Netravathi Basavaraj Angadi1 , Avinash Kavi2
, Avinash Kavi2 and Shashikant Shankreppa Torgal1
and Shashikant Shankreppa Torgal1
1Department of Pharmacology, Jawaharlal Nehru Medical College, KLE Academy of Higher Education and Research, Belagavi, Karnataka, India.
2Department of Community Medicine, Jawaharlal Nehru Medical College, KLE Academy of Higher Education and Research, Belagavi, Karnataka, India.
Corresponding Author E-mail : dravinashkavi@gmail.com
DOI : https://dx.doi.org/10.13005/bpj/2092
Abstract
Non-communicable diseases (NCDs) are no longer confined to urban and rich persons. They impose a great risk in the low-income nations due to epidemiological and demographic transition. Adherence to medication is key factor in improving the quality of life and preventing complications of NCDs. This study was carried out to study the prevalence of medication adherence and factors determining non-adherence in elderly population with chronic diseases. A community based cross sectional study was conducted with 400 elderly aged 60 years and above. Data was collected by using a pretested questionnaire, which included socio-demographic variables, co-morbidities and details of their medication. Therapeutic adherence was assessed by modified Morisky-Green test, level of cognitive impairment by Pfeiffer’s short portable mental status questionnaire and functional dependence in activities of daily living by Katz Index. Statistical analysis was done using chi-square test. In our study, out of 400 participants, male participants were 184 (48%) and female participants were 216 (52%). 58.5% of them were adherent to their respective treatment medication. Male gender, low level of education, lower socio-economic status and cognitive impairment were the factors associated with therapeutic non-adherence. Therapeutic non-adherence is highly prevalent among elderly persons and is multi-factorial in origin. Interventions to increase adherence among elderly might effective if they are provided with proper guidance and education on the indications of individual treatments, their adverse effects, importance of adherence to medications and various consequences of non-adherence to the therapy.
Keywords
Chronic Diseases; Elderly; Therapeutic Adherence; Urban Area
Download this article as:| Copy the following to cite this article: Angadi N. B, Kavi A, Torgal S. S. Therapeutic Adherence among Elderly with Chronic Diseases Residing in Urban Area of South India – A Descriptive Cross Sectional Study. Biomed Pharmacol J 2020;13(4). |
| Copy the following to cite this URL: Angadi N. B, Kavi A, Torgal S. S. Therapeutic Adherence among Elderly with Chronic Diseases Residing in Urban Area of South India – A Descriptive Cross Sectional Study. Biomed Pharmacol J 2020;13(4). Available from: https://bit.ly/38alIvo |
Introduction
One of the biggest social transformation is population ageing. Geriatric population has doubled since 1980. According to census 2001, elderly population constituted about 77 million, by 2011 it has increased to 96 million and it is expected to rise to 301 million by 2050.1 The core health challenges for elderly are non-communicable diseases (NCDs) such as Cardiovascular disease (CVD), diabetes mellitus (DM), chronic lung disease, hypertension and cancer.1
There is failure to control these morbidities in elderly due to various reasons, of which therapeutic non-adherence constitutes a major burden. Medication compliance could be understood as the degree to which a person’s behaviour and deeds that matches the health and diseases related advice.2 The constant rise in the elderly population combined with extreme surge in number of marketed prescription drugs and compliance to therapeutic regimes has become challenging issue.2 Elderly persons are especially vulnerable to therapeutic non-adherence as they have higher morbidity and mortality which is combined with cognitive and social problems which hinder the correct use of medications.3
Prevalence of therapeutic adherence among elderly ranges from 40-75% in various settings.2 Many factors have been associated with non-adherence; some of which are related to the characteristics of the medications administered, such as adverse effects, cost of drugs, improper instructions and polypharmacy.2 Patient related factors include age, cognitive and sensory disorders, and various other medical conditions.4 It has been shown that reduced compliance to prescribed medication leads to disease progression, in turn leading to deterioration of the symptoms, likely decline in health, the need for additional medical treatment, increased hospitalizations, and most ultimately, death.5
In the present era of clinical practice, promotion of therapeutic adherence is considered as a primary aspect which is often a neglected entity.6 Adherence related aspects should be a part of routine counselling to the patients with chronic illness who are on treatment for long duration and specifically when a treatment regimen appears to be unsuccessful. Various types of medication non-adherence include; failure to have the renewed prescription provided by the physician, lapse of doses, faulty dosage, improper administration of drugs, faulty medication consumption, regularity of medication intake and untimely termination of treatment schedule.7
Therapeutic adherence needs an operational association between a patient, caregiver and physician which helps in proper outlook of medications, i.e. the schedule of administration, proposed benefits, adverse effects and costs. Although non-adherence to medications may be common among the elderly, the key reasons may vary among patients in different scenarios.8 The patient’s demographic characteristics may help to classify elderly patients who are at risk for non-adherence. Insufficient or fringe health literacy among the elderly is also one of the common factors affecting non-adherence which warrants assessment.
The World Health Organization (WHO) report on medication adherence emphasized that interventions for increasing the adherence rate to the treatment may have a superior influence on the health of the people than any specific improvement due to medical interventions.5 Poor treatment adherence is a major barrier to an improved quality of life. Hence a community based study was undertaken out to assess the prevalence of therapeutic adherence and factors determining non-adherence to medications in elderly population with chronic diseases.
Materials and Methods
The present descriptive cross-sectional study was conducted among elderly aged 60 years and above residing in an urban area of Belagavi city, Karnataka state, south India. Study was approved by Institutional Ethical Committee for Human Subjects’ Research of the affiliated Medical College. A written informed consent was obtained from every participant before the study initiation. A pilot study was conducted to validate the assessment form and necessary modification was made to the data collection instrument to suit the local needs.
Sample size was estimated using the formula, N = 4pq/d2 where ‘p’ was considered as 50% of adherence to the medications based on a previous study;3 with a relative error of 10% of ‘p’ and 95% confidence level, the sample size obtained was 400. Sampling frame was prepared using the recent voter’s list and the study participants were carefully chosen using simple random sampling method using computer generated random number table.
Elderly persons (≥ 60 years) who were on treatment for chronic illness which included Hypertension, Diabetes Mellitus, Chronic lung diseases and Coronary artery disease for a minimum period of one year were included in the study. Data was collected by house to house visit using a predesigned, pretested questionnaire, which included socio-demographic variables viz. education and socio-economic status (SES), co-morbidities and details of their medication. The medication details were assessed by prescription by the health professional and by virtually checking the medications. Therapeutic adherence was assessed using modified Morisky-Green test.9 The level of cognitive impairment was assessed using Pfeiffer’s short portable mental status questionnaire10 and functional dependence in activities of daily living was assessed by Katz Index.11
Data was coded and entered on the excel spread sheet. Analysis of the data was performed using Statistical Package for Social Sciences (SPSS), version 20.0. Descriptive statistics for each variable were calculated as percentage. Chi-square test was conducted to examine differences in subject characteristics by adherence level and probability value (P value) of less than 0.05 was considered to be statistically significant.
Results and Discussions
The study included 400 elderly participants with one or more chronic diseases on therapy. Out of which male participants were 184 (48%) and female participants were 216 (52%). Nearly three-fourth of the participants (71%) were in the age group of 60 – 69 years.(Table 1) Significant proportion of participants (44.5%) did not receive any formal education. (Graph 1) Two-third of the participants belonged to class III and IV SES as per the modified BG Prasad classification of SES. (Graph 2)
Table 1: Distribution of the study participants according to the age group (N = 400)
| Age group (in years) | Number | Percentage |
| 60 – 64 | 138 | 34.5 |
| 65 – 69 | 142 | 35.5 |
| 70 – 74 | 70 | 17.5 |
| 75 -79 | 24 | 6.0 |
| ≥ 80 | 26 | 6.5 |
| Total | 400 | 100 |
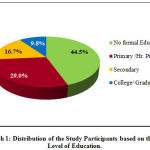 |
Graph 1: Distribution of the Study Participants based on the Level of Education. |
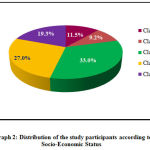 |
Graph 2: Distribution of the study participants according to Socio-Economic Status. |
Among the participants 58.5% (234) of them were adherent to their respective treatment. There was statistical significant difference between men and women with respect to non-adherence to treatment. (Table 2) Noteworthy association was observed between therapeutic adherence and the level of education among participants where those with primary and secondary education level were more adherent to the medications than those with no formal education. (Table 3)
Table 2: Prevalence of therapeutic adherence among different gender (N = 400)
| Gender | Adherent (%) | Non-adherent (%) | Total (%) |
| Men | 82 (44.6) | 102 (55.4) | 184 (100) |
| Women | 152 (70.4) | 64 (29.6) | 216 (100) |
| Total | 234 (58.5) | 166 (41.5) | 400 (100) |
| χ2 = 27.167 Df = 1 P < 0.0001* | |||
Table 3: Association between level of education and therapeutic adherence among study participants (N = 400)
| Educational
Status |
Adherence
(%) |
Non Adherence
(%) |
Total
(%) |
| No formal education | 60 (33.7) | 118 (66.3) | 178 |
| Primary | 96 (82.8) | 20 (17.2) | 116 |
| Secondary | 51 (76.1) | 16 (23.9) | 67 |
| PU College / Degree | 27 (69.2) | 12 (30.8) | 39 |
| Total | 234 (58.5) | 166 (41.5) | 400 (100) |
| χ2 = 83.467 Df = 3 P < 0.0001* | |||
Medication compliance was found to be significantly associated with the SES of participants (P<0.0001). Non-adherence was found to be in a higher proportion among the lowest socio-economic level. (Table 4) Nearly one-fourth of the participants had some degree of cognitive impairment; moderate to severe degree was found to be in <5% of them. (Graph 3) Table 5 describes the association between therapeutic adherence and the cognitive impairment among the study participants which was statistically significant.
Table 4: Association between socio economic status and therapeutic adherence among study participants (N = 400)
| Socio-Economic Status | Adherence
(%) |
Non Adherence (%) | Total
(%) |
| Class I | 35 (76.0) | 11 (24.0) | 46 |
| Class II | 19 (51.4) | 18 (48.6) | 37 |
| Class III | 83 (62.9) | 49 (37.1) | 132 |
| Class IV | 79 (73.1) | 29 (26.9) | 108 |
| Class V | 18 (23.4) | 59 (76.6) | 77 |
| Total | 234 (58.5) | 166 (41.5) | 400 (100) |
| χ2 = 56.251 Df = 4 P < 0.0001* | |||
Table 5: Association Between Cognitive Impairment and Therapeutic Adherence of Study Participants (N = 400)
| Cognition
Status |
Adherence
(%) |
Non Adherence
(%) |
Total (%) |
| Normal | 188 (61.4) | 118 (38.6) | 306 |
| Mild | 40 (54.8) | 33 (45.2) | 73 |
| Moderate | 05 (38.5) | 08 (61.5) | 13 |
| Severe | 01 (12.5) | 07 (87.5) | 8 |
| Total | 234 (58.5) | 166 (41.5) | 400 (100) |
| χ2 =10.704 Df = 3 P = 0.013* | |||
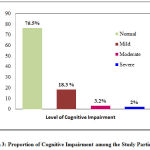 |
Graph 3: Proportion of Cognitive Impairment among the Study Participants. |
The geriatric population is constantly increasing worldwide. This population is vulnerable to many diseases which are chronic in nature and treating elderly is a new challenge of this century of increased life expectancy. Therapeutic non-adherence will bring down the effectiveness of the therapy and is thus a crucial problem in the management of patients with NCDs that require prolonged treatments. Our study assessed the prevalence of therapeutic adherence and factors determining non-adherence to medication in elderly population with chronic diseases. Snowballing the adherence interventions effectively, may have a significantly higher impact of the health of individual and the community which may not be evident with advancement in a specific medical therapeutics.12Adherence is of particular concern in elderly, with many relevant factors associated with lesser adherence, such as multiple co-morbidities and greater complexity of the regimen, which persistently increases with advancing age.13-15
In our study men constituted 52% of the study participants; study by Lemay J, et al had a similar gender proportion.16 Our study showed higher prevalence of therapeutic non-adherence among elderly population i.e., 41.5%. Study conducted by Jüngst C, et al demonstrated a similar rate of non-adherance of 40.9%.17 A study by Awad A, et al revealed a much higher proportion of non-adherence (51%) which was attributed to many social factors.18
Various factors associated with non-adherence to medications were assessed in our study. The gender difference was not only noticeable but also statistically associated in our results. Gender did have an influence on the rate of therapeutic adherence, which showed that women were more compliant than men, which was consistent with other research studies. A study done by Lertmaharit S, et al showed that female patients have better adherence.19 Addition; other study by Senior V, et al could not find a relationship between gender and therapeutic adherence to medication.20
Our results have also demonstrated that therapeutic adherence was significantly influenced by different patient-centered factors like education level, socio-economic status and cognitive level of the participant.
Level of education significantly affected the degree of adherence to medication among the study population. Persons with higher level of education tend to appreciate and understand its significance and thus the degree of adherence increased considerably. A study done by Sweileh W, et al showed that illiterate patients who could not differentiate their medications which increased the risk of errors and non-adherence and it also negatively affect patients’ medical knowledge.21 However a contrary observation was documented by Awad A, et al, where the patients with low to intermediate education levels were more non-adherent compared to those with higher education levels.18 Lemey J, et al showed that the patients were more likely to have negative understanding about their medications if they had lower education level.16
Medication non-adherence was significantly associated with socioeconomic status in our study. A higher proportion of non-adherence was evident among lower and middle income groups which was consistent with studies conducted by Awad A, et al and Bowry AD, et al. 18, 22 These findings could be attributed to the increased medication costs and affordability of medications will be a lower-priority option as compared to other basis needs because of chronic nature of the illnesses. Other possible reasons include prescription of expensive, proprietary medications instead of generic brands and poor health insurance coverage.18
Among the other possible associated factors for non-adherence, we also found that cognitive impairment affected the medication adherence among elderly population with chronic diseases. As the degree of cognitive impairment increases the extent of therapeutic non-adherence escalated significantly. Cognitive processes affect managing the treatment medications.23 In a recent review article, it was observed that older adults with cognitive impairment report lower adherence compared to cognitively intact people.24 Study by Campbell NL, et al suggested that older adults with even mild cognitive impairment have poor therapeutic adherence.25
Non-adherence is highly prevalent among elderly patients and is multi-factorial in nature. There is a need to understand the factors, that are critical in determining the adherence to medications and to develop pertinent strategies to mitigate its impact. Interventions to improve adherence in this population might be most effective if patients are provided with proper education on the indications of distinct therapies, their adverse effects, importance of adherence to medications and various consequences of non-adherence to the therapy especially in elderly with chronic diseases who are on multiple drug therapy for various conditions.
Implications
Our study provides the baseline burden of therapeutic non-adherence among the vulnerable elderly population. Assessment of the factors affecting the adherence and interventions for increasing the adherence to the therapy can be the future focus of research.
Limitation
The adverse outcomes associated with therapeutic non-adherence could not be assessed due to operational constraints.
Conclusion
The prevalence of therapeutic adherence was found to low among elderly urban population. Women were more compliant to medications. Non-adherence to medications was common and was associated with low socio-economic status, lower educational status and cognitive impairment. Enhancement of adherence to the therapy may be achieved through continuing patient education about disease, improvement of patients’ socio-economic levels, reassuring patients to seek medical help regularly; making the drug regimen simpler with reducing the number of drugs intake and use of medication boxes could be helpful.
Acknowledgement
We thank the medical officer and the staff of the Urban Health Centre, Ashok Nagar, Belagavi for their cooperation and support during data collection
Conflict of Interest
The authors report no financial interest or any relationship with any entity that would pose a conflict of interest.
Funding Source
This was a self-funded study.
References
- Irudaya Rajan S. Population ageing and health in India by The Centre for Enquiry into Health and Allied Themes (CEHAT), Mumbai. July 2006. [Accessed from: http://www.cehat.org/cehat/uploads/files/ageing%281%29.pdf last accessed on 12.11.2019]
- Doggrell SA. Adherence to medicines in the older‐aged with chronic conditions: does an intervention concerning adherence by an allied health professional help? Drugs and Aging. 2010; 27(3): 239‐doi: 10.2165/11532870-000000000-00000.
CrossRef - Valladolid C, Madrazo M, Salinero-Fort, Miguel A, Enrique Carrillo, Herranz A et. al. Prevalence of Adherence to Treatment in Homebound Elderly People in Primary Health Care: A Descriptive, Cross-Sectional, Multicentre Study. Drugs & Aging 2010; 27 (8): 641-51.
CrossRef - Salzman C. Medicine compliance in the elderly. Journal of Clinical psychiatry 1995; 56 (1):18-22.
- World Health Organization: Adherence to long term therapies. Evidence for action. Geneva: World Health Organization; 2003. [Available from https://www.who.int/ chp/knowledge/publications/adherence_report/en/ last accessed on 14/12/2019]
- Shams, ME, Barakat EA. Measuring the rate of therapeutic adherence among outpatients with T2DM in Egypt. Saudi Pharm J.2010; 18 (4): 225–32.
CrossRef - Gabr WM, Shams MS. Adherence to medication among outpatient adolescents with epilepsy. Saudi Pharm J. 2015; 23(1) :33-40. doi:10.1016/j.jsps.2014.05.003.
CrossRef - MacLaughlin EJ, Raehl CL, Treadway AK, Sterling TL, Zoller DP, Bond CA. Assessing medication adherence in the elderly: which tools to use in clinical practice? Drugs Aging. 2005; 22(3):231-55.
CrossRef - Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self-reported measure of medication adherence. Med Care 1986; 24(1):67-74.
CrossRef - Pfeiffer E. A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. Journal of American Geriatrics Society. 1975; 23: 433-41.
CrossRef - Katz S, Down TD, Cash HR, Grotz RC. Progress in the development of the index of ADL. Gerontologist. 1970; 10(1): 20-30.
CrossRef - Haynes RB, McDonald H, Garg AX, Montague P. Interventions for helping patients to follow prescriptions for medications. Cochrane Database Syst Rev. 2002; (2): CD000011.
CrossRef - Marengoni A, Angleman S, Melis R, et al. Aging with multimorbidity: A systematic review of the literature. Ageing Res Rev. 2011;10:430‐439.
CrossRef - Kim HA, Shin JY, Kim MH, Park BJ. Prevalence and predictors of polypharmacy among Korean elderly. PLoS ONE. 2014; 9: e98043. doi: 10.1371/journal.pone.0098043.
CrossRef - Blanco-Reina E, Ariza-Zafra G, Ocaña-Riola R, et al. Optimizing elderly pharmacotherapy: Polypharmacy vs. undertreatment. Are these two concepts related? Eur J Clin Pharmacol. 2015; 71: 199‐207.
CrossRef - Lemay J, Waheedi M, Al-Sharqawi S, Bayoud T. Medication adherence in chronic illness: do beliefs about medications play a role? Patient Prefer Adherence. 2018; 12: 1687‐98. [Accessed from: https://doi.org/10.2147/PPA.S169236 last accessed on 23.12.2019] CrossRef
- Jüngst C, Gräber S, Simons S, Wedemeyer H, Lammert F. Medication adherence among patients with chronic diseases: a survey-based study in pharmacies. QJM. 2019 Jul 1; 112(7): 505-12. doi: 10.1093/qjmed/hcz058.
CrossRef - Awad A, Osman N, Altayib S. Medication adherence among cardiac patients in Khartoum State, Sudan: a cross-sectional study. Cardiovasc J Afr. 2017; 28(6): 350‐5. [Accessed from: http://doi:10.5830/CVJA-2017-016 last accessed on 11.11.2019] CrossRef
- Lertmaharit S, Kamol-Ratankul P, Sawert H. Factors associated with compliance among tuberculosis patients in Thailand. J. Med. Assoc. Thai. 2005; 88: 149–56.
- Senior V, Marteau T M, Weinman J. Self-reported adherence to cholesterol-lowering medication in patients with familial hypercholesterolaemia: the role of illness perceptions. Cardiovasc. Drugs Ther. 2004; 18: 475–81.
CrossRef - Sweileh W, Aker O, Hamooz S. Rate of compliance among patients with diabetes mellitus and hypertension. An-Najah Univ. J.2005; 19: 2–11.
- Bowry AD, Shrank WH, Lee JL, Stedman M, Choudhry NK. A systematic review of adherence to cardiovascular medications in resource-limited settings. J Gen Intern Med. 2011;26(12):1479–91. doi: 10.1007/s11606-011-1825-3.
CrossRef - Park HY, Seo SA, Yoo H, Lee K. Medication adherence and beliefs about medication in elderly patients living alone with chronic diseases. Patient Preference and Adherence 2018:12 175–81. doi: 10.2147/PPA.S151263.
CrossRef - Smith D, Lovell J, Weller C, Kennedy B, Winbolt M, Young C, Ibrahim J. A systematic review of medication non-adherence in persons with dementia or cognitive impairment. PLoS One. 2017; 12(2): e0170651. [Accessed from: http://doi:10.1371/journal.pone.0170651 last accessed on 22.01.2020] CrossRef
- Campbell NL, Zhan J, Tu W, et al. Self-reported medication adherence barriers among ambulatory older adults with mild cognitive impairment. Pharmacotherapy. 2016; 36(2): 196–202. [Accessed from: https://doi.org/10.1002/phar.1702 last accessed on 12.02.2020] CrossRef







