Astuti1* , Sri Sutarni2
, Sri Sutarni2  and Ismail Setyopranoto2
and Ismail Setyopranoto2
1Department of Medical and Health Science, Faculty of Medicine, Public Health and Nursing, Universitas GadjahMada, Yogyakarta, Indonesia.
2Department of Neurology, Faculty of Medicine, Public Health and Nursing, Universitas GadjahMada, Yogyakarta, Indonesia.
Corresponding Author Email: dr_astutisps@ugm.ac.id
DOI : https://dx.doi.org/10.13005/bpj/2075
Abstract
Introduction:Due to the high prevalence, disability, and cost incurred by acute ischemic stroke, several parameters to predict the functional outcome of stroke have been developed. Brain-Derived Neurotrophic Factor (BDNF) is a protein that plays an important role in neuroplasticity after a stroke attack. Lower BDNF level was associated with increased risk of developing stroke and poor prognostic functional outcome in stroke patients. Here, we measured serum BDNF levels in the acute and chronic phases of acute ischemic stroke patients to see whether the level was changing and affecting the functional outcome. Methods: A hospital-based prospective cohort study was conducted in the three largest governmental hospitals in Yogyakarta, Indonesia. Acute ischemic stroke patients were consecutively recruited fromJune 2018 until July 2019. Serum BDNF level measurements using enzyme-linked immunosorbent assay (ELISA) and functional outcome assessments using Barthel Index (BI) were performed on the 5th and 30th days after stroke onset, representing the acute and chronic phases of stroke, respectively. Results: Sixty-eight patients completed the study and were categorized into dependent (n=22) and independent (n=46) groups according to BI score on the 30th day after stroke onset. The mean serum BDNF level in the acute phase of the independent group was significantly higher than the dependent group (27,152.28 vs 23,143.41; p=0.044). Similar results were also found in the measurement of serum BDNF levels in the chronic phase in which the mean serum BDNF level of the independent group was found to be significantly higher than the dependent group (27,526.48 vs 22,818.91; p=0.036). There were no significant changes in the measurement of serum BDNF level between the acute and chronic phases in both dependent and independent groups. Conclusions: Serum BDNF level, either in the acute or chronic phase of stroke onset, may predict the functional outcome of the acute ischemic stroke patients.
Keywords
Barthel Index; Brain-Derived Neurotrophic Factor; Functional Outcome; Ischemic Stroke
Download this article as:| Copy the following to cite this article: Astuti A, Sutarni S, Setyopranoto I. Serum Brain-Derived Neurotrophic Factor (BDNF)Level may Predict the Functional Outcome of Acute Ischemic Stroke Patients. Biomed Pharmacol J 2020;13(4). |
| Copy the following to cite this URL: Astuti A, Sutarni S, Setyopranoto I. Serum Brain-Derived Neurotrophic Factor (BDNF)Level may Predict the Functional Outcome of Acute Ischemic Stroke Patients. Biomed Pharmacol J 2020;13(4). Available from: https://bit.ly/3miG75q |
Introduction
Acute ischemic stroke is the most prevalent of all stroke cases and is ranked as the second most common cause of death worldwide. Along with the advancement of medical technology, the number of patients who survive from a stroke attack is increasing. Accordingly, stroke is the primary cause of disabilities in the world.1,2 The Framingham’s study revealed that 26% of stroke patients had a dependency in their daily activities until six months after the attack due to mobility decrease, hemiparesis, and independent walk disability. As a consequence, stroke is also causing financial burdens with the direct yearly costs of hospitalization, rehabilitation, and disability reaching almost US$28.30 million in 2005 in the USA. Apart from that, patients and their families had to pay the indirect social and occupational costs of approximately US$25.60 million.3
Many tools have been developed to assess the functional outcome of stroke patients. These tools include the modified Rankin Scale (mRS), Barthel Index (BI), National Institutes of Health Stroke Scale (NIHSS), Activities of Daily Living (ADL), Instrumental Activities of Daily Living (IADL), and the Gadjah Mada Stroke Scale (SSGM) that assess mostly functional human activities that involve awareness, wakefulness, and muscle strength. Additionally, there are also specific tools to assess cognitive outcome in stroke patients, such as the Mini Mental State Examination (MMSE) and Montreal Cognitive Assessment (MoCA). These tools are widely distributed and daily used for the assessments of stroke patients during hospitalization or during follow-up meetings and consultations.
Considering the high prevalence, disability, and the cost incurred by stroke, biomarker examination was developed to predict the functional outcomes ofstroke patients. Brain-Derived Neurotrophic Factor (BDNF) is a protein that plays an important role in neuroplasticity after a stroke attack. BDNF will induce the migration and mitosis of neural cells to trigger improvement of a patient’s motoric function after stroke.Since the first day of stroke attack,BDNF can already be detected in serum and can be used to predict stroke patients’functional outcome.4,5
Several studies have reported the role of BDNF in stroke. The Framingham’s study indicated that a low level of BDNF is associated with an increased risk ofstroke.5On the other hand, higher BDNF could improve post-stroke depressionwhich indirectly may improve the functional outcome.6Furthermore, studies on BDNF have also been directed to assess the long-term stroke outcome. The study conducted by Hidayat et al. in 2016 showed that the level of BDNF is associated with the outcomes of ischemic stroke patients. Unfortunately, the tools used to assess functional outcomes were not specified.7 However Luo et al. (2019) found that BDNF was statistically yet not clinically significant in its association with patients’ functional outcome measured using the Functional Independence Measure (FIM).4Whether serum BDNF level in the acute phase of stroke may predict the long-term functional outcome of acute ischemic stroke and whether its level changes along with the disease course need to be elucidated.
In this study, we performed the measurements of serum BDNF level and the assessments of functional outcome in patients with the first attack of acute ischemic stroke in the acute and chronic phases of the stroke onset. We used BI as the tool for assessing the functional outcome which allowed the categorization of dependent and independent patients. We aimed to see whether serum BDNF level could predict the functional outcome of acute ischemic stroke patients on the 30th day after the stroke onset.
Material and Methods
Recruitment of Study Participants
This was a hospital-based prospective cohort study conducted in the three largest governmental hospitals in Yogyakarta, Indonesia: Dr. Sardjito General Hospital, Hardjolukito Central Air Force Hospital, and the Academic University Hospital of Universitas Gadjah Mada. We consecutively recruited acute ischemic stroke patients who were admitted to the hospitals from July 2018 to June 2019 with the inclusion criteria as follows: (1) first time acute ischemic stroke attack; (2)the ability to participate in the study until the following month; (3) being cooperative; (4) no history of other organic central nervous system damage such as tumor, trauma, encephalitis, Parkinson’s disease, previous stroke, nor previous physical disability; and (5) willingness to sign the informed consent form. All patients who met the inclusion criteria were included in the study and followed-up until the 30th day of the stroke onset.
On the day of admission, all patients underwent complete clinical, laboratory, and imaging examinations following standard operational procedures and clinical pathways of acute ischemic stroke patients in the three hospitals. The diagnosis of acute ischemic stroke was determined by a neurologist according to the clinical examinations and non-contrast head computerized tomography (CT) scan results. The study was approved by the Medical and Health Research Ethics Committee of the Faculty of Medicine, Public Health and Nursing, Universitas Gadjah Mada(No. KE/FK/0728/EC/2018).
Functional outcome assessments of the acute ischemic stroke patients
Barthel Index (BI) was used as a tool for examining the functional assessment of stroke patients in all three hospitals. BI assessment was performed daily for all the stroke patients from the day of admission until discharge. We collected the BI scores of the patients on the day of admission and on the fifth day after stroke onset during the patient’s hospitalization. Then, on the day of follow-up, on the 30th day after the stroke onset, every patient was assessed again using BI to see their functional outcome. At this time point, the patients were categorized either as dependent or independent according to their BI score. The patients with BI score≥85 were categorized into the independent group while patients with BI score<85 were categorized into the dependent group.8
Serum BDNF Level Measurements
In this study, we measured the serum BDNF level of the patients twice in two separate time points. First, serum BDNF level was measured during the acute phase of ischemic stroke on the 5th day after the stroke onset. Second, serum BDNF level was measured during the chronic phase on the 30th day after stroke onset. The acute phase blood sampling was withdrawn during the patient’s hospitalization and the chronic phase blood sampling was withdrawn on the day of follow-up.
Serum BDNF level was measured using venous blood sample. An amount of 5 ml venous whole blood was collected from the patients between 7:00 to 9:00 am into a serum separator tube. Patient was also advised to avoid oral or enteral feeding for 10 hours prior to blood sampling. The venous whole blood was allowed to clot for 30 minutes in room temperature and then centrifuged at 1,000 x g for 15 minutes at 40C to separate the serum and blood clot within 60 minutes after blood sampling. The serum was collected in a separated tube and stored at -20oC. The serum sample was transferred under frozen condition packed in a heat insulated container filled with dry ice to Prodia Laboratory, Jakarta, Indonesia for further analysis.
Serum BDNF level was measured using enzyme-linked immunosorbent assay (ELISA) Human BDNF Immunoassay Quantikine® (R&D systems, Minneapolis, USA) according to the manufacturer’s instructions. Serum BDNF level (pg/mL) was derived from optical density (OD) values using standard curves. A monoclonal antibody specific for human BDNF was pre-coated onto 96 well polystyrene microplate (BDNF, R&D System) at concentration 1000 pg/mL in a buffered protein base with preservatives to ensure samples were lyophilized. The samples were applied (100µL/well) in duplicate.
Statistical analysis
The data distribution was analyzed using the Shapiro-Wilk test. Numeric data were presented as means value ± standard deviation (SD) or median (minimum-maximum). The mean differences between the two groups were evaluated using unpaired T-test or Mann-Whitney test. Nominal data were presented as proportion and discrepancy between the two groups was analyzed using Chi-squared or Fischer tests. The value was considered significant if p<0.05. All statistical analyses were performed using SPSS version 25 (IBM Corp., New York, USA).
Results and Discussion
Study participants, baseline characteristics, and risk factor analyses
A total of 87 patients with suspected new onset of acute ischemic stroke were recruited on the day of admission to the emergency room or policlinic. Only cooperative patients were assigned to this study. After undergoing initial assessments, including non-contrast head CTscan, all patients who were diagnosed with acute ischemic stroke diagnosis by the neurologist were admitted to the stroke unit or intensive care unit. During the patients’ stay in the hospital, BI score and serum BDNF level in the acute phase were assessed on the 5th day of stroke onset. The next follow-up of the patients was performed on the 30th day after stroke onset. During this time period, 14 patients failed to complete the study. During the follow-up, patients were assessed for their functional outcome using BI and serum BDNF level in the chronic phase. A total of 68 patients were able to complete the study and included in the data analysis. According to the BI score on the follow-up day, the patients were then categorized as dependent (BI score < 85) and independent (BI score > 85). The detailed study design is presented in Figure 1.
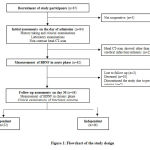 |
Figure 1: Flowchart of the study design |
The baseline characteristics of the study participants are presented in Table 1. Of the 68 patients who were included in the analysis of the study, most of them were geriatric patients and their mean age was 60.97 years old. The male and female proportion was almost equally distributed. All patients were admitted to the hospital within the acute phase of their stroke attack. Their length of stay in the hospital was mainly affected by the severity of their disease as well as comorbidities. Most of the patients were using national health insurance to cover their hospitalization’s claim. On the day of admission, we found that most of the study participants (n=52, 76.5%) had BI score < 85. However, during their treatments in the hospital and after discharge, most of them showed functional outcome improvement so that at the end of the study most of the patients (n=46, 67.64%) were categorized into the independent group (Figure 1).
Table 1: Baseline Characteristics of Study Participants
| Variable | n=68 |
| Age | 60.97 ± 9.75 |
| Sex
a. Male b. Female |
36 (52.90%) 32 (47.10%) |
|
Ethnicity Javanese |
75 (100.00%) |
|
Spouse a. Yes b. No |
58 (85.30%) 10 (14.70%) |
|
Education (years) |
9 (0-22) |
| Occupation
a. Employed b. Unemployed |
39 (57.40%) 29 (42.60%) |
| Onset (hour) | 10.5 (0-129) |
| LOS (day) | 6 (3-11) |
| Health Insurance
a. Yes b. No |
59 (86.8%) 9 (13.2%) |
| Functional outcome on the day of admission
a. Barthel Index < 85 b. Barthel Index > 85 |
52 (76.47%) 16 (23.53%) |
Plus-minus indicates means value ± standard deviation (SD. The range indicates median (minimum-maximum). *The p value is considered statistically significant if p<0.05.
The stroke risk factors, either clinical examinations, comorbidities, or laboratory parameters, that might affect the patients’ functional outcomes were analyzed further (Table 2). We found that most of the analyzed stroke risk factors did not show any significant difference between the dependent and independent groups. We found that serum albumin level on the day of admission was the only laboratory parameter which showed significant difference between the two groups. A significantly lower serum albumin level was found in the dependent group compared to the independent group. This finding is supported by several previous studies that found lower serum albumin level is a predictor for poor clinical and functional outcomes of acute ischemic stroke patients.9,10 Even further, a study also reported that hypoalbuminemia is a frequent laboratory finding in stroke patients and is correlated with the increased stroke severity.11
Table 2: Risk Factor Analysis
| Clinical and Laboratory Parameters | Dependent
(n=22) |
Independent
(n=46) |
p |
| Demographic Characteristics | |||
| Sex
a. Male b. Female |
11 (30.60%) 11 (34.40%) |
25 (69.40%) 21 (65.60%) |
0.74 |
| Spouse
a. Yes b. No |
3 (30.00%) 19 (32.80%) |
7 (70.00%) 39 (67.20%) |
1.00 |
| Age | 61.00 (49.00-84.00) | 59.50 (38.00-81.00) | 0.12 |
| Onset | 12.16 (0.33-85.50) | 9.05 (0.00-129.00) | 0.95 |
| Clinical examinations | |||
| Body Mass Index | 23.61 ± 3.36 | 24.24 ± 3.70 | 0.50 |
| Systolic Blood Pressure | 152.00 (90.00-211.00) | 170.00 (120.00-243.00) | 0.12 |
| Diastolic Blood Pressure | 90.00 (60.00-140.00) | 90.00 (65.00-125.00) | 0.24 |
| Barthel Index on day of admission | 24.09 ± 19.62 | 32.50 ± 80.22 | 0.00* |
| Barthel Index on day-5 onset (acute phase) | 32.50 ± 22.77 | 80.22 ± 19.58 | 0.00* |
| Comorbidities | |||
| Congestive Heart Failure
a. Yes b. No |
3 (42.90%) 19 (31.10%) |
4 (57.10%) 42 (68.90%) |
0.67 |
| Coronary Heart Disease
a. Yes b. No |
0 (0.00%) 22 (33.80%) |
3 (100.00%) 43 (66.20%) |
0.55 |
| Hypertensive
a. Yes b. No |
18 (36.70%) 4 (21.10%) |
31 (63.30%) 15 (78.90%) |
0.22 |
| Hypotensive
a. Yes b. No |
0 (0.00%) 22 (32.80%) |
1 (100.00%) 45 (67.20%) |
1.00 |
| Choric Renal Failure
a. Yes b. No |
1 (100.00%) 21 (31.30%) |
0 (0.00%) 46 (68.70%) |
0.32 |
| Arrythmias
a. Yes b. No |
1 (25.00%) 21 (32.80%) |
3 (75.00%) 43 (67.20%) |
1.00 |
| Atrial Fibrillation
a. Yes b. No |
1 (50.00%) 21 (31.80%) |
1 (50.00%) 45 (68.20%) |
0.55 |
| Chronic Obstructive Pulmonary Disease
a. Yes b. No |
1 (50.00%) 21 (31.80%) |
1 (50.00%) 45 (68.20%) |
0.55 |
| Type II Diabetes
a. Yes b. No |
7 (36.80%) 15 (30.60%) |
12 (63.20%) 34 (69.40%) |
0.62 |
| Dyslipidemia
a. Yes b. No |
5 (20.80%) 17 (38.60%) |
19 (79.20%) 27 (61.40%) |
0.13 |
| Sedentary life style
a. Yes b. No |
14 (35.00%) 8 (28.60%) |
26 (65.00%) 20 (71.40%) |
0.58 |
| Exercise
a. Yes b. No |
2 (13.30%) 20 (37.70%) |
13 (86.70%) 33 (62.30%) |
0.12 |
| Smoking
a. Yes b. No |
8 (38.10%) 14 (29.80%) |
13 (61.90%) 33 (70.20%) |
0.50 |
| Alcohol Consumption
a. Yes b. No |
0 (0%) 22 (32.80%) |
1 (100%) 45 (67.20%) |
1.00 |
| Laboratory Parameters | |||
| Hemoglobin (g/dL) | 13.52 ± 2.54 | 13.45 ± 1.72 | 0.89 |
| Hematocrit | 40.43 ± 7.34 | 39.87 ± 4.95 | 0.71 |
| HbA1C (%) | 6.30 (5.40-13.80) | 6.25 (4.60-18.00) | 0.59 |
| Random blood glucose (mg/dL) | 125.50 (85.00-395.00) | 131.50 (88.00-460.00) | 0.90 |
| Fasting blood glucose (mg/dL) | 109.00 (59.00-318.00) | 94.00 (59.00-277.00) | 0.18 |
| Albumin (g/dL) | 3.79 ± 0.50 | 4.03 ± 0.39 | 0.04* |
| Urea (mg/dL) | 23.20 (9.00-123.80) | 24.05 (8.50-62.00) | 0.79 |
| Creatinine (mg/dL) | 1.03 (0.64-21.78) | 0.92 (0.46-1.88) | 0.42 |
| Cholesterol (mg/dL) | 196.50 (95.00-314.00) | 199.00 (107.00-690.00) | 0.37 |
| Triglycerides (mg/dL) | 105.00 (49.00-291.00) | 147.50 (46.00-1829.00) | 0.09 |
| HDL (mg/dL) | 39.50 (20.00-59.00) | 40.50 (19.00-69.00) | 0.79 |
| LDL (mg/dL) | 138.50 (47.00-237.00) | 142.00 (49.00-353.00) | 0.41 |
| Uric Acid (mg/dL) | 5.19 ± 2.23 | 5.34 ± 1.64 | 0.76 |
| Therapy | |||
| Anti-platelet
a. Yes b. No |
21 (31.30%) 1 (100.00%) |
46 (68.70%) 0 (0%) |
0.32 |
| Statin
a. Yes b. No |
14 (29.20%) 8 (40.00%) |
34 (70.80%) 12 (60.00%) |
0.384 |
| Anti-coagulant
a. Yes b. No |
1 (33.30%) 21 (31.20%) |
2 (66.70%) 44 (67.70%) |
1.00
|
Plus-minus indicates means value ± standard deviation (SD), p value was calculated using Independent T-test. The range indicates median (minimum-maximum), p value was calculated using Mann-Whitney test. *The p value is considered statistically significant if p<0.05.
Other parameters that showed significant difference between the two groups were the mean BI score on the day of admission and on the 5th day of the patients’ stroke onset. In the dependent group, all patients had BI score < 85 on the day of admission, on the 5th day of their stroke onset, and on the 30th day of stroke onset. Although the increase of BI score was observed on every time point assessment, the mean BI score was still below 85 that categorized them into dependent patients (Table 2). On the other hand, the independent groups showed improvement of BI score that allowed the patients to be more independent on the 30th day of stroke onset. The mean value of BI scores on the day of admission and on the 5th day of stroke onset showed that some of the patients that belonged to the independent group had BI score < 85 (Table 2). There were thirty patients whose BI score was < 85 on the day of admission or on the 5th day of stroke onset that finally belonged to the independent group on the 30th day of stroke onset because they reached BI score of > 85. Our findings were supported by previous studies that reported BI score on admission of stroke patients, as well as stroke severity and infarction size on cerebral imaging, may predict the functional outcome one month after the stroke onset.12–14
Serum BDNF level as a predictor of functional outcome in acute ischemic stroke
In this study, serum BDNF level was measured at two different time points: on the 5th day and on the 30th day after stroke onset that representserum BDNF levels in the acute and chronic phases of acute ischemic stroke, respectively. The mean serum BDNF level in the acute phase of the independent group was significantly higher compared to the dependent group. The similar result was also observed in the measurement of serum BDNF level in the chronic phase in which the mean serum BDNF level of the independent group was found to be significantly higher compared to the dependent group (Table 3).
Table 3: Serum BDNF Level in Acute and Chronic Phases.
| Serum BDNF Level
(pg/mL) |
Dependent
(n=22) |
Independent
(n=46) |
p |
| Acute phase (on day-5 after onset) | 23,143.41 ± 8,570.32 | 27,152.28 ± 6,992.04 | 0.044* |
| Chronic phase (on day-30 after onset) | 22,818.91 ± 8,999.79 | 27,526.48 ± 8,211.23 | 0.036* |
Data is displayed as means value ± standard deviation (SD), p value was calculated using unpaired T-test. * The p value is considered statistically significant if p<0.05.
There was no significant difference in the serum BDNF level between the acute and chronic phases of both dependent and independent groups (Figure 2). This finding showed that there was no significant change in the serum BDNF level in the acute and chronic phases of acute ischemic stroke patients, regardless of the stroke severity and functional outcome. In addition, we also found that some patients in the independent groups who had BI score < 85 on the 5th day of stroke onset had a relatively higher serum BDNF level in the acute phase compared to the mean value of serum BDNF level of the dependent group (data not shown). This finding could indicate that higher levels of serum BDNF level may predict a better functional outcome of acute ischemic stroke patients.
 |
Figure 2: Comparison of Acute and Chronic serum BDNF levels between dependent and independent groups.There was no significant difference (p>0.05) in serum BDNF levels between the acute and chronic phases in both the dependent and independent groups. |
Neurotrophic factor is a protein that plays important roles in synaptic processes, growth, myelination, differentiation, and endurance of the neurons. There are three well-known neurotrophic factors that are important for these roles: (1) brain-derived neurotrophic factor (BDNF); (2) nerve growth factor (NGF); and (3) glial cell-derived neurotrophic factor (GDNF). Of the three neurotrophic factors, BDNF is widely studied for its roles in cellular differentiation, neuronal growth and survival, synaptogenesis, cellular migration, neuronal synaptic plasticity, and is involved in the process of neurogenesis.15–17 Furthermore, BDNF is known as the main facilitator of neuroplasticity that plays a role in the rehabilitation process after stroke.18–20BDNF is mainly expressed in the neurons of the central nervous system, but can also be found in the heart, gut, thymus, and spleen. 21,22 BDNF is also secreted by the cerebral endothelial cells (CEC) under the influences of nitrogen oxide (NO) and hypoxia, particularly intermittent hypoxia. This is related to the larger effect of intermittent hypoxia in the incidence of oxidative stress and calcium mobilization.17In blood, most BDNF is stored within platelets.23
Many brain pathologies and psychiatric disorders were reported to reduce the BDNF levels in the patients’ brain and serum.24–26In stroke, angiogenesis and neurogenesis will affect neuron migration, mitosis, and neuroplasticity after ischemic process.In ischemic animal models, neurogenesis will have an effect on the recovery of motoric function after the ischemic process.7,16 After the onset of stroke attack, BDNF contributes in the regeneration and improvement of the neurons with its highest level in the serum could be found on the 30th day of stroke onset. If after 30 days the serum BDNF level remains high, it indicates that the process of neuron regeneration is going well.7 Previous reports that studied experimental animals and stroke patients showed that lower levels of BDNF may lead to poorer functional outcome.7,16,27These reports support our findings that lower levels of serum BDNF in the acute phase were found in the dependent group, and the serum BDNF levels in the chronic phase remained low. In contrast, Figure 2 shows that the independent group hadhigher serum BDNF levelsin the acute phase that remained high until day 30 (chronic phase).This finding might indicate that neuron regeneration in the independent group, whose serum BDNF levels remained high, was much more effective which in turn may improve the functional and clinical outcomes. 7,28
Our findings may indicate that BDNF could be the future potential target of treatment in acute ischemic stroke to improve the patients’ functional outcome. In an animal study, the administration of intracerebral BDNF to mice that underwent internal carotid artery sham operation could improve their functional outcome and reduce the neuro-inflammation process.27 In addition, an animal study using cognitive disorder animal model in stroke (photothrombic-induced prefrontal cortex stroke) showed cognitive improvement after undergoing intracerebral BDNF administration.29
BDNF also serves a function in the neuronal plasticity at the chronic phase duringthe recovery process after an ischemic event. The existence of ischemic lesions increases the endogenous BDNF mRNAexpression and BDNFsecretion which prevent the effects of neuro-inflammation and gliosis as well as increasing axon sprouting.27Accordingly, the stroke outcome is influenced by the expression of BDNF. The functional outcome measured by Fugl-Meyer Assessment (FMA) indicates that the incidence of BDNF genotype polymorphism has effects on the upper extremity motoric function. Acute phase BDNF can predict the medium-long term outcomeforwhich lower levels of BDNFmay serve as a poor prognostic factor.30
Many strategies of medical rehabilitation have been developed to improve the functional outcomes in stroke patients. Aerobic physical exercise can improve the neuroplasticity in stroke patients, through the increase of BDNF secretion, which in turnmay improve the motoric rehabilitation.19,31Besides that, risk factor control and life style intervention are important during the recovery process after stroke attack. In obese children, BDNF level is significantly lower than controls and the lifestyle intervention in obese children significantly increased BDNF and high-density lipoprotein (HDL) levels, and also decreased fasting blood glucose level, insulin, cholesterol, low-density lipoprotein (LDL), and triglyceride levels.32It is expected that early detection and intervention for stroke can reduce the patient’s disability, and thereby reduce the burden and improve the quality of life of the patients and their family.
Conclusions
In this study, we found that higher serum BDNF level in the acute phase of acute ischemic stroke may predict a good functional outcome of stroke patients on the 30th day of stroke onset. On the other hand, lower serum BDNF level in the acute phase of acute ischemic stroke may predict a poor functional outcome of stroke patients on the 30th day of stroke onset. In addition, acute and chronic phases of serum BDNF levels were relatively similar in the dependent and independent groups. This indicates that the measurement of serum BDNF level in the acute phase may reflect its chronic phase. Therefore, measurement of serum BDNF level, either in the acute or chronic phase of stroke onset, may predict the functional outcome of the acute ischemic stroke patients. Our findings may support the development of BDNF as the future potential treatment target in acute ischemic stroke. Further study is needed to be performed in a larger population to validate the cut-off point of lower and higher serum BDNF levels to be used as a predictive biomarker for the functional outcome of acute ischemic stroke patients.
Acknowledgements
The authors are in debt to the patients who were willingly participate in the study. The authors are grateful for the assistance of Kol. Kes. dr. Wahyu Wihartono, M.Kes.,Sp.Sas the neurologist in Hardjolukito Central Air Force Hospital; dr. Farida Niken Astari, M.Sc., Sp. S and dr. Fajar Maskuri, Sp.S, M.Sc as the neurologists in Academic University Hospital of Universitas Gadjah Mada during the study.
Conflict of Interest
There is no conflict of interest from authors sides.
Funding Source
This study was funded by Hibah Dana Masyarakat Program from theFaculty of Medicine, Public Health and Nursing, Universitas Gadjah Mada, Yogyakarta, Indonesia (Number: UPPM/46667/M/05/04/04/18)
References
- Habibi-Koolaee M, Shahmoradi L, Niakan Kalhori SR, Ghannadan H, Younesi E. Prevalence of stroke risk factors and their distribution based on stroke subtypes in Gorgan: a retrospective hospital-based study – 2015-2016. Neurol Res Int. 2018;2018. doi:10.1155/2018/2709654
CrossRef - George MG, Fischer L, Koroshetz W, et al. CDC grand rounds: public health strategies to prevent and treat strokes. Morb Mortal Wkly Rep. 2017;66(18):479-481. doi:10.15585/mmwr.mm6618a5
CrossRef - Ma VY, Chan L, Carruthers KJ. Incidence, prevalence, costs, and impact on disability of common conditions requiring rehabilitation in the united states: Stroke, spinal cord injury, traumatic brain injury, multiple sclerosis, osteoarthritis, rheumatoid arthritis, limb loss, and back pain. Arch Phys Med Rehabil. 2014;95(5):986-995.e1. doi:10.1016/j.apmr.2013.10.032
CrossRef - Luo W, Liu T, Li S, et al. The serum BDNF level offers minimum predictive value for motor function recovery after stroke. Transl Stroke Res. 2019;10(4):342-351. doi:10.1007/s12975-018-0648-5
CrossRef - Pikula A, Beiser AS, Chen TC, et al. Serum BDNF and VEGF levels are associated with risk of stroke and vascular brain injury: Framingham Study Alexandra. Stroke. 2014;44(10):1-16. doi:10.1161/STROKEAHA.113.001447.Serum
CrossRef - Chang WH, Shin MA, Lee A, Kim H, Kim YH. Relationship between serum BDNF levels and depressive mood in subacute stroke patients: A preliminary study. Int J Mol Sci. 2018;19(10). doi:10.3390/ijms19103131
CrossRef - Hidayat A, Arief M, Wijaya A, As’ad S. Vascular Endothelial Growth Factor and Brain-Derived Neurotrophic Factor Levels in Ischemic Stroke Subject. Indones Biomed J. 2016;8(2):115-118. doi:10.18585/inabj.v8i2.206
CrossRef - Schulc E, Pallauf M, Mueller G, Wildbahner T, Them C. Is the Barthel Index an Adequate Assessment Tool for Identifying a Risk Group in Elderly People Living at Home? Int J Nurs Clin Pract. 2015;2(1). doi:10.15344/2394-4978/2015/140
CrossRef - Abubakar S, Sabir A, Ndakotsu M, Imam M, Tasiu M. Low admission serum albumin as prognostic determinant of 30-day case fatality and adverse functional outcome following acute ischemic stroke. Pan Afr Med J. 2013;2. doi:10.11604/pamj.2013.14.53.1941
CrossRef - Manickam S, Franklin J, Petchiappan V, Menon S. A Study of Serum Albumin Levels in Acute Ischemic Stroke and its Correlation with Clinical Outcome. Int J Contemp Med Res IJCMR. 2019;6(3). doi:10.21276/ijcmr.2019.6.3.44
CrossRef - Dziedzic T, Pera J, Slowik A, Gryz-Kurek EA, Szczudlik A. Hypoalbuminemia in acute ischemic stroke patients: frequency and correlates. Eur J Clin Nutr. 2007;61(11):1318-1322. doi:10.1038/sj.ejcn.1602643
CrossRef - Nakibuuka J, Sajatovic M, Nankabirwa J, et al. Early mortality and functional outcome after acute stroke in Uganda: prospective study with 30 day follow-up. SpringerPlus. 2015;4(1):450. doi:10.1186/s40064-015-1252-8
CrossRef - Cioncoloni D, Piu P, Tassi R, et al. Relationship between the modified Rankin Scale and the Barthel Index in the process of functional recovery after stroke. NeuroRehabilitation. 2012;30(4):315-322. doi:10.3233/NRE-2012-0761
CrossRef - Musa KI, Keegan TJ. The change of Barthel Index scores from the time of discharge until 3-month post-discharge among acute stroke patients in Malaysia: A random intercept model. Wang P-N, ed. PLOS ONE. 2018;13(12):e0208594. doi:10.1371/journal.pone.0208594
CrossRef - Greenberg ME, Xu B, Lu B, Hempstead BL. New insights in the biology of BDNF synthesis and release: Implications in CNS function. J Neurosci. 2009;29(41):12764-12767. doi:10.1523/JNEUROSCI.3566-09.2009
CrossRef - Stanne TM, Aberg ND, Nilsson S, et al. Low circulating acute brain-derived neurotrophic factor levels are associated with poor long-term functional outcome after ischemic stroke. Stroke. 2016;47(7):1943-1945. doi:10.1161/STROKEAHA.115.012383
CrossRef - Marie C, Pedard M, Quirié A, et al. Brain-derived neurotrophic factor secreted by the cerebral endothelium: A new actor of brain function? J Cereb Blood Flow Metab. 2018;38(6):935-949. doi:10.1177/0271678X18766772
CrossRef - Calabrese F, Rossetti AC, Racagni G, Gass P, Riva MA, Molteni R. Brain-derived neurotrophic factor: A bridge between inflammation and neuroplasticity. Front Cell Neurosci. 2014;8(DEC):1-7. doi:10.3389/fncel.2014.00430
CrossRef - Mang CS, Campbell KL, Ross CJD, Boyd LA. Promoting Neuroplasticity for Motor Rehabilitation After Stroke: Considering the Effects of Aerobic Exercise and Genetic Variation on Brain-Derived Neurotrophic Factor. Phys Ther. 2013;93(12):1707-1716. doi:10.2522/ptj.20130053
CrossRef - Budni J, Bellettini-Santos T, Mina F, Garcez ML, Zugno AI. The involvement of BDNF, NGF and GDNF in aging and Alzheimer’s disease. Aging Dis. 2015;6(5):331-341. doi:10.14336/AD.2015.0825
CrossRef - Lommatzsch M, Braun A, Mannsfeldt A, et al. Abundant Production of Brain-Derived Neurotrophic Factor by Adult Visceral Epithelia. Am J Pathol. 1999;155(4):1183-1193. doi:10.1016/S0002-9440(10)65221-2
CrossRef - Lommatzsch M, Quarcoo D, Schulte‐Herbrüggen O, et al. Neurotrophins in murine viscera: a dynamic pattern from birth to adulthood. Int J Dev Neurosci. 2005;23(6):495-500. doi:10.1016/j.ijdevneu.2005.05.009
CrossRef - Fujimura H, Altar CA, Chen R, et al. Brain-derived neurotrophic factor is stored in human platelets and released by agonist stimulation. Thromb Haemost. 2002;87(4):728-734. doi: 10.1055/s-0037-1613072
CrossRef - Borba EM, Duarte JA, Bristot G, Scotton E, Camozzato AL, Chaves MLF. Brain-Derived Neurotrophic Factor Serum Levels and Hippocampal Volume in Mild Cognitive Impairment and Dementia due to Alzheimer Disease. Dement Geriatr Cogn Disord Extra. 2016;6(3):559-567. doi:10.1159/000450601
CrossRef - Galvez-Contreras AY, Campos-Ordonez T, Lopez-Virgen V, Gomez-Plascencia J, Ramos-Zuniga R, Gonzalez-Perez O. Growth factors as clinical biomarkers of prognosis and diagnosis in psychiatric disorders. Cytokine Growth Factor Rev. 2016;32:85-96. doi:10.1016/j.cytogfr.2016.08.004
CrossRef - Jiang H, Chen S, Li C, et al. The serum protein levels of the tPA–BDNF pathway are implicated in depression and antidepressant treatment. Transl Psychiatry. 2017;7(4):e1079-e1079. doi:10.1038/tp.2017.43
CrossRef - Ravina K, Briggs DI, Kislal S, et al. Intracerebral delivery of brain-derived neurotrophic factor using hystem®-C hydrogel implants improves functional recovery and reduces neuroinflammation in a rat model of ischemic stroke. Int J Mol Sci. 2018;19(12):1-19. doi:10.3390/ijms19123782
CrossRef - Béjot Y, Mossiat C, Giroud M, Prigent-Tessier A, Marie C. Circulating and brain BDNF levels in stroke rats. relevance to clinical studies. PLoS ONE. 2011;6(12):6-11. doi:10.1371/journal.pone.0029405
CrossRef - Houlton J, Zhou LYY, Barwick D, Gowing EK, Clarkson AN. Stroke induces a BDNF-dependent improvement in cognitive flexibility in aged mice. Neural Plast. 2019;2019. doi:10.1155/2019/1460890
CrossRef - Chang WH, Park E, Lee J, Lee A, Kim YH. Association between Brain-Derived Neurotrophic Factor Genotype and Upper Extremity Motor Outcome after Stroke. Stroke. 2017;48(6):1457-1462. doi:10.1161/STROKEAHA.116.015264
CrossRef - Ergul A, Alhusban A, Fagan SC. Angiogenesis: A Harmonized Target for Recovery after Stroke. Stroke. 2012;43(8):2270-2274. doi:10.1038/jid.2014.371
CrossRef - El-Alameey IR, Ahmed HH, Abushady MM. Role of Lifestyle Intervention Program in RegulatingBrain Derived Neurotrophic Factor in Obese Childrenwith Metabolic Syndrome Components. Biomed Pharmacol J. 2019; 12(3): 1317-1328. doi: 10.13005/bpj/1760
CrossRef







