Sheikha Nasser said Al-Shidhani1, Shadia Al-Sinawi2, Maiya Al-Bahri2, Masoud Al-Kindi3 and Mohamed Mabruk1
1Department of Allied Health Sciences, College of Medicine and Health Sciences, Sultan Qaboos University, Oman.
2Department of Pathology, College of Medicine and Health Sciences, Sultan Qaboos University, Muscat, Oman.
3Department of Pathology, Armed Forces Hospital, Muscat, Oman.
Corresponding Author E-mail: mabruk@squ.edu.om
DOI : https://dx.doi.org/10.13005/bpj/2121
Abstract
Background: Nasopharyngeal carcinoma(NPC) is a rare malignant carcinoma that develops in the epithelial lining of the nasopharyngeal mucosa It is the most common neoplasm of the Nasopharynxand it is associated with many risk factors; one of them is Epstein-Barr virus infection. An Epstein-Barr virus is a tumorigenic herpes virus that infects and persists in B-lymphocytes without causing disease. This virus is associated with significant pathological conditions, such as benign and malignant lymphoproliferation.
Objectives: To determine Epstein -Barr encoded RNA 1&2 (EBER1,2) and latent membrane protein (LMP) expressionin formalin-fixed paraffin-embedded tissue samples obtained from Omani patients diagnosed with nasopharyngeal carcinoma.Also, to identify the pattern and the type(s) of cells infected with EBV in nasopharyngeal carcinoma tissue samples obtained from Omani patients. Moreover, to compare the sensitivity of Immuno histochemistry and in-situ Hybridization for the detection of EBV in the nasopharyngeal carcinoma tissue sample.
Materials and Method:Thirteen formalin-fixed paraffin-embedded nasopharyngeal carcinoma tissue samples archived from the period 2010 to 2017, were obtained from the Pathology Departments of Sultan Qaboos University Hospital and the Armed Force Hospital. These tissue samples were processed using two different methods Immunohistochemistry (IHC) and In situ hybridization (ISH).
Results:Eleven out of thirteen NPC Omani patients were positive for EBV (84.61%) by either LMP-IHC or EBER-ISH. All cells stained positive for EBV in NPC tissue samples was of malignant type rather than normal cell type. EBV is mostly detected in patients in the age group of less than 50 years old. Also out of the 13 NPC patients, seven females (58.34%), and six males (46.15%) were positive for EBV.
Conclusion:This study may provide evidence indicating an association between EBV and nasopharyngeal carcinoma. In addition, the detection of EBV in NPC obtained from Omani patients may encourage the physician to consider using anti-herpes virus drugs in the treatment of EBV positive NPC patients as an additional tool for the treatment of this kind of malignancy.
Keywords
Epstein Barr virus; Nasopharyngeal Carcinoma; Omani patients
Download this article as:| Copy the following to cite this article: Al-Shidhani S. N. S, Al-Sinawi S, Al-Bahri M, Al-Kindi M, Mabruk M. Determination of the Expression of Latent Epstein Barr virus in Omani Nasopharyngeal Carcinoma Patients. Biomed Pharmacol J 2021;14(1). |
| Copy the following to cite this URL: Al-Shidhani S. N. S, Al-Sinawi S, Al-Bahri M, Al-Kindi M, Mabruk M. Determination of the Expression of Latent Epstein Barr virus in Omani Nasopharyngeal Carcinoma Patients. Biomed Pharmacol J 2021;14(1). Available from: https://bit.ly/3ujlTgn |
Introduction
Nasopharyngeal carcinoma is a rare malignant carcinoma that develops in the epithelial lining of the nasopharyngeal mucosa1. It is the most common neoplasm of the nasopharynx, and it differs from other cancers of the head and neck in its occurrence, unique etiological associations, clinical behaviour and treatment 2. The incidence of this type of malignancy is very rare (less than 1 in 100.000) in most populations3, but it is relatively common in males of Western North Africa 4. In Asian countries, 50 years old is generally the mean age of NPC patients5. In the Omani population, 40% of the total cases of NPC were reported from the capital city Muscat, and about 21% were reported from Ash Sharqiyah region6. Besides, 17% of cases were reported from both Al-Batinah and Dhofar regions 6.
In high-risk areas, the undifferentiated carcinoma of nasopharyngeal type (UCNT) is the most dominant histopathological type3. Moreover, NPC associated risk factors include genetic susceptibility, Epstein Barr virus (EBV) infection, ecological risk factors 3,7. Also, certain dietary factors such as salted fish consumption is another factor that may contribute to the development of NPC6. Elevated antibody titers against Epstein Barr virus and a certain human leukocyte antigen class I genotypes are considered as well as a risk factors of NPC 8.
Epstein-Barr virus (EBV) was first identified in a biopsy culture obtained fromBurkitt lymphoma patients in 1964 9. EBV is a tumorigenic herpesvirus that infects and persists in B-lymphocytes without causing disease 9. In most cases, infection with EBV remains latent; however, in a few cases, it is associated with significant pathological conditions, such as benign and malignant lymphoproliferation9.
This virus has shown the ability to contribute to oncogenesis as it frequently detected in tumour tissue samples like Burkitt lymphoma, Hodgkin’s disease, and post-transplant B cell lymphomas10. In UCNT (The undifferentiated carcinoma of nasopharyngeal type), the EBV infection presents at an early stage of tumour development, which is evident by the usual presence of the EBV genome in a circular and monoclonal episomal form in the tumour cells 11.
Latent membrane protein 1 (LMP1) which is a critical EBV oncogene 3, is a transmembrane protein with two important properties, the first is its potent cell signalling properties and the second is the tumorigenic transformation properties 12. LMP1 is capable of inducing cancer progenitor cell-like phenotyping in epithelial cells, which may contribute to the progression of nasopharyngeal carcinoma 13. Transformation and immortalization of cells by LMP1 is done through directing the signalling pathways that stimulate cell proliferation and block apoptosis 14. Many different downstream pathological changes can be caused by LMP1 including cell proliferation, apoptosis and metastasis15. LMP has the capabilitiesof activating several oncogenic signalling pathways such as NF-kB, JNK and MAPK15.
Epstein-Barr virus-encoded RNA (EBER), which have two types EBER1 and EBER2, is a non-polyadenylateduntranslated RNAs of 167 (EBER1) and 172 (EBER2) nucleotides long, and it is transcribed by RNA polymerase III 16. Besides, both EBER1 and EBER2 contribute to the oncogenesis of EBV, the transforming ability of recombinant EBVs expressing EBER2 was as high as thatof EBVs expressing both EBER1 and EBER217.The way by which EBERscontribute to the efficient growth transformation of B-lymphocytes is by enhancing thegrowth potential of the transformed lymphocytes16.
Materials and Methods
Specimens
Thirteen formalin-fixed paraffin-embedded nasopharyngeal carcinoma tissue samples collected and archived from the period 2010 until 2017,were included in the present study. These samples were obtained from the Pathology Departments of SQUH and the Armed Force Hospital in Muscat/Oman. Also, the patient information including diagnosis, age, gender and MRN of each sample wasrecorded. The research ethical approval for the present study was obtained from the Research Ethics Committee of the College of Medicine and Health Sciences, Sultan Qaboos University, Muscat, Oman (MREC # 1495).
Tissue processing
Tissue processing for both Immunohistochemistry (IHC)and in situ hybridization (ISH), were carried out as described previously18,19. Briefly, the nasopharyngeal carcinoma formalin-fixed paraffin-embedded tissue samples were cut into sequential 4 µm sections using the microtome (Thermo Scientific).
From each tissue sample,3 sectionswerecut and one was used for Haematoxylin and Eosin staining (H&E)and the other 2 sequential sections bounded covalently to the glass slides, where onewas used for in situ hybridization (ISH) and the other onewas used for Immunohistochemistry (IHC)analysis. After sectioning the slides were incubated in 60 0C oven for one hour.
Positive controls consisited of Hodgkins Lymphoma tissue sample was included in each experiment. In addition, a negative control, was included in each experiment in which the primary antibody /EBERs probe was omitted and replaced with a buffered saline.
Immunohistochemistry
Immunohistochemistry was carried out on nasopharyngealtissue(NPC), samples using the Envision Flex+ High pH (Ref K8002, Dako) in accordance with the manufacturer’s instructions. Prior to staining the sections were deparaffinized twice through two changes of xylene, each xylene change was carried out for 5 minutes. Then, sections were hydrated in three changes of graded ethanol, each for 5 minutes followed by heat-induced epitope retrieval using the target high pH solution in the detection kit according to the package insert for the primary antibody. Subsequently, tissue sections were incubated in EnVision Flex Peroxidase-Blocking Reagent (SM801) for 10 minutes to block the endogenous peroxidase activity. This was followed by washing in Envision Flex Wash Buffer (TBS-DM831) (Dako, Denmark) for 5 minutes. Immunohistochemistry on processed tissue sections was carried out by the incubation of NPC tissue sections for 60 minutes at 370C with primary antibody consisted of mouse monoclonal antibody against EBV-encoded LMP (clone: CS, 1-4 and isotype: IgG1, kappa, Dako, Denmark), followed by incubation at room temperature for 30 minuteswith biotinylated secondary antibody. The secondary polyclonal antibody used in the present study consisted of dextran coupled with peroxidase molecules ( Dako Envision Flex/HRP SM802). Then, 3,3-diaminobenzidine tetra hydrochloride (DAB) was add as ana chromogen. The DAB chromogen gave a brown colourstain over the target site (EBV LMP protein). Mayer’s Haematoxylin stain was used as a counterstain.
In situ hybridization (ISH)
The expression of EBER1 and EBER2of EBVin NPC tissue samples was carried out by using the Inform EBER Probe (800-2842, Ventana Medical Systems, Roche Diagnostics GmbH, Mannheim Germany). The EBERs positive signals in tissue samples were detected by Ventana ISH/View Blue detection Kit (Ref: 853-2193). In situ hybridization experiment was performed using (Ventana Bench Mark Ultra, Medical Systems Inc, Tucson, AZ, USA) following manufacturer instructions.
Data analysis
SPSS version 23 was used for data analysis. Frequency tables and pie charts or bar charts have been used to display percentages for categorized variables, and continuous variables have been shown as Mean ± SD and error bar charts. For the analysis, to test the significance of the association between categorized variables, the chi-square test was used.
Results
Epstein-Barr virus (EBV) expression in NPC tissue samples
The expression of Epstein-Barr virus (EBV) was detected in the present study by usingtwo different technical approaches,In-situ hybridization for the detection of EBER and Immunohistochemistry for the detection of LMP protein of EBV formalin-fixed paraffin-embedded NPC tissue samples obtained from Omani patients.
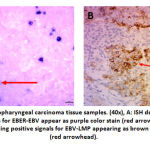
The results for the expression of EBV-LMP and the expression of EBV-EBER are summarized inTable.1.Positive cases were considered positive if they are positive by either one of the techniques (ISH or IHC). Eleven out of thirteen NPC Omani patients’ tissuesampleswere positive for EBV (84.61%) by either LMP-IHC or EBER-ISH; five of them were positive by both LMP-IHC and EBER-ISH (about 38.46%) while four of them were positive only by EBER-ISH (about 30.76%).Also, one of the cases was positive by LMP-IHC only.The results of EBER-ISH and LMP-IHC NPC positive cases are shown in Table.1 and Figure.1.The EBV positive NPC tissue samples detected by EBER-ISH (69.23%) is higher than that of LMP-IHC (53.84%). This may indicate that the sensitivity and specificity of EBER-ISH arehigher than that of LMP-IHC for the detection of EBV.
Table 1: The expression of EBER and LMP in Nasopharyngeal carcinoma in Omani patients.
| EBER-EBV
positivity by ISH (%) |
LMP-EBV
positivity by IHC (%) |
Total positive cases | Total number of cases |
| 9 (69.23%) | 7 (53.84%) | 11 (84.61%) | 13 (100%) |
The staining pattern of EBV expression/lymphocytic infiltration.
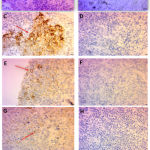
The pathological examination of the NPC tissue sections stained with Haematoxylin and Eosin and the interpretation of IHC and ISHresults was carried out by independent Pathologist. In the seven positive cases, latent Membrane Protein (LMP) staining of EBV was Cytoplasmic and Membranous [Figure.1: B, Figure.2: C, E,G] [Table.2], while in EBER positive cases the staining pattern was Nuclear [Figure.1:A; Table.3]. The integrity of the staining in LMP-IHC ranges from mild to moderate to strong (Table 2; Figure.2: C, E, G]; however, strong staining integrity was seen in EBER-ISH [Table.3; Figure.1:A]. In addition, all cells stained positive by both ISH and IHC was of malignant type rather than normal cell type. Examples of staining pattern of EBER-ISH and LMP-IHC positive cases are shown in Figures.1,2.
Table 2: The integrity of staining, staining patterns and the type cells stained positive by LMP-EBV.
| Cases | Integrity of staining | Staining pattern | Type of cells stained positive |
| Case 1 | Mild | Cytoplasmic and Membranous | Malignant cells |
| Case 2 | Moderate | ||
| Case3 | Moderate | ||
| Case4 | Mild | ||
| Case5 | Strong | ||
| Case6 | Moderate (patchy) | ||
| Case7 | Mild |
Table 3: The integrity of staining, staining patterns and the type cells stained positive by EBER-EBV.
| Histo# | Integrity of staining | Staining pattern | Type of cells stained positive |
| Case 1
Case 2 Case 3 Case 4 |
strong | Nuclear | Malignant cells |
The degree of lymphocytic infiltration in correlation to positive and negative cases was detected. Mild to moderate (7.143%), moderate (35.71%), and moderate to severe (7.143%) lymphocytic infiltration was observed in positive cases with LMP-IHC, while negative cases showed a similar degree of sparse, mild, andmoderateof lymphocytic infiltration(16.67%) [Figure.2: A].Also, Haematoxylin and Eosin stain for NPC tissue samples showed a fibro collagenous tissue densely infiltrated by lymphocytes [Figure.2: A].
EBV gene expression in correlation to age and gender:
Thirteen NPC patients(from 2010-2017)were divided into two age groups, < 50 years old and ≥50 years old. The first group (< 50 years) includes seven cases, four of them were positive for LMP-IHC (57.14%), while five of them were positive for EBER-ISH (71.42%). The second age group (≥50 years) included6 cases, three of them were positive for LMP-IHC (50%), and four of them were positive for EBER-ISH (66.66%) [Table.4] [Figure.3]. The P-Value for both positivity by LMP-IHC and EBER-ISH shows a value higher than 0.05, which means that the association between the age and the positivity of both LMP and EBER is not statistically significant.
Table 4: The frequency of EBV positive cases in NPC (2010-2017) in correlation with Gender and Age.
| AGE | Number of Cases | LMP-EBV Positivity by IHC (%) | EBER-EBV Positivity by ISH (%) |
| < 50 years | 7 | 4 (57.14%) | 5 (71.42%) |
| ≥ 50 years | 6 | 3 (50%) | 4 (66.66%) |
| Total | 13 | 7 | 9 |
| P-value | – | 0.797 | 0.853 |
In relation to gender, out of the thirteen cases included in this study seven of them were female, and the rest six were males. Five out of the seven females were positive for LMP-IHC (71.42%), while six of them were positive for EBER-ISH (85.71%). In the male’s category, two of them were positive for LMP-IHC (33.33%), and three of them were positive for EBER-ISH(50%) [Table.5] [Figure.3].The P-Value for both positivity by LMP-IHC and EBER-ISH shows a value higher than 0.05, which means that the association between the gender and the positivity of both LMP and EBER is not significant.
Table 5: The frequency of EBV positive cases in NPC (2010-2017) in correlation with Gender.
| GENDER | Number of Cases | LMP-EBV Positivity by IHC (%) | EBER-EBV Positivity by ISH (%)) |
| Female | 7 | 5 (71.42%) | 6 (85.71%) |
| Male | 6 | 2 (33.33%) | 3 (50%) |
| Total | 13 | 7 | 9 |
| P-value | – | 0.170 | 0.164 |
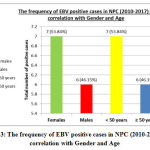 |
Figure 3: The frequency of EBV positive cases in NPC (2010-2017) in correlation with Gender and Age. |
Discussion
Nasopharyngeal carcinoma hasa very rare incidence (less than 1 in 100.000) in most populations 3.The mean age of developing NPC worldwide is of 50 years old in most Asian countries 5. In contrast, this study shows that the mean age of Omani patients with NPC was 47 years old, which could be considered close to that of Asian countries. The number of samples in the present study (Thirteen cases) demonstrates the very rare incidence of this type of malignancy in Oman6.
There are different techniques used for the detection of Epstein-Barr virus (EBV), including immunohistochemistry (IHC), in situ hybridization (ISH), and polymerase chain reaction (PCR). The present studyshowed thateleven out of thirteen NPC Omani patients were positive for EBV by either LMP-IHC or EBER-ISH (84.6%), however, the positivity of EBER-ISH (69.23%) is higher than that of LMP-IHC (53.84%). This indicates that the sensitivity and specificity of EBER-ISH arehigher than that of LMP-IHC for the detection of EBV.However, these findings are not of that significantas this could be due to the low number of samples used in the present study. Thisfinding is similar to some degree to the finding ofanother study, which showed that EBER-ISH is more sensitive and more reliable than LMP-IHC for the detection of EBV in formalin-fixed paraffin-embedded tissue samples20.
Most of the EBV positive cases were foundin female category (58.34%), precisely out of the thirteen cases included in the present study seven of them were female, and the rest six were males (46.15%).This shows that EBV associated Nasopharyngeal carcinoma is more common in females than males among patients in Oman. This is different from the findings of other studies,which found that EBV is more prevalent in male NPC patients than females 7. However, in the present study,the P-Value for both positivity by LMP-IHC and EBER-ISH in correlation to age and gender shows a value higher than 0.05, which indicates that the association between both the age and the gender and the positivity of both LMP and EBER is statistically non-significant. In addition, the results of the present study, show that EBV associated nasopharyngeal carcinoma are more prevalent in patients with the age of less than 50 years old (53.84%) in comparison to the age group ≥ 50 years old (46.15%). This is similar to a study carried outon the Sudanese population which found that the EBV associated NPC were seen mostly among the age group of 21-40 yearsold2,7. Moreover,in the present study, all cells stained positive was of malignant type rather than normal cell type. This may indicate a relation between Epstein Barr Virus (EBV) and the pathogenesis of nasopharyngeal carcinoma.
The degree of lymphocytic infiltration ranged from sparse to mild to moderate to severe in some cases.In addition, as the results of the present study showed that there was a correlation between the positivity for LMP-IHC and the degree of lymphocytic infiltration; where a higher degree of lymphocytic infiltration was detected in positive cases for LMP-IHC. Similarly, other studies validate this correlation between the positivity of EBV and the consistency of lymphocytic infiltration21,22.
In conclusion, this study aimed to determine the expression of latent Epstein-Barr virus in Omani nasopharyngeal carcinoma patients. The importance of this study originated from the need to determine the prevalence of EBV in Omani patients with NPC especially that the prevalence of latent EBV infection is considered as a risk factor of NPC. The present study showed a clear association between EBV and NPC among Omani patients, especially, that all cells stained positive for EBV was of malignant type rather than normal cell type. This indicatesthat EBVinfection may play a role in the pathogenesis of NPC. The detection of EBV in NPC obtained from Omani patients may encourage the physician to consider using anti-herpes virus drugs in the treatment of EBV positive NPC patients as an additional tool for the treatment and the management of this kind of malignancy.
Acknowledgement
The authors would like to thank the head and all the staff at the Department of Pathology at Sultan Qaboos University Hospital for their help and support and for allowing us to use their Departmental and laboratory facilities.The authors would also like to thank the Pathology Department/Armed Force Hospital for all of their help and support.
Conflict of interest
The authors declare no conflict of interest.
Funding source
The present study was not funded by any grant.
References
- Borthakur P , Kataki K , Keppen C , Khamo V , Medhi D , Deka M. Expression of Epstein Barr Virus Encoded EBNA1 and LMP1 Oncoproteinsin Nasopharyngeal Carcinomas from Northeast India”. Asian Pacific Journal of Cancer Prevention 17(7): 3411-341 (2016).
- Beena U, and Ahmed R. “Nasopharyngeal Carcinoma, An Analysis Of Histological Subtypes And Their Association With EBV, A Study Of 100 Cases Of Pakistani Population”. Asian Journal of Medical Sciences5(4): 16-20(2014).
CrossRef - Banko A,Lazarevic I, Folic MM. Characterization Of The Variability Of Epstein-Barr Virus Genes In Nasopharyngeal Biopsies: Potential Predictors For Carcinoma Progression”. PLOS ONE11(4):1-16 (2016): e0153498.
CrossRef - Bernadette B Nasopharyngeal Carcinoma”. Orphanet Journal of Rare Diseases: 1:23. (2006). doi:10.1186/1750-1172-1-23
CrossRef - Gamoudi A, Fourati A, BiazigN.Complementary Determination Of Epstein-Barr Virus DNA Load And Serum Markers For Nasopharyngeal Carcinoma Screening And EarlyDetection In Individuals At Risk In Tunisia”. European Archives of Oto-Rhino-Laryngology269(3): 1005-1011(2012).
CrossRef - Al-Azri, AbdulAziz, and Salma Al-Sheibani. “Nasopharyngeal Carcinoma In Oman: A Descriptive Analysis”. Oman Medical Journal30(3): 167-172(2015).
CrossRef - Ahmed GD, Suliman RS, El Aziz Mand, Alshammar FD. Molecular Detection Of Epstein – Barr Virus In Nasopharyngeal Carcinoma Among Sudanese Population”. Infectious Agents and Cancer11(1):1-5(2016)
CrossRef - Chang, E. and Adami, H.. The Enigmatic Epidemiology of Nasopharyngeal Carcinoma. [online] Cancer Epidemiol Biomarkers Prev;15(10):1765-1777(2006)
CrossRef - Williams, H., and Dorothy H.crawford. “Epstein-Barr Virus: The Impact Of Scientific Advances On Clinical Practice”. Blood107(3): 862-869(2006)
CrossRef - Young, Lawrence S, and Paul G Murray. “Epstein–Barr Virus And Oncogenesis: From Latent Genes ToTumours”. Oncogene22(33): 5108-5121(2003).
CrossRef - Rey J,Xerri L,Bouabdallah R, Keuppens M,Brousset P, Meggetto F. Detection Of Different Clonal EBV Strains In Hodgkin Lymphoma And Nasopharyngeal Carcinoma Tissues From The Same Patient”. British Journal of Haematology142(1): 79-81(2008).
CrossRef - Jun Zhang , Lin Jia, Weitao Lin , Yim Ling Yip , Kwok Wai Lo , Victoria Ming Yi Lau, Sai WahTsao. Epstein-Barr Virus-Encoded Latent Membrane Protein 1 Upregulates Glucose Transporter 1 Transcription Via The Mtorc1/NF-Kb Signaling Pathways. Journal of Virology91(6): 1-20(2017).
CrossRef - He, Jiang.Positive Regulation Of TAZ Expression By EBV-LMP1 Contributes to Cell Proliferation and Epithelial-Mesenchymal transition In Nasopharyngeal Carcinoma”. Oncotarget; 8(32): 52333–52344.
CrossRef - Yang S, Li S-S, Yang XM, YinDan‑Hui, Wang L. “Embelin Prevents LMP1-Induced TRAIL Resistance Via Inhibition Of XIAP In Nasopharyngeal Carcinoma Cells”. Oncology Letters11: 4167-4176(2016).
CrossRef - Lu, J., Tang, M., Li, H., Xu, Z., Weng, X., Li, J., Yu, X., Zhao, L., Liu, H., Hu, Y., Tan, Z., Yang, L., Zhong, M., Zhou, J., Fan, J., Bode, A. M., Yi, W., Gao, J., Sun, L., & Cao, Y. (2016). EBV-LMP1 suppresses the DNA damage response through DNA-PK/AMPK signaling to promote radioresistance in nasopharyngeal carcinoma. Cancer Letters, 380(1), 191-200. https://doi.org/ 10.1016/ j.canlet.2016.05.032(2016).
CrossRef - Yajima, M., Kanda, T. and Takada, K. Critical Role of Epstein – Barr virus (EBV)-Encoded RNA in Efficient EBV-Induced B-Lymphocyte Growth Transformation. Journal of Virology;79(7):4298-4307 (2005).
CrossRef - Wu, Y., Maruo, S., Yajima, M., Kanda, T. and Takada, K.. Epstein – Barr virus (EBV)-Encoded RNA 2 (EBER2) but Not EBER1 Plays a Critical Role in EBV-Induced B-Cell Growth Transformation. Journal of Virology; 81(20): 11236-11245(2007)
CrossRef - Mabruk, M., Flint, S., Coleman, D., Shiels, O., Toner, M. and Atkins, G. A rapid microwave-in situ hybridization method for the definitive diagnosis of oral hairy leukoplakia: comparison with immunohistochemistry. Journal of Oral Pathology and Medicine;25(4):170-176(1996).
CrossRef - Yunos A, Mabruk M. “Detection Of Epstein-Barr Virus In Lower Gastrointestinal Tract Lymphomas”. Molecular Diagnosis & Therapy 10(4): 251-256(2006).
CrossRef - Nonogaki, S., Shirata, N., Kimura, L., Guerra, J., Medeiros, R., Paes, R., Kanamura, C., Oliveira, C. and Menezes, Y. Comparative study of five commercial probes for the detection of Epstein-Barr virus (EBV) by in situ hybridization in cases of nodular sclerosis Hodgki’s lymphoma. JornalBrasileiro de Patologia e Medicina Laboratorial.JornalBrasileiro de Patologia e Medicina Laboratorial 52(6). 5935/1676-2444.20160065; (2016)
CrossRef - Chu, P., Chang, K., Chen, Y., Chen, W. and Weiss, L.. No Significant Association of Epstein-Barr Virus Infection with Invasive Breast Carcinoma. The American Journal of Pathology; 159(2) :571-578(2001).
CrossRef - Abe, T., Shinohara, N., Tada, M., Harabayashi, T., Sazawa, A., Maruyama, S., Moriuchi, T., Takada, K. and Nonomura, K.. Infiltration of Epstein-Barr virus-harboring lymphocytes occurs in a large subset of bladder cancers. International Journal of Urology; 15(5):429-434(2008).
CrossRef