serum vitamin D (ng/ml) (post-intake) | 29.8 | 8.5 | ||
| HbA1C initial (%) | 9.3 | 1.8 | 16.8 | 0.00001 |
| HbA1C post-intake (%) | 7.1 | 1.6 |
Discussion
The current study showed significant decline in serum vit D level among a group of Egyptian children and adolescents despite the sunny weather and moderate to high range of UVI, 24 patients (53.33%) had vit D deficiency with 16 patients (35.6%) had insufficiency and only 5 (11.11%) were vit D sufficient. This goes in hands with what Hafez et al (10) found that among 50 Egyptian children with T1D 70% of the patients had vit D deficiency, 24% had insufficiency and 6% were vit D sufficient. Also Hassan et al who conducted a study on 60 Egyptian children and adolescents with T1DM and found that 91.67% of were vit D deficient (11). Similarly, another Egyptian studies revealed a prevalence of 84.9% (12) and 75% (13). This concurs with Bin Abbas et al., (14) and Bener et al., (15) found that vit D deficiency was considerably higher in children with T1DM (84%, 90.67% respectively). Janner et al, (16) reported relatively lower prevalence (28%). This high prevalence of VDD in Egypt despite the presence of adequate sunlight and sunny weather most of the year can be attributed to the vit D receptor gene polymorphism (17) as well as the lack exposure to sunlight due to religious or cultural reasons. Or due to conducting the study during autumn and winter with the lowest UVI levels. Another possible cause as reported by Xiang et al., (18), that pigmented skins are less effective than light skins at vit D production.
Our study showed highly significant negative correlation between levels of serum vit D and HbA1c (r = -0.54, p = 0.00001). Similarly, Al-Agha and Ahmad (19) identified a significant relationship between HbA1c and the status of vit D among diabetic patients. Soliman and his colleagues (12) also found a significant strong negative correlation between 25OHD levels and HbA1c%. This was in concur with what Aljabri et al. (20) reported. On the other hand, Janner et al. (16) found no such significant correlation in the Swiss population. This could be explained on ethnic or genetic bases since most of the concurring studies were conducted in Egypt.
The current study shows improvement in the levels of serum vit D levels and HbA1C after the administration of vit D, 87.5% and 86.5% respectively and statistical analysis shows that, the improvement was statistically highlysignificant (p-vales < 0.05). in concur with that, Hafez et al (10) reported that VIT D supplementation was associated with a significant improvement in HbA1c% mean values. Similarly, Parildar and his co-workers (21) found a significant reduction in HbA1c following vit D supplementation in patients with prediabetes favoring the improvement in glucose metabolism. Aljabri et al. (21) concluded that vitD supplementation might improve the glycemic control of patients with T1D as there was significant reduction in HbA1c% levels following a supplementation given to 80 patients with T1D aged over 12 years. Walter and his colleagues (22) as well as a meta-analysis conducted by George et al. (23) in Scotland, observed no significant improvement in HbA1c% or fasting blood glucose in those receiving vit D supplementation compared with those who received placebo concluding that there was insufficient evidence of the beneficial effect of vit D supplementation as a means of improving glycemic control in children and adolescents with T1D.
Our study showed no significant statistical difference between comparable groups (either sex difference or age difference) regarding the levels of serum vit D and HbA1c% initially or post vit D intake. That was also reported by Branco et al. (24) and Mutlu et al. (25) who found no significant difference between males and females regarding 25OHD and their glycemic control. In contrast, Hafez et al (10) found no significant sex difference regarding HbA1c% but males had higher mean 25OHD levels. That was also the case in the study conducted by Al-Agha and Ahmad (19) where the boys had higher levels of vit D. This could be attributed to females covering their head and body due to cultural and religious reasons. In addition to the fact that, more vit D is required for bone growth during faster pubertal spurt in females (26).
Conclusion
The study showed that serum vit D was deficient among Egyptian children and adolescents with T1D (mean 11.4±3.4 ng/ml). , 53.33% of the patients had vit D deficiency with a 35.6% had insufficiency and 11.11% were vit D sufficient. Patients received oral vit D supplementation for 3 months after which marked improvement in the levels of serum vit D levels and HA1C, 87.5% and 86.5% respectively.
Acknowledgment
We would like to thank the National Research Centre in Cairo, Egypt for supporting and facilitating this work. We would like to express our appreciation to our colleagues and nurses at The Pediatric and Adolescents Diabetes Clinic, of Children’s Hospital, Ain Shams University, Egypt who facilitated this work. Last but not least, I’d like to thank all children and their parents who participated in the study
Conflict of interest
No conflict of interest
Funding Source
National Research Centre, Cairo, Egypt
References
- American Diabetes Association (ADA). 2. Classification and Diagnosis of Diabetes. Diabetes Care 2017;40 (Suppl. 1):S11–S24
CrossRef - International Diabetes Federation. The IDF Diabetes Atlas. 5th ed., Brussels: International Diabetes Federation; 2011. http://www.idf.org/idf-diabetes-atlas-fifth-edition. Date of last access 23th April 2013.
- Knip M and Simell O. Environmental Triggers of Type 1 Diabetes. Cold Spring HarbPerspect Med 2012;2:a007690
CrossRef - Nowicka P, Santoro N, Liu H, et al. Utility of hemoglobin A1c for diagnosing prediabetes and diabetes in obese children and adolescents. Diabetes Care 2011;34:1306–1311
CrossRef - Holick MF. Sunlight and vitamin D for bone health and prevention of autoimmune diseases, cancers, and cardiovascular disease. Am J ClinNutr 2004;80:1678Se88S.
CrossRef - Wortsman J, Matsuoka LY, Chen TC, et al. Decreased bioavailability of vitamin D in obesity. Am J ClinNutr 2000;72:690e3.
CrossRef - M, Dhananjayan.R and Swaminathan.S. The Significance and Importance of Vitamin D and Zinc in Type2 Diabetes Mellitus: International Journal of Research Studies in Biosciences (IJRSB) Volume 3, Issue 8, August 2015, PP 78-85
CrossRef - Emamaullee JA, Davis J, Merani S, Toso C, Elliott JF, Thiesen A and Shapiro AM: Inhibition of Th17 cells regulates autoimmune diabetes in NOD mice. Diabetes 2009, 58(6):1302–11.
CrossRef - Giarratana N, Penna G, Amuchastegui S, Mariani R, Daniel KC andAdorini L: A vitamin D analog down-regulates proinflammatory chemokine production by pancreatic islets inhibiting T cell recruitment and type 1 diabetes development. J Immunol 2004, 173(4):2280–2287.
CrossRef - Hafez M., Hassan M., Musa N., Abdel Atty S. and Abdel Azim S. Vitamin D status in Egyptian children with type 1 diabetes and the role of vitamin D replacement in glycemic control. J PediatrEndocrinolMetab 2017; 30(4): 389–394
- Hassan MM, Alashmawy AA, Sharaf SA, Soliman HM, Fares ZMA, andImad M A. Vitamin D Status in Egyptian Children and Adolescents with Type 1 Diabetes Mellitus. J Diabetes Metab 6: 636.
- Soliman GT, Ali BA, Mohamed AA, Mahmoud AM andAbdellatif AA. Assessment of vitamin D status in Egyptian children with type-1 diabetes mellitus. J Diabetes Metab 2015;6:573.
CrossRef - Abd-Allah SH, Pasha HF, Hagrass HA andAlghobashy AA. Vitamin D status and vitamin D receptor gene polymorphisms and susceptibility to type 1 diabetes in Egyptian children. Gene 2014;536:430–4.
CrossRef - Bin-Abbas BS, Jabari MA, Issa SD, Al-Fares AH and Al-Muhsen S.Vitamin D levels in Saudi children with type 1 diabetes. Saudi Med J 32: 589-592. 11.
- Bener A, Alsaied, Al-Ali M , Kubaisi A, Basha B, et al. High prevalence of vitamin D deficiency in type 1 diabetes mellitus and healthy children. ActaDiabetol 46: 183–189.
CrossRef - Janner M, Ballinari P, Mullis EP and Fluck CE. High prevalence of vitamin D deficiency in children and adolescents with type 1 diabetes. Swiss Med Wkly 140: 13091.
- Hamed EO, Abdel-Aal AM, Din AK andAtia MM. Vitamin D level and Fok-I vitamin D receptor gene polymorphism in Egyptian patients with type-1 diabetes. Egypt J Immunol 2013;20:1–10
- Xiang, F. , Lucas, R. , de Gruijl, F. , and Norval, M. A systematic review of the influence of skin pigmentation on changes in the concentrations of vitamin D and 25‐hydroxyvitamin D in plasma/serum following experimental UV irradiation. Photobiol. Sci. 14, 2138–2146.
CrossRef - Al-Agha AE andAhmad IA. Association among vitamin D deficiency, type 1 diabetes mellitus and glycemic control. J Diabetes Metab 2015;6:594
CrossRef - Aljabri KS, Bokhari SA and Khan MJ. Glycaemic changes after vitamin D supplementation in patients with type 1 diabetes mellitus and vitamin D deficiency. Ann Saudi Med 2010;30:454–58.
CrossRef - Parildar H, Cigerli O, Unal DA, Gulmez O,Demirag NG. The impact of vitamin D replacement on glucose metabolism. Pak J Med Sci 2013;29:1311–4
CrossRef - Walter M, Kaupper T, Adler K, Foersch J, Bonifacio E, et al. No effect of the 1,25-dihydroxyvitamin D3 on b-cell residual function and insulin requirement in adults with new-onset type 1 diabetes. Diabetes Care 2010;33:1443–8.
CrossRef - George PS, Pearson ER and Witham MD. Effect of vitamin D supplementation on glycaemic control and insulin resistance: a systematic review and meta-analysis. Diabet Med 2012;29:e142–50.
CrossRef - Branco S, Rego H, Costa C, Correia C andFontoura M. Vitamin D deficiency in children and adolescents with type 1 diabetes. Pediatr Diabetes 2012;13:91–2.
CrossRef - Mutlu A, Mutlu GY, Ozsu E, Cizmecioglu FM andHatun S. Vitamin D deficiency in children and adolescents with type 1 diabetes. J Clin Res PediatrEndocrinol 2011;3:179–83
CrossRef - Razzaghy-Azar M andShakiba M. Assessment of vitamin D status in healthy children and adolescents living in Tehran and its relation to iPTH, gender, weight and height. Ann Hum Biol 2010;37:692–701
CrossRef








