Rike Syahniar1* , Rayhana1
, Rayhana1 , Dayu Swasti Kharisma1
, Dayu Swasti Kharisma1 , Muhammad Khatami2
, Muhammad Khatami2 and Dimas Bagus Bramasta Duarsa2
and Dimas Bagus Bramasta Duarsa2
1Department of Microbiology and Parasitology, Faculty of Medicine and Health, Universitas Muhammadiyah Jakarta, Indonesia.
2Department of Medicine and Health, Universitas Muhammadiyah Jakarta, Indonesia.
Corresponding Author E-mail: rikesyahniar@gmail.comDOI : https://dx.doi.org/10.13005/bpj/2062
Abstract
BACKGROUND: The high infection of methicillin-resistant Staphylococcus aureus (MRSA) accompanied by increased resistance to many groups of antibiotics is a major concern in the field of infection. This study aims to evaluate the prevalence of MRSA isolates and antimicrobial susceptibility to MRSA isolates in Indonesia. METHODS: We did searches in Pubmed, Proquest, DOAJ, GARUDA, and google scholar for studies published in 2006-2020. Study in Indonesian (Bahasa) and English with the keywords "methicillin-resistant Staphylococcus aureus", "MRSA" and "Indonesia". More than 30 S.aureus isolates derived from human samples were included. RESULTS: A total of 738 articles based on the search results, 13 studies were included in this systematic review. The prevalence of MRSA reported from all studies is 0.3%-52%. The study with the largest prevalence of MRSA was found in Jakarta. The susceptibility of vancomycin antibiotics to MRSA isolates is known to range from 87%-100%. Based on all studies, Linezolid, Tigecycline, Nitrofurantoin, and quinupristin/dalfopristin were reported to have 100% susceptibility. CONCLUSIONS: The prevalence of MRSA is still found high in one of the cities in Indonesia. Surveillance of antibiotic use, monitoring of antimicrobial susceptibility patterns, and antibiotic resistance control programs need to be optimized. MRSA screening is based on a rapid diagnosis when an inpatient admission is also necessary.
Keywords
Indonesia; Methicillin-Resistant Staphylococcus Aureus; Systematic Review
Download this article as:| Copy the following to cite this article: Syahniar R, Rayhana R, Kharisma D. S, Khatami M, Duarsa D. B. B. Methicillin-Resistant Staphylococcus aureus among Clinical Isolates in Indonesia: A Systematic Review. Biomed Pharmacol J 2020;13(4). |
| Copy the following to cite this URL: Syahniar R, Rayhana R, Kharisma D. S, Khatami M, Duarsa D. B. B. Methicillin-Resistant Staphylococcus aureus among Clinical Isolates in Indonesia: A Systematic Review. Biomed Pharmacol J 2020;13(4). Available from: https://bit.ly/3msRnvZ |
Introduction
Methicillin-Resistant S.aureus (MRSA) infections are a tenacious problem in many healthcare settings around the world (1). MRSA infections can range from mild, such as skin infections to bacteremia or sepsis. These infections include endocarditis, pneumonia, osteomyelitis, device-related, cellulitis, and impetigo in health and community care for people(2–4).
In 2017, WHO included S.aureus as a pathogenic bacterium in the list of “high priority” pathogenic bacteria that required a new generation of antibiotics(5). Since the 1960s, the prevalence of MRSA has increased at a dramatic rate and is associated with higher rates of morbidity and mortality(6). MRSA was reported to reach 20% in all regions of the World Health Organization (WHO) and more than 80% in some regions(7). Resistant to methicillin confers resistance to all β-lactamase-resistant penicillins and cephalosporins(8). Vancomycin has been an approved and effective option for treating S. aureus infections, especially MRSA. It has been successfully used worldwide for over 50 years. However, its effectiveness is questioned by the emergence of S. aureus strains that show intermediates to total resistance to this antibiotic(4).Current therapeutic options approved by the Food and Drug Administration (FDA) for MRSA are limited like linezolid, teicoplanin, daptomycin, tedizolid, and streptogramins(9),(10). In contrast, least resistance was observed to vancomycin(9).
A hospital-acquired infection caused by S.aureus is widely reported throughout the world, mainly in Asia(11). The problem of antibiotic resistance in developing countries such as Indonesia, where infectious disease is rampant, is highly pronounced. S. aureus infections cause long hospital stays and increase health care costs(9). S. aureus has gained resistance to most of the antibiotics shown by antimicrobial chemotherapy and once it is resistant, it will be difficult to control and eradicate(9). To control the increase in antimicrobial resistance, it is necessary to collect data about the sensitivity and resistance of each antibiotic. Therefore, this systematic review aims to evaluate the prevalence and antimicrobial susceptibility patterns of MRSA from each study in Indonesia.
Materials and Methods
Search Strategy
This study refers to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) method(12). A search was conducted in April 2020 on PubMed, Proquest, Directoryof Open Access Journal (DOAJ), Garuda (http://garuda.ristekbrin.go.id/),and Google Scholar. We use search terms (“methicillin-resistant Staphylococcus aureus” OR “MRSA”) AND “Indonesia”.We also identified a list of references to search for additional studies.
Study Selection and Eligibility Criteria
All studies reviewed are based on inclusion criteria:(1) Report the prevalence of MRSA; (2) S.aureus isolate samples are human clinical specimens; (3)Publication of articles from January 2006 to March 2020; (4)Articles in English and Indonesian (Bahasa); (5)Isolates amount ≥ 30; (6) The study is an original journal article include cross-sectional, case-control and cohort. Studies that have less than 30 isolate bacteria do not accurately represent resistant bacteria(13). Excluded studies, include: (1)review studies; (2) repetitive isolates; (3) does not explain the number of isolates and sensitivity test methods.
Two authors (RS, R) screened the titles and abstracts of the articles obtained from the initial search. To complete the selected articles, two authors (RS, R) read the full text and were assessed and selected based on inclusion criteria. The disagreement between the two authors was decided by discussion.
Data Extraction and Synthesis
All articles provide the following information: first author, year of publication, study location, study period, data type, sample source, a total of isolates, prevalence of MRSA, and antimicrobial susceptibility results. The data is presented in description and synthesized with a narrative.
Table 1: Summary of studies.
 |
Table 1: Summary of studies |
Results
Selection and Characteristics of Studies.Results
Database search results on Pubmed, Proquest, GARUDA, and DOAJ get 733 articles. Additional articles were identified from Google Scholar and cross-referenced articles were obtained 5 articles. After eliminating duplication, a total of 656 articles are screened for title and abstract. After screening, a total of 43 full-text articles are carried out eligibility assessments. A total of 30 studies were excluded because they did not match with inclusion criteria and duplication of isolates in some studies. The majority of studies are excluded due to the number of S.aureus isolates that do not reach 30. The total articles to be included in 13 studies (Fig. 1).
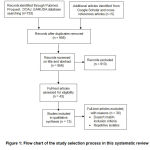 |
Figure 1: Flow chart of the study selection process in this systematic review. |
The most studies for sample collection came from Jakarta(14),(15),(16),(17),(18).One multicenter study collected isolates from Padang, Denpasar, Malang, Semarang(19).Besides, one study collected isolates from 2 cities is Surabaya and Semarang(20).Each of the other studies from Makasar, Pekanbaru, Sanglah, Bandung, Malang, Surabaya, Lampung(14),(21),(22),(23),(24),(25).Five studies are retrospective based on patient medical record data(17,18,21,22,24).A total of 8studies are prospective studies(14),(15),(16),(19),(20),(23),(25)(26).Seven studies used phenotypic sensitivity tests, two using genotypic, and five using both combinations.Based on all phenotypic tests showing that the most used are disk diffusions. MRSA isolates were taken from various clinical samples, including nose, wound, pus, blood, sputum, etc.
Prevalence of MRSA and Antibiotic Susceptibility
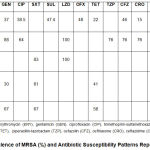 |
Table 2: Prevalence of MRSA (%) and Antibiotic Susceptibility Patterns Reported in Each Study |
The prevalence of MRSA reported from each study was 0.3%-52%. The study with the largest prevalence of MRSA was conducted in Jakarta(17). The lowest prevalence of MRSA was reported in multicenter studies in Surabaya and Semarang(20).Studies with the largest prevalence of MRSA did not perform sensitivity tests on other antibiotics. A total of 5 studies conducted antibiotic sensitivity tests on MRSA isolates (Table 2)(14–16,23). The sensitivity of vancomycin antibiotics to MRSA isolates is known to be 87%-100%(14),(21),(22).Based on all studies, Linezolid, Tigecycline, Nitrofurantoin, and quinupristin/dalfopristin have 100% sensitivity.
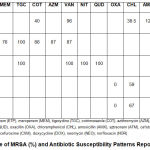 |
Table 3: Prevalence of MRSA (%) and Antibiotic Susceptibility Patterns Reported in Each Study. |
Discussion
Overall, the highest prevalence of MRSA reached 52%. This result was higher than the survey conducted through the SENTRY Antimicrobial Surveillance Program in 1997-2016 involving North America, Europe, Latin America, and the Asia-Pacific region of 40.3%. In the Asia-Pacific region, the SENTRY program reported MRSA amounting to 39.6% (27). In 2017-2018, Indonesia is not included in the Global Antimicrobial Resistance Surveillance System as reported by WHO, so there is no available prevalence of S. aureus resistance(5).
Once the isolate S. aureus is identified as MRSA, it is immediately classified as MDR, because resistance to cefoxitin or oxacillin causes an inability to all categories of antimicrobial β-lactam (i.e. all categories of penicillin, cephalosporins, β-lactamase inhibitors, and carbapenem)(28).MRSA resistance to beta-lactam antibiotics is due to the order of the mecA gene, which is known to produce PB2a transpeptidase thereby lowering the affinity of organisms to bind to beta-lactam antibiotics. S.aureus resistant to penicillin can produce a penicillinase, which can hydrolyze the β-lactam penicillin ring, causing resistance to penicillin(29). Penicillin-resistant S.aureus has long been known since 1942. After being known for penicillin resistance, scientists developed a new semisynthetic penicillin-resistant penicillinase, called Methicillin, which is more resistant to the hydrolysis of β-lactamases (30,31).
The treatment option for MRSA is the Glycopeptide group such as Vancomycin and Teicoplanin, which can only be administered by injection(32). Resistance to vancomycin has been reported since the year 2002(33). The results of this study show vancomycin are still sensitive to S. aureus and can be used in invasive MRSA infections(14),(21,22).Other antibacterial agents to defy MRSA, include quinupristin/dalfopristin, linezolid, daptomycin, and tigecycline(28). In this review, quinupristin/dalfopristin, linezolid, and tigecycline were reported to be 100% sensitive.
The choice of empiric antibiotic for the treatment of MRSA infection depends on the type of disease, the local pattern of S.aureus resistance, drug availability, side effect profile, and individual patient profile. Empiric treatment of uncomplicated skin and soft tissue infections with suspected MRSA infection can be given oral antibiotics such as trimethoprim / sulfamethoxazole, tetracyclines (such as doxycycline or minocycline) and clindamycin (34). There were three studies in this review, tetracycline reported to be less sensitive to MRSA isolate(15,21,26). Excessive empirical antibiotic therapy can also be one of the contributing factors to resistance.
Risk factors in someone infected with MRSA consist of many things. Increased risk with activities or places involving crowding, skin-to-skin contact, and the use of shared equipment. Some people who carry MRSA may continue to having MRSA infection. Intact skin, such as if there are blisters or incisions, is often the location of MRSA infection. Those who have surgery or receive inpatient medical care or have medical devices inserted into their bodies are at a higher risk of developing MRSA infections(35).Over-use and misuse of antibiotics can lead to resistance such as MRSA(36).
Based on all the studies reviewed, the location of the most isolated retrieval and the largest prevalence of MRSA came from Jakarta(15),(16,17),(18),(26). This can be due to major cities such as Jakarta more microbiology examination laboratories with PCR for MRSA detection.Checks using PCR are quite sensitive, so it detects MRSA more.Multicenter research involving many locations including Jakarta and other cities is still needed to see the spread of MRSA in Indonesia.
In Indonesia, many large hospitals, especially vertical hospitals have performed the best standard of microbiology laboratory services following the Guidelines International (latest CLSI) and National (Ministry of Health). Based on PMK 8, 2015 national regulations on Hospitals Anti-Microbial Resistance Control Program (PPRA), antibiograms in hospitals are regularly developed and standardized at least once a year. Antibiograms must be prepared as one of the measurements elements in the ASP (National Standards Program Group) Standard(37). This antibiogram is considered local Empirical Antibiotics guidelines.
Most of these antibiograms are not published, although there are also those in the publication. Also, based on our search for local articles published, some did not meet the inclusion criteria, so we were excluded.There are some limitations to this study such as other systematic reviews, potential publication biases may exist.
Conclusions
MRSA infections are still reported quite high in some studies. Vancomycin, linezolid, and Tigecycline are reportedly still quite sensitive to MRSA isolates. Existing antimicrobial control programs need to be maximized and evaluated in line with the MRSA report found.
Acknowledgements
We would like to thank the LPPM Universitas Muhammadiyah Jakarta and Faculty of Medicine and Health Universitas Muhammadiyah Jakarta for financial support of this work.
Conflict of Interest
All authors declare no conflicts of interest in this paper.
Funding Source
Our study was supported by LPPM UMJ grants with a reference number69/R-UMJ/IV/2020 from Universitas Muhammadiyah Jakarta.
References
- Santosaningsih D, Santoso S, Budayanti NS, Kuntaman K, Lestari ES, Farida H, et al. Epidemiology of Staphylococcus aureus harboring the mecA or Panton-Valentine leukocidin genes in hospitals in Java and Bali, Indonesia. Am J Trop Med Hyg. 2014;90(4):728–34.
CrossRef - Pathare NA, Asogan H, Tejani S, Al Mahruqi G, Al Fakhri S, Zafarulla R PA. Prevalence of methicillin resistant Staphylococcus aureus [MRSA] colonization or carriage among health-care workers. J Infect Public Health. 2016;9(5):571–6.
CrossRef - Oliveira D, Borges A, Simões M. Staphylococcus aureus toxins and their molecular activity in infectious diseases. Toxins (Basel). 2018;10(6).
CrossRef - Abulreesh HH, Organji SR, Osman GEH, Elbanna K, Almalki MHK, Ahmad I. Prevalence of antibiotic resistance and virulence factors encoding genes in clinical Staphylococcus aureus isolates in Saudi Arabia. Clin Epidemiol Glob Heal. 2017;5(4):196–202.
CrossRef - WHO. Global Antimicrobial Resistance Surveillance System (GLASS) Report Early implementation. 2017.
- Zhang S, Sun X, Chang W, Dai Y, Ma X. Systematic review and meta-analysis of the epidemiology of vancomycin-intermediate and heterogeneous vancomycin-intermediate Staphylococcus aureus isolates. PLoS One. 2015;10(8):1–22.
CrossRef - Amann S, Neef K, Kohl S. Antimicrobial resistance (AMR). Eur J Hosp Pharm. 2014;26(3):175–7.
CrossRef - Deyno S, Fekadu S, Astatkie A. Resistance of Staphylococcus aureus to antimicrobial agents in Ethiopia: A meta-analysis. Antimicrob Resist Infect Control. 2017;6(1):1–15.
CrossRef - Gebremariam T, Zelelow Y. A systemic review of antimicrobial resistance pattern of methicillin-resistant Staphylococcus aureus. Saudi J Heal Sci. 2014;3(2):71.
CrossRef - Vanegas Múnera JM, Ocampo Ríos AM, Urrego DM, Jiménez Quiceno JN. In vitro susceptibility of methicillin-resistant Staphylococcus aureus isolates from skin and soft tissue infections to vancomycin, daptomycin, linezolid and tedizolid. Brazilian J Infect Dis. 2017;21(5):493–9.
CrossRef - Chen CJ, Huang YC. New epidemiology of Staphylococcus aureus infection in Asia. Vol. 20, Clinical Microbiology and Infection. Blackwell Publishing Ltd; 2014. p. 605–23.
CrossRef - Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JPA, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6(7).
CrossRef - World Health Organization. Antimicrobial resistance: global report on surveillance. 2014. 2014.
- Santika IKJ, Januartha K, Pinatih P, Nengah N, Fatmawati D. Pola Kepekaan Methicillin-Resistant Staphylococcus aureus terhadap Antibiotika di RSUP Sanglah pada Agustus 2013-Oktober 2013. E-Jurnal Med Udayana. 2014;3(7).
- Safari D, Harimurti K, Khoeri MM, Waslia L, Mudaliana S, A’yun HQ, et al. Staphylococcus aureus and Streptococcus Pneumoniae Prevalence Among Elderly Adults in Jakarta, Indonesia. Southeast Asian J Trop Med Public Health. 2015 May;46(3):465–71.
- Nelwan EJ, Sinto R, Subekti D, Adiwinata R, Waslia L, Loho T, et al. Screening of methicillin-resistant Staphylococcus aureus nasal colonization among elective surgery patients in referral hospital in Indonesia. BMC Res Notes. 2018 Jan;11(1):56.
CrossRef - Lestari DC, Kusumaningrum A, Yasmon A, Karuniawati A, Setting A. Isolates Harboring mecA Genes among Intensive Care Unit Patients from Tertiary Care Hospital in Jakarta , Indonesia. 2017;11(1):23–6.
- Putra MIH, Suwarto S, Loho T, Abdullah M. Faktor Risiko Methicillin Resistant Staphylococcus aureus pada Pasien Infeksi Kulit dan Jaringan Lunak di Ruang Rawat Inap. J Penyakit Dalam Indones. 2014;1(1):3–14.
CrossRef - Santosaningsih D, Santoso S, Budayanti NS, Suata K, Lestari ES, Wahjono H, et al. Characterisation of clinical Staphylococcus aureus isolates harbouring mecA or Panton-Valentine leukocidin genes from four tertiary care hospitals in Indonesia. Trop Med Int Heal. 2016 May 1;21(5):610–8.
CrossRef - Severin JA, Lestari ES, Kuntaman K, Melles DC, Pastink M, Peeters JK, et al. Unusually high prevalence of Panton-Valentine leukocidin genes among methicillin-sensitive Staphylococcus aureus strains carried in the Indonesian population. J Clin Microbiol. 2008 Jun;46(6):1989–95.
CrossRef - Wildana, Sennang N, Rusli B. Methicillin Resistant on Staphylococcus aureus at Hospital Ward. Indones J Clin Pathol Med Lab. 2010;16(3):136–9.
- Anggraini D, Yovi I, Yefri R, Christianto E, Syahputri EZ. Pola Bakteri dan Antibiogram Penyebab Ulkus Diabetikum di RS X Riau Periode 2015 – 2018. Indones J Clin Pathol Med Lab. 2020;12(1):27–35.
- Dahesihdewi A, Mulyono B, Dwiprahasto I, Wimbarti S. Methicillin-Resistant Staphylococcus Aureus Colonization and Screening Method Effectiveness for Patients Admitted To the Intensive Care. Indones J Clin Pathol Med Lab. 2017;24(1):12.
CrossRef - Erikawati D, Santosaningsih D, Santoso S, Dewi K, Laboratorium E, Fakultas M, et al. Tingginya Prevalensi MRSA pada Isolat Klinik Periode 2010- 2014 di RSUD Dr . Saiful Anwar Malang , Indonesia The High Prevalence of MRSA in Clinical Isolates in the period of 2010-2014 in Dr . Saiful Anwar General Hospital Malang , Indonesia. 2016;29(2):149–56.
CrossRef - Setiawan B, Soleha TU RP. Identification of Methicillin-Resistant Staphylococcus aureus (MRSA) in Clinicians and Paramedics in the Perinatology and Obstetric Ginecologic Room of Abdul Moeloek Regional Hospital. J Kedokt Univ Lampung. 2014;3:38–45.
- Suryatenggara AN, Khoeri MM, Waslia L, Tafroji W, Kumalawati J, Subekti D, et al. Identification and Antibiotic Susceptibility of Methicillin-Resistant Staphylococcus aureus Strains Collected at a Referal Hospital, Jakarta, Indonesia in 2013. Southeast Asian J Trop Med Public Health. 2018 Nov;49(6):1053–9.
- Diekema DJ, Pfaller MA, Shortridge D, Zervos M, Jones RN. Open Forum Infectious Diseases Twenty-Year Trends in Antimicrobial Susceptibilities Among Staphylococcus aureus From the SENTRY Antimicrobial Surveillance Program. Open Forum Infect Dis. 2019;6(Suppl 1):S47–53.
CrossRef - Kaur DC, Chate SS. Study of antibiotic resistance pattern in methicillin resistant staphylococcus aureus with special reference to newer antibiotic. J Glob Infect Dis. 2015;7(2):78–84.
CrossRef - Guo Y, Song G, Sun M, Wang J, Wang Y. Prevalence and Therapies of Antibiotic-Resistance in Staphylococcus aureus. Front Cell Infect Microbiol. 2020;10(March):1–11.
CrossRef - Khoshnood, S., Heidary, M., Asadi, A., Soleimani, S., Motahar, M., Savari, M. et al. A review on mechanism of action, resistance, synergism, and clinical implications of mupirocin against Staphylococcus aureus. Biomed Pharmacother. 2019;109:1809–1818.
CrossRef - Rayner, C., and Munckhof WJ. Antibiotics currently used in the treatment of infections caused by Staphylococcus aureus. Intern Med J. 2005;35(Suppl 2.
CrossRef - WHO. Antimicrobial Resistance Global Report on Surveillance. 2014.
- CDC. About Antibiotic Resistance | Antibiotic/Antimicrobial Resistance | CDC [Internet]. 2019 [cited 2020 Jul 16]. Available from: https://www.cdc.gov/drugresistance/about.html
- Siddiqui AH, Koirala J. Methicillin Resistant Staphylococcus Aureus (MRSA). In StatPearls Publishing; 2020.
- CDC. General Information | MRSA | CDC [Internet]. 2019 [cited 2020 Aug 21]. Available from: https://www.cdc.gov/mrsa/community/index.html
- CL V. The antibiotic resistance crisis: part 1: causes and threats. Electrochemistry. 2015;40(4):277–83.
- RI. DJPKKK. Komite Pengendalian Resistensi Antimikroba. Modul Workshop Implementasi PPRA di Rumah Sakit, edisi-3. 2016.








