Vinod Bandela1 , Bharathi Munagapati2, Jayashree Komala3, Ram B Basany3, Santosh R Patil4 and Saraswathi Kanaparthi5
, Bharathi Munagapati2, Jayashree Komala3, Ram B Basany3, Santosh R Patil4 and Saraswathi Kanaparthi5
1Faculty of Dentistry, Pacific Academy of Higher Education and Research University, Udaipur, Rajasthan. India - 313003.
2Department of Prosthodontics and Crown and Bridge, G. Pulla Reddy Dental College and Hospital, Kurnool, Andhra Pradesh. India - 518002.
3Department of Prosthodontics and Crown and Bridge, SVS Institute of Dental Sciences, Mahbubnagar, Telangana. India - 522660.
4Department of Oral Medicine and Radiology, New Horizon Dental College and Research Institute, Bilaspur, Chhattisgarh. India - 495001.
5Department of Pedodontics and Preventive Dentistry, St. Joseph Dental College and Hospital, Eluru, Andhra Pradesh. India - 534004.
Corresponding Author E-mail: vinod.bandela@gmail.com
DOI : https://dx.doi.org/10.13005/bpj/2058
Abstract
To evaluate the better method of implant insertion into the osteotomy site in compromised quality bone for attaining optimal primary stability and thereby achieving the osseointegration for the ultimate success of implant. A total of 32 specimens (wood blocks) simulating D4 bone, were categorized into two groups. The osteotomy site was prepared as per the protocol and implants were placed till the level of the block. The insertion torque was quantified using digital Kratos torque meter. While the implants were inserted and abutments placed by hand ratcheting in the first group; they were motor-driven in the second group. Later pullout test was carried out in universal testing machine and results were analyzed using IBM SPSS Statistics for Windows Software, version 22 (IBM Corp., Armonk, NY, USA). The mean pull out force values obtained in implants placed by hand driven method were 624.375 N while the force values for implants inserted by motor-driven was 692.625 N. There was a statistically significant difference between hand and motor driven implant into the osteotomy site (p<0.05) between the groups. Of the different methods of implant insertion evaluated in this study, motor-driven imply to have a better primary stability indicating better integration with the bone to become a successful implant.
Keywords
Bone Density; Bone Quality; Implant; Implant Success; Insertion Torque; Primary Stability
Download this article as:| Copy the following to cite this article: Bandela V, Munagapati B, Komala J, Basany R. B, Patil S. R, Kanaparthi S. Evaluating the Primary Stability of Implants by Two Different Insertion Methods in Compromised Bone – A Pilot Study. Biomed Pharmacol J 2020;13(4). |
| Copy the following to cite this URL: Bandela V, Munagapati B, Komala J, Basany R. B, Patil S. R, Kanaparthi S. Evaluating the Primary Stability of Implants by Two Different Insertion Methods in Compromised Bone – A Pilot Study. Biomed Pharmacol J 2020;13(4). Available from: https://bit.ly/34W4Ren |
Introduction
Dental implants have become a viable treatment option for restoring missing tooth/teeth. The purpose of tooth replacement with implants is to restore adequate function and esthetics without affecting adjacent hard and/or soft tissue structures. The successful outcome of any implant procedure depends on a series of patient-related and procedure-dependent parameters; general health condition, biocompatibility of the material used, implant surface characteristics, surgical procedure performed and the quality and quantity of the implant site.[1]
Treatment should be based on accurate information; understanding patient’s problems, and acknowledging suitable treatment alternatives, but not simply on the hopes of dentist and patient. Implant stability is defined as the absence of positive clinical mobility. Implant instability could result in fibrous encapsulation with resultant failure. Primary implant stability is a mechanical phenomenon that is related to the technique followed, the type of implant used and the quality and quantity of bone available in the region of implant placement. Secondary implant stability is the increase in stability attributable to bone formation and remodeling at the implant/tissue interface and the surrounding bone.[2-4]
Factors affecting implant stability can be categorized into those a) influencing primary stability and b) influencing secondary stability as in the figure-1.[5] Primary stability of an implant is a result of initial interlocking between the body of implant and alveolar bone, which later-on affects the secondary stability.[6,7] For immediate or early loading; primary stability is the key prerequisite.[8,9]
 |
Figure 1: Factors affecting implant stability |
There are many ways by which the implant stability can be evaluated. The gold standard in evaluating the degree of osseointegration is either microscopically or histologic analysis. Due to the invasiveness of these procedures, other methods have been proposed such as the use of radiographs, reverse torque analysis, cutting torque resistance, periotest, resonance frequency analysis (RFA) and checking for mobility clinically.[10]
Surgical driven motors play an important role in the placement of implants. These handpieces can better stabilize the orientation and maintain a constant drilling speed.[11] However, motor-driven instruments are expensive. So, manual insertion of implant into the osteotomy site is the viable alternative option.
Objectives
To evaluate the primary stability of implants inserted by manual method.
To evaluate the primary stability of implants inserted by motor-driven method.
To compare the primary stability of implants placed by manual and motor insertion methods.
Materials and Methods
The entire study was done at Indian Institute of Chemical Technology (IICT), under the Council of Scientific and Industrial Research (CSIR); Hyderabad. Two different implant insertion techniques; manual insertion and motor driven were used in the current study to evaluate the primary stability. Soft wood blocks simulating D4 bone were selected as it has similar mechanical properties to the human bone and for the ease of standardizing the samples.[12] Wood was used as a substrate for the placement of implants and the type of wood used was from Pinus densiflora and the samples were collected from the stem portion of the tree (single wood block) from high-grade lumber.[13] The samples were stored below 19 percent moisture content and care was taken not to exceed excessive moisture with relative humidity about 78 percent and temperature between 32oC – 35oC by storing in the boxes. Whole experiment was done in particular seasoned wood in order to minimize the effects of temperature, moisture and relative humidity.[14]
Quality of the wood was based on the suggestion of local timber depots and tactile sensitivity of the experienced implantologists. The block dimensions were 40X14X40mm length, width and height respectively, to accommodate the holding plates of the universal testing machine (Dak Series 7200, Mumbai, India). A total of 32 specimens were divided into two study groups (n=16). Sample size estimation was done by using GPower software (version 3.0). A minimum total sample size of 32 (16 in each group) was found to be sufficient for an alpha value of 0.05. Touareg™ S Implant (Adin-Israel) was used for performing the study. The dimensions of the implant were 10X4.2mm in length and diameter with internal hex implant-abutment connection. After placing and adjusting the sample over the cast holder, osteotomy was done with the aid of a dental parallelometer (Iso A1, Artiglio, Italy) (fig.2). The preparation of osteotomy site was done initially using pilot drill followed by sequential drills upto a depth of 10mm and 3.2 mm wide. In first group of samples, the implant was hand-tightened using a ratchet and in second group, the implant was placed with a low speed motor driven hand piece of 20rpm, such that the implant platform merges with the level of the wood in both groups. An abutment was hand screwed in group-1 while it was motor driven in group-2. Insertion torque analysis was quantified by using digital torquimeter Kratos (Kratos Industrial Equipment Inc., Cotia, SP, Brazil) coupled to implants mount. To verify the pullout strength, the implant mounts were coupled to a piece adapted to a load cell of 200kg of aforementioned universal testing machine. The test was performed using an axial traction force of 10mm/min at a load of 200 kg in the direction of the long axis of the implant (fig.3). Data was analyzed using IBM SPSS Statistics for Windows Software, version 22 (IBM Corp., Armonk, NY, USA). One-way analysis of variance (One-way ANOVA) and independent t test was performed for intergroup comparison, the p values less than 0.05 were statistically significant.
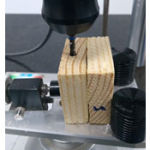 |
Figure 2: Osteotomy preparation with parallelometer |
 |
Figure 3: Pull-out test with Instron machine |
Results
A total of 32 specimens were tested, in the first group where the implants were hand driven, a mean value of 624.375 N with a standard deviation (SD) of 72.0832. In the second group implants placed with help of motor, a mean of 692.625 N with SD of 59.9265 (table-1). There was a statistically significant difference between hand and motor driven implant into the osteotomy site (p<0.007) between the groups (table-1 and fig.4).
Table 1: Comparison of implant stability values between two groups
| Implant
placement |
n | Mean | SD | SD Error
Mean |
Mean
Difference |
t-value | p value |
| (Group-1)
Hand driven |
16 | 624.375 | 72.0832 | 18.0208 | -68.25 | -2.91 | 0.007* |
| (Group-2)
Motor driven |
16 | 692.625 | 59.9265 | 14.9816 |
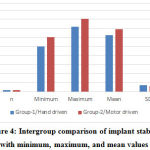 |
Figure 4: Intergroup comparison of implant stability with minimum, maximum, and mean values. |
Discussion
Brånemark’s historical discovery of titanium osseointegration to the bone, made rehabilitation of edentulous patients possible using machined screws enabling the attachment for a fixed prosthesis.[15] Since then, endosseous dental implants of various shapes, sizes and surface textures have been used in partially and completely edentulous patients, achieving a greater success rate of 96.7%.[16]
Lekholm and Zarb listed four different bone qualities in different regions of the jaw bone; where bone quality 4 has a thin cortical bone with low density trabecular core. Hence, clinician needs a greater concern during implant procedures in such locations. Misch described these four bone density groups in all the regions of jaw and found D4 bone (the low density bone) in the posterior maxilla.[13,17,18]
In the present study, the osteotomy site was under-prepared than the actual size of the proposed implant dimensions since the quality of bone selected was D4. In a study by Su-jin Ahn et al., concluded that in a compromised situation like posterior maxilla under-preparation and bi-cortical fixation of the implant increased the stability.[18]
Present study was performed to evaluate the primary stability of implant. There are many factors which influence the success of an implant, primary stability being the key factor. Fawad and George in a literature review emphasized on the implant stability and the factors governing its clinical success in particular: adequate bone volume and bone density, implant dimensions, surgical procedure performed, and initial torque acquired are important.[19]
In the present study, 20 rpm was used to place the implant onto the osteotomy site, which was in accordance with the recommended use of low speed (less than 30 rpm) hand piece for implant installation by Misch.[17]
In this study, pullout test was performed and wood was used to simulate bone. Assessing the implant stability can be categorized as invasive/destructive methods and non-invasive/non-destructive methods. Invasive methods can be; histologic/ histomorphologic analysis, tension test, pull-out test and removal torque analysis. In direct method, a specified force is necessary to remove the implant from its bed.[20]
Brunski et al., concluded that pull-out test not only investigates the healing capabilities, but also measures the interfacial shear strength by applying load parallel to the implant-bone interface.[21] Though reverse torque test can be used, it would be beneficial during second stage surgery and also, it is one of the method in removing the undesirable placed or angulated implants.[22]
In the present study, one of the commonest method of the implant insertion – manual method; which most of the early practitioners used for threading the implant as it offers a better tactile sensation of the path compared to a hand piece was carried out. Dorjpalam et al., in his study concluded that primary stability not only depend on the insertion torque but also on the quality of the bone.[23]
Pullout test was used in the present study to compare the primary stability of implants placed by different insertion methods. Surveyor was used to prepare osteotomies of similar dimensions. While the mean pull-out force values obtained by hand-driven method were 624.375 N, it was 692.625 N for implants placed by motor-driven (table-1). The results were statistically significant (p<0.05) between the groups, motor-driven technique showed increased stability as compared to that of hand-driven implants. Results of our study were in accordance with the study of Oliscovicz et al., where stability of the implants inserted in different substrates were evaluated. [24] A study by Jung SK et al., on the success rate of orthodontic mini-screws concluded that the motor-driven method has a higher rate of success.[11]
Such difference between the methods could be due to the precise placement of motor-driven implants in contrary to hand-driven implants where there may be widening of the osteotomy due to the lateral component of force being applied while threading the implant with a hand ratchet, decreasing the stability of implants. However, a study by Novsak et al., on the effect of insertion method on the primary stability of orthodontic mini implants by machine versus manual method, concluded that manual insertion method as the better way of attaining primary stability.[25]
Conclusion
Within the limitations, it can be concluded that: motor-driven implants offered significantly greater implant stability as compared to those inserted by manual method. However, we suggest that a larger in-vivo study with a greater sample size could be carried out to confirm the findings of this study and shed more light on implant stability.
Acknowledgments
I would like to thank Dr. D.B Rohini Kumar, Sr. technician–IICT, Hyderabad. India for helping me to carry out this study.
Conflicts of Interest
None
Funding Source
The study is self-funded
References
- Turkyilmaz I, Tumer C, Ozbek EN, Tözüm TF. Relations between the bone density values from computerized tomography, and implant stability parameters: a clinical study of 230 regular platform implants. J Periodontol.2007;34(8):716-22.
CrossRef - Meredith N. Assessment of implant stability as a prognostic determinant. Int J Prosthodont. 1998;11(5):491-501.
- Brunski JB. Biomechanical factors affecting the bone-dental implant interface. Clin Mater. 1992;10(3):153-201.
CrossRef - Nedir R, Bischof M, Szmukler-Moncler S, Bernard JP, Samson J. Predicting osseointegration by means of implant primary stability. Clin Oral Implants Res. 2004;15(5):520-8.
CrossRef - Javed F, Ahmed HB, Crespi R, Romanos GE. Role of primary stability for successful osseointegration of dental implants: Factors of influence and evaluation. Interv Med Appl Sci. 2013;5(4):162–7.
CrossRef - Berglundh T, Abrahamsson I, Lang NP, Lindhe J. De novo alveolar bone formation adjacent to endosseous implants. Clin Oral Implants Res. 2003;14(3):251-62.
CrossRef - Esposito M, Grusovin MG, Maghaireh H, Worthington HV. Interventions for replacing missing teeth: different times for loading dental implants. Cochrane Database Syst Rev. 2013(3).
CrossRef - Kim SK, Lee HN, Choi YC, Heo SJ, Lee CW, Choie MK. Effects of anodized oxidation or turned implants on bone healing after using conventional drilling or trabecular compaction technique: histomorphometric analysis and RFA. Clin Oral Implants Res. 2006;17(6):644-50.
CrossRef - Roccuzzo M, Aglietta M, Cordaro L. Implant loading protocols for partially edentulous maxillary posterior sites. Int J Oral Maxillofac Implants. 2009;24:147-57.
- Mistry G, Shetty O, Shetty S, Singh RD. Measuring implant stability: A review of different Methods. J Dent Implant. 2014;4(2):165-9.
CrossRef - Kim JS, Choi SH, Cha SK, Kim JH, Lee HJ, Yeom SS, Hwang CJ. Comparison of success rates of orthodontic mini-screws by the insertion method. Korean J Orthod. 2012;42(5):242-8.
CrossRef - Ayse Gulsahi (2011). Bone Quality Assessment for Dental Implants, Implant Dentistry – The Most Promising Discipline of Dentistry, Prof. Ilser Turkyilmaz (Ed.), ISBN: 978-953-307-481-8, InTech, Available from: http://www.intechopen.com/books/implant-dentistry-the-most-promising discipline-of-dentistry/bone-qualityassessment-for-dental-implants.
CrossRef - Lekholm U, Zarb GA, Albrektsson T. Patient selection and preparation. Tissue integrated prostheses. Chicago: Quintessence Publishing Co. Inc., 1985;199-209.
- Rietz RC. Storage of lumber. Forest Products Laboratory, Forest Service, US Department of Agriculture; 1978.
- Branemark PI, Breine U, Adell R, Hansson BO, Lindstrom J, Ohlsson A. Intra-osseous anchorage of dental prostheses: I. Experimental studies. Scand J Plast Reconstr Surg. Suppl 1969; 3(2):81-100.
CrossRef - Buser D, Mericske-Stern R, Pierre Bernard JP, Behneke A, Behneke N, Hirt HP, Belser UC, Lang NP. Long-term evaluation of non-submerged ITI implants. Part 1: 8-year life table analysis of a prospective multi-center study with 2359 implants. Clin Oral Implants Res. 1997;8(3):161-72.
CrossRef - Misch CE: Bone density: a key determinant for treatment planning. Contemporary Implant Dentistry. 3rd Missouri: Elsevier;2008.130-46.
- Ahn SJ, Leesungbok R, Lee SW, Heo YK, Kang KL. Differences in implant stability associated with various methods of preparation of the implant bed: An in-vitro study. J Prosthet Dent. 2012;107(6):366-72.
CrossRef - Javed F, Romanos GE. The role of primary stability for successful immediate loading of dental implants. A literature review. J Dent. 2010;38(8):612-20.
CrossRef - Nonhoff J, Moest T, Schmitt CM, Weisel T, Bauer S, Schlegel KA. Establishment of a new pull-out strength testing method to quantify early osseointegration-An experimental pilot study. J Cranio Maxill Surg. 2015;43(10):1966-73.
CrossRef - Brunski JB, Puleo DA, Nanci A. Biomaterials and biomechanics of oral and maxillofacial implants: Current status and future developments. Int J Oral Maxillofac Implants. 2000;15(1):15-46.
- Jividen Jr G, Misch CE. Reverse torque testing and early loading failures: help or hindrance? J Oral Implantol. 2000;26(2):82-90.
CrossRef - Bayarchimeg D, Namgoong H, Kim BK, Kim MD, Kim S, Kim TI, Seol YJ, Lee YM, Ku Y,Rhyu IC, Lee EH. Evaluation of the correlation between insertion torque and primary stability of dental implants using a block bone test. J Periodontal Implant Sci. 2013;43(1):30-6.
CrossRef - Oliscovicz NF, Shimano AC, Marcantonio Junior E, Lepri CP, Dos Reis AC. Analysis of primary stability of dental implants inserted in different substrates using the pullout test and insertion torque. Int J Dent. 2013;2013.
CrossRef - Novsak D, Trinajstic Zrinski M, Spalj S. Machine-driven versus manual insertion mode: influence on primary stability of orthodontic mini-implants. Implant Dent. 2015;24(1):31-6.
CrossRef








