Zakaria Tahiri1* , Mounir Mkimel2
, Mounir Mkimel2 , Laila Jroundi3 and Fatima Zahra Laamrani3
, Laila Jroundi3 and Fatima Zahra Laamrani3
1Doctoral Study Center for Life and Health Sciences, Faculty of Medicine and Pharmacy of Rabat, Impasse Souissi, Rabat 10100, Morocco.
2Laboratory of Technology and Health Sciences, High Institute of Health Sciences, Route de Casablanca km 3,5 université hassan 1er. BP 555, Settat, Morocco.
3Emergency Radiology Department, Faculty of Medicine and Pharmacy of Rabat, Impasse Souissi, Rabat 10100, Morocco.
Corresponding Author E-mail: tahiri.zakaria@gmail.com
DOI : https://dx.doi.org/10.13005/bpj/2120
Abstract
Digital Mammography is used as a screening tool to discover breast cancer at an early stage, the benefits and harms of this techniques is under scrutiny hence and Moroccan regulations governing radiation protection of patients have been strengthened, the need to investigate the dose received during screening mammography and the risk associated. This study is consisted of examining 126 mammography projections, for 63 women. All examinations were performed with a full digital mammography machine, technical and exposure parameters were recorded, statistical analysis was carried out using Microsoft Excel in order to calculate local DRLs and compare them with international standards. Cancer risk has been estimated using BEIR VII report methods. The mean glandular dose MGD was 1,09±0, 45 mGy and 1,26±0,74 mGy for craniocaudal (CC) and mediolateral oblique (MLO) respectively, DRLs were 1,34 for CC view and 1,36 for MLO view. Of the 100,000 women exposed, Lifetime Attributable Risk of cancer incidence has been found to be 0,76 for CC examination, 0.88 for MLO, and 1,64 for the full mammography protocol. Established local DRLs in this study are lower compared to that of United Kingdom and France and higher compared to that of Nigeria and Australia. A potential risk of radiation-induced carcinogenesis exists, and there is a need for optimization of screening mammography practices.
Keywords
Breast Cancer; Mammography; Radiation Biological Effects; Radiation Protection
Download this article as:| Copy the following to cite this article: Tahiri Z, Mkime M, Jroundi L, Laamrani F. Z. Evaluation of Radiation Doses and Estimation of the Risk of Radiation-Induced carcinogenesis in Women Undergoing Screening Mammography Examinations. Biomed Pharmacol J 2021;14(1). |
| Copy the following to cite this URL: Tahiri Z, Mkime M, Jroundi L, Laamrani F. Z. Evaluation of Radiation Doses and Estimation of the Risk of Radiation-Induced carcinogenesis in Women Undergoing Screening Mammography Examinations. Biomed Pharmacol J 2021;14(1). Available from: https://bit.ly/3tapXyZ |
Introduction
X-ray mammography offers the possibility of discovering breast cancer at an early stage, organized screening program recommends one mammography examination every 2 years for women aged 50 to 74 with no specific symptoms [1]. For a woman considered to be at risk, this can lead her to undergo several mammography examinations, without counting the other examinations she will undergo during her life (CT Scans, X ray procedures). In addition, during a mammogram, a woman can have several images and receive repeated doses. This received doses from mammography examinations may be associated with a risk of radiation-induced carcinogenesis [2], annual screenings of 100,000 women aged 40 to 74 years have been projected to induce an average 125 breast cancer resulting in 16 deaths [3].
A new law no.142-12 [4] has been adopted, governing nuclear and radiological safety and security, which contains new provisions relating to radiation protection of patients, by applying the principle of justification and optimization of the doses delivered. Diagnostic reference levels (DRLs) play an important role in health-care delivery and radiation safety of patients, they are suggested radiation dose levels of the radiographic investigations above which a medical facility could review its work methods and determine if required image quality can be achieved at lower doses.
This study was to evaluate radiation doses delivered during screening mammography procedures in order to compare them with international standards, guided by Dose Reference levels (DRLs) and estimate the Lifetime Attributable Risk of Cancer Incidence due to radiological exposure.
Materials and Methods
Machine Specification
GE Senographe 2000D with a range of 22 to 49 for kV and 4 to 500 for mAs , a rotating anode with two different targets (Molybdenum and Rhodium), and an inherent filtration of 0.03 mm Molybdenum , 0.025 mm Rhodium and 1.0 mm Aluminum.
Exposure Parameters Survey
In this study, all examinations were performed with a full field digital mammography which are subject of a recent approved quality control, DICOM headers were extracted from Picture Archiving and Communications System (PACS), technical and exposure parameters from 126 projections for 63 adult patients (patients aged 45 to 55) were recorded, kV, mAs, Mean glandular dose (MGD), Entrance Surface Dose (ESD) and used filters, and statistical analysis was realized using Microsoft Excel 2016. The study was limited to screening examinations, therefore, the rest of procedures were excluded.
Diagnostic Reference Level
In digital mammography, the diametric scale used to establish DRLs is the average dose to the mammary gland (MGD), expressed in milligrays (mGy), and determined for an equivalent breast thickness of 45 mm, the value of the DRLs is defined from the 75th percentile of the distributions of data collected for a standard examination [5] , the 75th percentile constitutes a level of alert above which the practices can be considered as not optimized in term of delivered dose to the patient, considering its international use, it remains an essential indicator of DRLs.
In this study, the projections were analyzed, the median and 75th percentiles were calculated across MGDs obtained and compared to DRLs from United Kingdom[6], Australia[7], Nigeria [8], and France [9].
Cancer Risk Estimation
The estimation of cancer risks following exposure to ionizing radiation has been the subject of several reports by international organizations such as the International Commission on Radiological Protection (ICRP) and the United Nations Scientific Committee on the Effects of Atomic Radiation (UNSCEAR) during the past few decades. These estimates have been based largely on data for survivors of the atomic bombings of Hiroshima and Nagasaki, supplemented in some instances by information from studies of medically exposed groups [10].
In this study, Lifetime Attributable Risk of cancer incidence and has been estimated using BEIR VII report methods [11], the most up-to-date and comprehensive risk estimates for cancer and other health effects from exposure to low-level ionizing radiation, based on epidemiological data from radiation-exposed populations and aims to estimate cancer risk induced by exposure to low-linear energy transfer radiation.
Results
Statistical Analysis
A total of 126 projections (Mediolateral Oblique View “MLO” and Craniocaudal “CC”) for 63 patients were performed during the data collection period in the medical imaging department. The mean age of patients is 50 years. The average values for weight and height were 68 kg and 1.65 m respectively.
Tables 1 and 2 present a summary of the exposure parameters details used for the screening mammography of examinations of all the women involved in the study.
In most cases, the mean glandular dose in MLO projections was higher than recorded in the CC projection due to higher mAs used in the MLO projection.
Table 1: Comparison of the MGD received in MLO and CC projections
|
Projection |
CC mGy
(mean±SD) |
MLO mGy (mean±SD) | Δ (%) |
|
MGD |
1,09±0,45 | 1,26±0,74 | 13,61 |
Table 2: The range of exposure details (mAs, kv and ESE ) obtained during screening mammography for 63 projections.
| Projection | mAs (mean±SD) | kVp (mean±SD) | ESE mGy (mean±SD) |
| Cranio-caudal | 45,93±24,24 | 30,53± 1,33 | 5,68±3,32 |
| Medio-lateral oblique | 53,43±36,48 | 30,96±1,35 | 6,96±5,4 |
The mean effective tube time current, tube voltage and Entrance Surface Dose ESE for CC and MLO projections was (45,93±24,24 , 53,43±36,48) , (30,53± 1,33 , 30,96±1,35) and (5,68±3,32 , 6,96±5,4) respectively .
The analysis of the exposure factors showed that both kV and mAs were higher for MLO views than for CC views. The MGD for this study was 1,09±0,45mGy and 1,26±0,74 mGy for craniocaudal (CC) and mediolateral oblique (MLO) respectively.
MGD values compared to DRLs
The diagnostic reference level (DRLs) is generally defined as the 75th percentile of the distributions of mean glandular doses observed as shown in (fig. 1) [12] .In this study, the 75th percentile is estimated for all patients based on the average glandular dose from two projections ( MLO, CC ), Table 3 present 75th percentile, median values of MGD compared with DRLs from different countries.
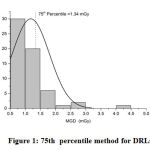 |
Figure 1: 75th percentile method for DRLs. |
Table 3: Comparison of calculated DRLs for mammography examination with DRLs from different countries.
|
Projection |
MGD mGy |
DRLs |
DRLs |
DRLsFrom NGRc |
DRLs |
DRLs |
|
| Median | 75th Percentile | ||||||
| CC | 0,98 | 1,32 | 0,88 | 2,5 | 0,63 | 1,6 |
1,32 |
|
MLO |
1 |
1,34 |
1,30 | 2,5 | 1,04 | 1,6 | 1,34 |
a Aus: Australia[7], b UK: United kingdom [6], c NGR: Nigeria [8], d FR: France [9].
DRLs for France, United kingdom, Nigeria, Australia and this work were 1.6 mGy, 2.5 mGy, 0.63 mGy, 0.88 and 1.32 mGy for CC view, DRLs for MLO was 1.6 mGy, 2.5 mGy, 1.04 mGy, 1.30mGy and 1.13 for Fr, Uk, Ngr, Aus, and present work, respectively.
Cancer Risk
The radiation risk estimates for developing radiation induced carcinogenesis was performed using the data evaluated by the Biological effects of ionizing radiation committee seven (BEIR VII) relative risk model for breast cancer incidence. The BEIR report is addressing health effects from exposure to low-energy radiation, including mammography based on the number of cases per 100,000 persons exposed to a single dose of 0.1 Gy.
Of the 100,000 persons exposed, the Lifetime Attributable Risk of Cancer Incidence has been found to be 0.76 for CC examination, 0.88 for MLO, and 1,64 for the full mammography protocol (Table 4).
Table 4: Estimated Lifetime Attributable Risk of Cancer Incidence per 100,000 women undergoing mammography at age 45 – 55.
|
Examination |
Mean dose ( mGy ) |
Lifetime Attributable Risk of Cancer Incidence per (100 000) women |
|
CC |
1.09 | 0.76 |
|
MLO |
1.26 |
0.88 |
|
Mammography protocol |
2.35 |
1.64 |
Discussion
The MGD value for MLO projection obtained in this study was higher than the CC projection due to the important thicknesses generated by the inclusion of the pectoral muscle, increasing beam attenuation. The results of this study were consistent with those of a pilot study conducted in the United Kingdom in order to evaluate the radiation doses received by women undergoing mammography examinations, the mean dose was 1.7 mGy for the MLO projection and 1.4 for the CC projection [13]. The dose per view showed an exponential relationship to the tube time current which increase with breast thickness.
DRLs for mammography, in this study, are higher compared to that of Nigeria and Australia and lower compared to that of the United Kingdom and France (fig. 2). This difference observed in this study than those of other studies can be explained using different screening protocols and different mammography machine parameters. The results obtained is a local DRLs from a single study and may vary from one screening center to another with the change of devices and protocols, a national investigation will allow to have representative values of DRLs which intended to provide standards for dose optimization across these facilities to encourage those with median doses that exceed international guidelines to consider potential improvement avenues.
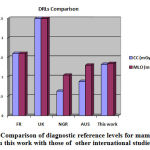 |
Figure 2: Comparison of diagnostic reference levels for mammography in this work with those of other international studies. |
In this study, we also assessed the Lifetime Attributable Risk of Cancer Incidence after mammography screening examinations, the minimum age used in this study is 45 years and the maximum is 55 years. The risk increase with MGD, with a value of 0,76 per 100,000 women, for CC view, 0,88 for MLO view, and 1,64 for full mammography procedure. This assessed risk is based on the results obtained from women with an average age of 50 years undergoing a single screening mammography procedure, however, according to the BEIR Report, the risk decreases considerably with the age, which means that the risk is higher for women who have undergone the same exposures at an early age as shown in (fig.3), and multiple examinations according to the frequencies recommended for each case.
 |
Figure 3: Lifetime Attributable Risk of Cancer Incidence per 100,000 women undergoing screening mammography examination per age. |
The same radiation doses obtained in this study may generate a much higher risk for young women who carry mutations in either the BRCA1 or BRCA2 genes and for which it is recommended to begin screening mammography at age 25 to 30 years [14][15], according to a study on estimated cancer risk from mammography procedures for young BRCA Mutation [16], the lifetime risk of radiation induced cancer mortality per 100,000 women was 260 for screening at age 25 – 29 years, 200 for screening at age 30 – 34 years and 130 for screening at age 35 – 39 years.
Therefore, it is necessary to properly account for the impact of radiation while evaluating the hazard vs benefit of screening mammography procedures [17] The risk of radiation-induced carcinogenesis is relatively small compared to the advantages of early detection, and it can be reduced by implementing a quality control protocol and all optimization procedures to reduce the patient dose and improve the image quality.
Conclusion
The MGD for this study was 1,09±0,45mGy and 1,26±0,74 mGy for craniocaudal (CC) and mediolateral oblique (MLO) respectively. Established local DRLs for mammography in this study are lower compared to that of UK and France and higher compared to that of Nigeria and Australia.
A potential risk of radiation-induced carcinogenesis exists in mammography because the breast is radiosensitive, the risk increases especially when mammographic examinations commence too early or are too frequent. Justification and optimization of screening mammography procedures, and implementation of a quality assurance system are highly recommended for the purpose of reducing the dose as much as possible without impacting image quality, as well as the establishment of National Diagnostic Reference Levels (DRLs) on which health professional could refer to optimize their practices.
Considering that the technical specifications of the machine used in this study are identical to those used in most mammography screening national centers, the results of this study can be considered as a preliminary estimation for the mammography DRLs in Morocco.
References
- Wise J. Women aged 50 to 74 should have mammogram every two years, say US guidelines. Bmj. 2016; 352:i118.
CrossRef - Pauwels EKJ, Foray N, Bourguignon MH. Breast Cancer Induced by X-Ray Mammography Screening? A Review Based on Recent Understanding of Low-Dose Radiobiology. Med Princ Pract. 2016;25(2):101-109. doi:10.1159/000442442
CrossRef - Seimenis I, Chouchos K, Prassopoulos P. Radiation Risk Associated With X-Ray Mammography Screening: Communication and Exchange of Information via Tweets. J Am Coll Radiol. 2018;15(7):1033-1039. doi:10.1016/j.jacr.2018.02.028
CrossRef - General Secretariat of the Government of Morocco. Law 142-12, Related to Nuclear and Radialogical Safety and Security and the Creation of Moroccan Agency for Nuclear and Radiation Safety and Security.
- Vañó E, Miller DL, Martin CJ, et al. ICRP Publication 135: Diagnostic Reference Levels in Medical Imaging. Ann ICRP. 2017;46(1):1-144. doi:10.1177/0146645317717209.
CrossRef - Young KC, Oduko JM. Radiation doses received in the United Kingdom breast screening programme in 2010 to 2012. Br J Radiol. 2016;89(1058). doi:10.1259/bjr.20150831
CrossRef - Zira JD, Nzotta CC. Radiation doses for mammography and its relationship with anthropo technical parameters. Int J Radiol Radiat Ther. 2018;5(5). Accessed June 20, 2020. https://medcrave.org/ index.php /IJRRT/article/view/6680.
CrossRef - Joseph DZ, Nzotta CC, Skam JD, Umar MS, Musa DY. Diagnostic reference levels for mammography examinations in North Eastern Nigeria. Afr J Med Health Sci. 2018;17(1):54.
CrossRef - Order of May 23, 2019 Approving Decision No. 2019-DC-0667 of the Nuclear Safety Authority of April 18, 2019 Relating to the Procedures for Assessing the Doses of Ionizing Radiation Delivered to Patients during a Radiology Procedure, Radio-Guided Interventional Practices or Nuclear Medicine and Updating Associated Diagnostic Reference Levels, French Government; 2019.
- Protection R. 125: Low Dose Ionizing Radiation and Cancer Risk. Commission, European. Luxembourg: sn; 2001.
- Council NR. Health Risks from Exposure to Low Levels of Ionizing Radiation: BEIR VII Phase 2.; 2005. doi:10.17226/11340
CrossRef - Rehani MM. Limitations of diagnostic reference level (DRL) and introduction of acceptable quality dose (AQD). Br J Radiol. 2014;88(1045):20140344. doi:10.1259/bjr.20140344
CrossRef - Burch A, Goodman DA. A pilot survey of radiation doses received in the United Kingdom Breast Screening Programme. Br J Radiol. 1998;71(845):517-527. doi:10.1259/bjr.71.845.9691897
CrossRef - Burke W, Daly M, Garber J, et al. Recommendations for follow-up care of individuals with an inherited predisposition to cancer. II. BRCA1 and BRCA2. Cancer Genetics Studies Consortium. JAMA. 1997;277(12):997-1003.
CrossRef - Daly MB, Axilbund JE, Buys S, et al. Genetic/familial high-risk assessment: breast and ovarian. J Natl Compr Cancer Netw JNCCN. 2010;8(5):562-594. doi:10.6004/jnccn.2010.0043
CrossRef - Berrington de Gonzalez A, Berg CD, Visvanathan K, Robson M. Estimated risk of radiation-induced breast cancer from mammographic screening for young BRCA mutation carriers. J Natl Cancer Inst. 2009;101(3):205-209. doi:10.1093/jnci/djn440
CrossRef - Løberg M, Lousdal ML, Bretthauer M, Kalager M. Benefits and harms of mammography screening. Breast Cancer Res BCR. 2015;17:63. doi:10.1186/s13058-015-0525-z
CrossRef







