Ivan H Hadisaputra1 , Gede Suwedagatha1
, Gede Suwedagatha1 and Tjokorda GdeBagus Mahadewa2*
and Tjokorda GdeBagus Mahadewa2*
1Department of Surgery, Faculty of Medicine, Udayana University/Sanglah General Hospital, Bali, Indonesia
2Department of Surgery, Faculty of Medicine, Udayana University Jl. PB Sudirman, Denpasar 80232, Bali, Indonesia
Corresponding Author E-mail: tjokmahadewa@unud.ac.id
DOI : https://dx.doi.org/10.13005/bpj/2122
Abstract
Background: The Trauma and Injury Severity Score (TRISS) is the most applied tool to predict the multi trauma outcome. It is shown that the predictive value of TRISS could be improved by adjusting the coefficient. Originally this study aims to evaluate our hospital in treating multitrauma patients, with good outcome we propose adjustment to TRISS formula.
Methodology:This study is a diagnostic test to determine the accuracy of TRISS scores to predict mortality of multitrauma patients treated in Sanglah General Hospital.
Result: Fifty two multitrauma patients with ISS score > 18 with at least 2 body regions being injured. The TRISS diagnostic test was obtained with a sevsitivity 81.8%, specificity 97.6%, positive predictive value 90%, negative predictive value 95.2%, prevalence 21%, accuracy rate of 94.2%.
Conclusion: Adjustment to TRISS formula coefficient for better prediction is proposed. Physiological parameter in RTS that does not include respiratory rate shows reliable prediction, which can be used in emergency setting when anatomical diagnostic has not yet to be obtained.
Keywords
Multi Trauma; RTS; TRISS; Revised Score
Download this article as:| Copy the following to cite this article: Hadisaputra I. H, Suwedagatha G, Mahadewa T. G. Adjustment of Trauma and Injury Severity Sccore (TRISS) and Revised Trauma Score (RTS) in Predicting Mortality of Multitraumapatients in Sanglah Hospital Bali. Biomed Pharmacol J 2021;14(1). |
| Copy the following to cite this URL: Hadisaputra I. H, Suwedagatha G, Mahadewa T. G. Adjustment of Trauma and Injury Severity Sccore (TRISS) and Revised Trauma Score (RTS) in Predicting Mortality of Multitraumapatients in Sanglah Hospital Bali. Biomed Pharmacol J 2021;14(1). Available from: https://bit.ly/3ckQhkJ |
Introduction
The Trauma and Injury Severity Score (TRISS) is the most widely used tool to predict the outcome of trauma patients. Initially TRISS was made in 1983 using a combination of the patient’s age, Injury Severity Score (ISS), and Revised Trauma Score (RTS) to predict the probability of patient safety. The TRISS coefficient was measured using an ordinary logistic regression model in 1987, and was revised in 1995 by American College of Surgeons Committee on Trauma Coordinated Major Trauma Outcome Study (MTOS).1,2In 2010, TRISS coefficients were further revised using data obtained from the American College of Surgeons Committee on the Trauma National Trauma Data Bank (NTDB) and NTDB National Sample Project (NSP).1,2,3
TRISS system combines injury assessments based on physiological (RTS) and anatomical (ISS) status, with age and trauma mechanism (blunt or penetrating) to calculate the safety probabilities of each individual patient. TRISS has the best prediction rate for patients with multiple injuries due to blunt trauma. The TRISS methodology is currently used as a standard for adjusting performance standards in America, and has been widely accepted in many parts of the world.4,5
Since it was first implemented, many attempts have been made to improve TRISS through recalibration of the coefficients, careful consideration and inclusion of missing data, or through new or specifically modified variables. Recently it has been demonstrated that an important and fundamental development in predicting the power of TRISS is to make a simple re-classification of variable components and treat variable categories nominally in the logistic regression model.1,6
Methods
This is diagnostic research that underwent from June 2018 to December 2019 in Sanglah General Hospital. Ethical approval was granted by Udayana University Medicine Faculty / Sanglah Hospital’s Research Ethical Comitee, without informed consent needed.
The inclusion criteria is multi-trauma patients who suffered injuries on two body regions or more with AIS score of each ≥ 3 in.7 The exclusion criteria are patients with comorbid that can affecting outcome, i.e chronic heart failure, diabetes mellitus, chronic obstructive pulmonary disease, chronic kidney disease. The TRISS score obtained was divided into two categories, where the probability of survival ≤ 33.3% were included in the deceased category, and the probability of survival > 33.3% was included in the survivors category.8,9 All patients received therapy according to protocol standards.
We collected data comprised of patient characteristic, age, gender, prehospital time, mechanism of injury, trauma type, hospital length of stay, Glasgow Coma Scale (GCS) score, systolic, and respiratory rate. The patients were followed-up through their stay in the hospital and the final outcomes were noted, either patients have deceased or survive. Data analysis was undertaken in SPSS version 23.
Result
There were 52 multi-trauma patients admitted to Sanglah Hospital during the study period (Table 1). The mean age of patients was 32.4 years, with 94.2% of them aged <55 years. The ratio of male to female was 7.6:1. Fifty-one patients experienced a blunt trauma injury, of which 85% were traffic accidents, while only one patient had a penetrating injury due to a knife stab. The head and neck were the organs most frequently injured, which were found in 35 patients (67.3%), followed with extremities (50%), face (48.1%), external (40.4%), thorax (38.5%), and abdomen (28.8%). The observed mortality rate was 21.2% (11 cases), with a predicted mortality rate of 19.2% (10 patients)
Table 1: Epidemiology and clinical data
| Variable | Deceased | Survivors | Total | p-value |
| Age (years), n(%)
< 55 ≥ 55 |
10 (20.4%) 1 (33.3%) |
39 (79.6%) 2 (66.7%) |
49 (94.2%) 3 (5.8%) |
0.518 |
|
Gender, n(%) Male Female
|
8 (17.4%)
3 (50%) |
38 (82.6%)
3 (50%) |
46 (86.5%)
6 ( 13.5%) |
0.101 |
| Mechanism of injury, n(%)
Traffic accident Fall from heights Natural disaster Criminal
|
10 (22.2%)
1 (20%) – – |
35 (77.8%)
4 (80%) 1 (100%) 1 (100%) |
45 (86.5%)
5 (9.6%) 1 (1.9%) 1 (1.9%) |
0.50 |
| Trauma Type, n(%)
Blunt Penetrating |
11 (21.5%) – |
40 (88.5%) 1 (100%) |
51 (98%) 1 (2%) |
1.00 |
| Prehospital Time, n(%)
< 1 hour 1-3 hours > 3 hours
|
2 (25%)
5 (20%) 4 (21%) |
6 (75%)
20 (80%) 15 (79%) |
8 (15.4%)
25 (48.1%) 19 (36.5%) |
0.873 |
| Hospital length of stay (days), mean±SD | 3.27 (SD 3.3) | 14 (SD 9.6) | 11.57 (SD 9.7) | |
| Respiratory Rate
10-29 >29 6-9 1-5 0 |
4 (9.7%)
– 2 (66.7%) 3 (100%) 2 (100%) |
37 (80.3%)
3 (100%) 1 (33.3%) – – |
41 (78.8%)
3 (5.7%) 3 (5.7%) 3 (5.7%) 2 (3.8%) |
<0.001 |
| GCS
15-13 12-9 8-6 5-4 3 |
2 (6.1%) – 3 (75%) 2 (100%) 4 (100%) |
31 (93.9%) 9 (100%) 1 (25%) – – |
33 (63.5%) 9 (17.3%) 4 (7.7%) 2 (3.8%) 4 (7.7%) |
<0.001 |
By using a 33.3% cut-off point, 9 patients were predicted to die, of which 11 were deceased, with a sensitivity of 81.8% and a specificity of 97.6%. PPV was obtained at 90%, and NPV 95.2%, Accuracy Rate was 94.2% with the prevalence of death among multitrauma patients at 21% (Table 2).
Table 2: A 2×2 table of diagnostic values of the TRISS
| TRISS | Actual outcome | Total | |
| Deceased | Survivors | ||
| Deceased (≤33.3) | 9 | 1 | 10 |
| Survivors (>33.3) | 2 | 40 | 42 |
| Total | 11 | 41 | 52 |
ROC analysis shows that the area under the ROC curve is 0.897±0.071 (95% confidence interval= 0.758-1.000). An optimal cut-off point analysis has been done to get the best sensitivity and specificity values where the optimal value is between 43.7%-31.05%(Figure 1).
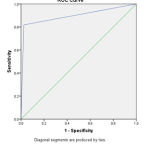 |
Figure 1: ROC analysis shows that the area. |
In this study with a specificity of 97.6%, it can be obtained an equation to determine the mortality rate of multitrauma patients:
Mortality=─ 0.717 + (─0,046 x RR) + (0,380 x Sys) + (0,297xGCS) + (─0,45xISS) + (0,038 x Age) + (0,069 x Trauma Type)
Where RR, Sys, and GCS are used are categories according to the RTS scoring system. Age <55 years = 1, and age ≥ 55 years = 2. Blunt injury = 1, and penetrating injury = 2.
Another simplerRTS equation (without respiratory rate) also obtained for faster tools in triage setting :
Mortality = -0.659 + (0,35 x Sys) + (0,255 x GCS)
Discussion
One of the problems with the multi trauma approach is that the profile of the patient varies with the type and severity of the injury. The heterogeneity and difficulty of adjusting for these variations have stimulated scientific research.8
A diagnostic test of TRISS score with a sample size of 52 was performed, at a cut-off point of 33.3%, a sensitivity of 81.8% was obtained, and specificity 97.6%, PPV 90% and NPV 95.2%, Prevalence 21%, Accuracy Rate 94.2%. In accordance with research by Gunawanet al at CiptoMangunKusumo Hospital, the sensitivity was 84.6% and 81.8% using an intersection point <90.5%.10,11 The outcome evaluation based on TRISS by Siritongtaworn, obtained a sensitivity of 90.9%, and a specificity of 97.2% with a cut-off point of 95%. Gorelik et al stated that in Florida there were no significant differences in trauma patient deaths between before and after the initiation of a surgical education program.12,13,14So it can be concluded that Sanglah Hospital as an Educational Hospital in providing health services does not reduce the quality of services provided.
RTS was obtained from a combination of 3 categories, the Glasgow Coma Scale (GCS), systolic blood pressure, and respiratory rate, which RTS calculation was obtained with an average of 6.86 (with a deviation of 1.49), ranging from 2,198-7,841. The mean RTS in died patients was 4.56 ± 1.63, and in living patients was 7.48 ± 0.57. Ranti et al stated that the cut-off point used by RTS was 5.88, where the mortality rate in the RTS 5-6 range was 81.92%.15In this study we found that RTS <5 had a mortality of 100%. The weakness of this RTS score is that it does not take into account prehospital time, where patients who experiencing shock in a shorter time will certainly have a worse prognosis than patients with longerprehospital time but the hemodynamic conditions just shows symptoms of shock recently.16,17According to Dinhet al patients with prehospital time which in the Golden hour (less than 1 hour) there were no significant advantages compared to patients who came with prehospital time more than 1 hour.18 Tien et al reported that patients with head injuries showed good results in patients who came at the golden hour.19Osterwalderet al reported no difference in mortality in patients who present with a prehospital time of less than 1 hour or more.20 RTS is a good scoring tool in predicting mortality in multitrauma patients.
Uncontrolled bleeding is the main cause in multitrauma which is the cause of prehospital death up to 35%. Systolic blood pressure <90 mmHg has been generally accepted as a limit for hypotension. But lately this concept has been controversial, where systolic blood pressure 90-109 mmHg in trauma patients or in the operating theatreshows worse outcomes than systolic blood pressure> 110 mmHg.21
Among the vital signs in RTS, the respiratory rate is still debatable. Respiratory rate has the lowest weight in RTS calculation compared to systolic and GCS, and is measured clinically which has low reproductive rate. Respiratory rate also has a very wide normal range, moreover respiratory rate does not correlate with ventilation and / or oxygenation disorder in trauma patients, which are often caused by pain and pyschological stress.22,23
We found 8 patients with an ISS score ≥ 50 where the mortality rate was 50%. This is in accordance with research from Boyd et al where the ISS 50 value gives a mortality rate of 50%. The most common organs injured were head and neck at 67.3%, followed by extremities (50%), face (48.1%), external (40.4%), thorax (38.5%), and abdomen (28.8%). The injured body region has a distribution similar to other studies, where the head is the organ most frequently injured, followed by the extremity.24,25In this study, head injuries with AIS score 5is the cause of death of most multiple trauma patients. The weakness of the ISS scoring system is accurate information on the injured organ has to be known, which is often only obtained when the patient has undergone further investigations such as a CT scan or even during surgery; especially in the abdominal and thoracic organs; so the ISS scoring system is not appropriate when applied in the ED.23
Conclusion
Adjustment to TRISS formula coefficient might be considered. Physiological parameter in RTS that does not include respiratory rate shows reliable prediction which can be used in emergency setting which anatomical diagnostic not yet obtained.
References
- Champion H, Moore L, Vickers R. Injury Severity Scoring and Outcomes Research. In Moore EE, Feliciano DV, Mattox KL. Trauma Eight Edition. McGraw-Hill. 2017;5:71-91.
- Moore L, Hanley JA, Turgeon AF, Lavoie A. Evaluating the performance of trauma centers: hierarchial modeling should be used. J Trauma. 2010;69:1132-1137
CrossRef - Moore L, Lavoie A, LeSage N. Statistical validation of the Revised Trauma Score.
- Asensio J and Trunkey D. Current Therapy of Trauma and Surgical Critical Care. 2016.
- Mahadewa TGB, Golden N, Saputra A, Ryalino C. Modified Revised Trauma-Marshall score as proposed tool in predicting the outcome of moderate and severe traumatic brain injury. Open Access Emergency Medicine. 2018:10;135-139.
CrossRef - Schluter PJ, Nathen A, Neal ML. Trauma and injury severity score (TRISS) coefficients 2009 revision. J Trauma. 2010;68(4):761-770
CrossRef - Butcher NE, Balogh ZJ. Update On The Definition of Polytrauma. Eur J Trauma Emerg Surg. 2014.
CrossRef - Gabbe BJ, Cameron PA, Wolfe R. TRISS: Does It Get Better Than This? Acad Emerg Med. 2004;11(2):181-186.
CrossRef - Kelly AM, Nicholl J, Turner J. Determining The Most Effective Level of TRISS-Derived Probability of Survival for Use As An Audit Filter. Emergency Medicine. 2002;13:146-152
CrossRef - Gunawan B, Dumastoro R, Kamal AF. Trauma and Injury Severity Score in Predicting Mortality of Polytrauma Patients. Research Article. 2017;5(3).
CrossRef - Fernandez CM. Mortality predition using TRISS methodology in the Spanish ICU Trauma Registry (RETRAUCI). Med Intensive. 2016.
- Gorelik M, Godelman S, Elkbuli A, Allen L, Boneva Dm Mckenney M. Can Residents Be Trained and Safety Maintained?. Journal of Surgical Education. Elsevier. 2017.
CrossRef - Chaudrhry N, Naqi SA, Qureshi AU. Effectiveness of TRISS to Evaluate Trauma Care in a Developing Country. Emergency Medicine. 2012.
CrossRef - Gunning AC, Leenen L. Applicability of the predictors of the historical trauma scorein the present Dutch trauma population: Modelling the TRISS predictors. Journal of Trauma and Acute Care Surgery. 2014;77(4):614-619.
CrossRef - Ranti JSR, Sapan HB, Kalesaran LTB. Aplikasi revised trauma score, injury severity score, dan trauma and injury severity score dalam memprediksi mortalitas pada pasien multitrauma di IRDB BLU RSUP Prof. Dr. R. D. Kandou Manado. Jurnal Biomedik (JBM). 2016;8:2:30-35.
CrossRef - Michelle S, Hari R, Bryan C, Dua A, Del Junco D, Wade C. Prehospital triage of trauma patients using the random forest computer algorithm. J Surg Res. 2013;187:371–6.
CrossRef - Alvarez BD, Razente DM, Lacerda DA, Lother NS, Von-Bahten LC, Stahlschimdt CMM. Analysis of the Revised Trauma Score (RTS) in 200 victims of different trauma mechanisms. Rev Col Bras Cir.2016;43(5):334-230
CrossRef - Dinh MM, Bein K, Roncal S, Byrne CM, Petchell J, Brennan J. Redefining the golden hour for severe head injury in an urban setting: the effect of prehospital arrival times on patient outcomes. Injury 2013;44(5):606–1
CrossRef - Tien HC, Jung V, Pinto R, Mainprize T, Scales DC, Rizoli SB. Reducing time-totreatment decreases mortality of trauma patients with acute subdural hematoma. Ann Surg. 2011;253(6):1178–83.
CrossRef - Osterwalder JJ. Can The Golden Hour of Shock Safely be Extended In Blunt Polytrauma Patients? Prospective Cohort Study at a Level I Hospital In Eastern Switzerland. Prehosp Disaster Med. 2002;17(2):75-80.
CrossRef - Ahmed N, Kassavin D, Kuo Y. Can initial systolic blood pressure (SBP) of more than 90 predict hemodynamic stability following torso trauma?. Chest Journal. 2008;134(4):125.
CrossRef - Raux M, Thicope M, Wiel E, Rancurel E, Savary D, David J, Berthier F, Hibon RA, Birgel F, Riou B. Comparison of Respiratory rate and peripheral oxygen saturation to assess severity in trauma patients. Intensive Care Medicine.2006;32(3):405-412.
CrossRef - Bouamra O, Wrotchford A, Hollis S, Vail A, Woodfored M, Lecky F. A new approach to outcome prediction in trauma: a comparison with the TRISS model. J Trauma. 2006;61:701-710
CrossRef - Singh J, Gupta G, Garg R, Gupta A. Evaluation of Trauma and Prediction of Outcome using TRISS Method. J Emerg Trauma Shock. 2011;4(4):446-449.
- Domingues CA, Nogueira LS, Sttervall CHC, Sousa RMC. Performance of Trauma and Injury Severity Score (TRISS) adjustments: an integrative review. Rev Esc Enferm USP. 2015;49:138-146.
CrossRef








