Vyshma Kizhuppully Viswambaran, Anavadhya K. A, Gopika Chandrababu, Amritha Babu, Gayathri Rajeev and Swati Gupta*
Amrita School of Pharmacy, Amrita Institute of Medical Sciences, Amrita Vishwa Vidyapeetham, AIMS-Ponekkara PO, Kochi, Kerala -682041, India.
Corresponding Author E-mail: swatigupta@aims.amrita.edu
DOI : https://dx.doi.org//10.13005/bpj/2072
Abstract
Blepharitis is an eyelid disorder characterized by inflammation and pain. It affects all the ages and ethnic groups. Primary cause of blepharitis is poor hygienic condition. Topical antibiotics are the preferred first line therapeutic agents along with eyelid cleansing and warm compresses are recommended. Topical steroids, oral antibiotics and calcineurin inhibitors are also recommended in severe conditions. However, recurrence of disease, dose related side effects and safety regimen are still uncertain with these agents. Blepharitis needs a long term treatment, thus novel formulations and products with natural components may be considered more reliable to overcome such issues. In this review article we have discussed human clinical trials (HCTs) conducted with conventional synthetic drugs, novel drug delivery systems developed with synthetic drugs and drugs of natural origin and other supportive measures. As compared to synthetic drugs, formulations with natural origin were found to be safe with minimum side effects.
Keywords
Blepharitis; Clinical Trials; Natural Drugs; Novel Drug Delivery Systems; Synthetic Drugs
Download this article as:| Copy the following to cite this article: Viswambaran V. K, Anavadhy K. A, Chandrababu G, Babu A, Rajeev G, Gupta S. Blepharitis: A Review on Human Clinical Trials with Synthetic and Natural Remedies.Biomed Pharmacol J 2020;13(4). |
| Copy the following to cite this URL: Viswambaran V. K, Anavadhy K. A, Chandrababu G, Babu A, Rajeev G, Gupta S. Blepharitis: A Review on Human Clinical Trials with Synthetic and Natural Remedies.Biomed Pharmacol J 2020;13(4). Available from: https://bit.ly/3gFOZAR |
Introduction
Blepharitis is an inflammatory disorder of eyelids affecting all the age and ethnic groups probably because of poor hygienic condition. To find the prevalence of blepharitis, a lot of surveys have been conducted among school going children in India (Table 1) 1, 2-7. Blepharitis is common among different ocular morbidity and prevailing unhygienic conditions. Apart from poor hygienic conditions microbial infection, clogged meibomian gland, dandruff, eyelash mite and allergy are some of the major causes of this disease 8. Blepharitis mainly starts with poor hygiene, allergy or meibomian gland dysfunctioning followed by blockage of meibomian gland and decreased production of meibom 8-10. Different causes of blepharitis have been summarized as schematic representation in the figure 1.
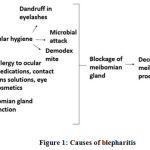 |
Figure 1: Causes of blepharitis |
Table 1: Blepharitis survey reports of different places in India
| Area of survey
|
No of subjects included in survey & their age range
|
Percentage of population affected
|
Reference
|
|
Eastern India |
633 (6-17yrs) |
5.05% |
[2] |
|
Assam |
208 (6-15 yrs) |
2.38% |
[3] |
|
Thiruvananthapuram, Kerala |
3130 (9-15 yrs) |
0.3% |
[4] |
|
Ernakulam, Kerala |
1100 (8-12 yrs) |
3.81% |
[5] |
|
Kolar, South India |
2680 (6-16 yrs) |
3.64% |
[6] |
|
Uttar Pradesh |
110 (3-12 yrs) |
15.45% |
[7] |
Classification and diagnosis
Based upon anatomic location, blepharitis classified as anterior, posterior and mixed type blepharitis. In anterior blepharitis, Inflammation occurs on the base of eyelashes and follicles and it is characterized by redness in lid margin, superficial discomfort, eyelid ulceration, crusting around lashes, blurred vision, light sensitivity, stickiness of eyelidsin morningetc 1, 8. In posterior blepharitis meibomian gland dysfunctioning happens and it is characterized by decreased meibom secretions with foamy tears, chalazia, eyelid scarring, corneal scarring, corneal neovascularization, corneal ulceration, marginal infiltration and pannus. Red swollen eyelids, burning sensations, ocular irritation, loss of eyelashes and misdirected eyelashes are common symptoms of Blepharitis 1, 8. Techniques used to diagnose blepharitis are slit lamp examination and tear film stability test by using manual keratometry, placidokeratometry precorneal tear film interferometry 1. Confocal microscopy is the modern technique to diagnose presence of inflammatory cells 10, 11.
Treatment and management
Blepharitis is a common recalcitrant condition; complete recovery from this condition is not possible. The synthetic methods for treatment are not adequate 12. Topical antibiotics and warm compress is as a first line therapy. Among different antibiotics, macrolides are preferred in the treatment of blepharitis, becausealong with antibacterial effect it reduces inflammation as well 13. Long term therapy creates resistance 14. Topical steroids are using in chronic conditions of blepharitis to reduce inflammation, but it can use for less duration due to its complications like increased intraocular pressure 15. Oral antibiotics are preferred in chronic conditions 16. Calcineurin inhibitors are immunomodulatory agents given as topical, which also reduces the inflammation 1, 8, 9. They creates side effects like mild and transient ocular irritation and burning sensation 17, 18. Omega 3 fatty acids are the supportive therapy in blepharitis to improve functioning of meibomian glands 19, 20. Eyelid cleansing, warm compress and eyelid scrub are preferred to reduce some complications by removing the meibom clogging and removes microbes 12, 21. A detailed account on HCTs with synthetic drugs has been presented in the Table 2 22-30.
Table 2: Synthetic drugs used for the management of blepharitis
|
Drug Class, Dosage form & ophthalmic application |
Dosage |
Duration of Treatment |
Side effects |
Reference |
|
Azithromycin 1% & 1.5% (Antibiotic solution) |
1 drop, Twice daily/1 drop, Once daily |
2 days/12 days |
Eye irritation, blurred vision, dry eyes, stuffy nose. |
[10] |
|
Erythromycin (Antibiotic ointment) |
1 drop, Twice daily |
2-8 weeks |
Stinging, burning, temporary blurred vision, redness. |
[9] |
|
Norfloxacin 0.3% (Antibiotic solution) |
2 drops, every 2 hours/2 drops, 4 times daily |
1 day/6 days
|
Eyelid itching, swelling or crusting, tearing, bad taste in mouth, light sensitivity. |
[22] |
|
Tobramycin 0.3% & Dexamethasone 0.1% (Antibiotic & Steroids suspension) |
1 drop, every 12 hours |
12 weeks |
Redness, discomfort, light sensitivity, blurred vision. |
[10] |
|
Tobramycin 0.3% & loteprednol 0.5% (Antibiotic & Steroids suspension) |
1 drop, 4 times, daily |
14 days |
Increased IOP, lacrimation disorders, photophobia, corneal deposits. |
[10] |
|
Moxifloxacin 0.5% & Dexamethasone 0.1% (Antibiotic & Steroids suspension) |
1 drop, 4 times, daily |
7 days |
Watery eyes, pain, redness, itchiness. |
[10] |
|
Doxycycline 100mg (Antibiotic Capsules/Tablet) |
Twice daily |
8 weeks |
Loss of appetite, nausea, vomiting, diarrhoea, sensitivity to sun, adult teeth discolouration, headache. |
[23, 24] |
|
Doxycycline 300mg (Antibiotic Capsules/Tablet) |
Once daily |
3 weeks | Loss of appetite, vomiting, diarrhoea, sensitivity to sun, hives, adult teeth discolouration, headache. |
[25] |
|
Minocycline 50mg (Antibiotic Capsules) |
Twice daily |
2 months |
Stomach upset, dizziness, unsteadiness, drowsiness, swollen tongue, mouth sores. |
[26] |
| Itraconazole 200mg
(Antifungal agent Capsules) |
Once daily |
7 days |
Stomach upset, headache, unpleasant taste, skin rashes, joint/ muscle pain. |
[27] |
|
Cyclosporine 0.05% (Calcineurin inhibitors emulsion) |
1 drop, every 12 hour | 12 weeks |
Discharge, tearing, visual blurring, redness. |
[28] |
|
Tacrolimus 0.03% (Calcineurin inhibitors Ophthalmic ointment) |
Twice daily, applying in eyelid margin |
28 days |
Soreness, eye discomfort, eyelid itching. |
[29, 30] |
In past few decades some review articles published on treatment and management of blepharitis. Christopher (2016) and Katherine et al. (2015) discussed about synthetic drugs used for blepharitis, but didn’t include any treatment using natural products 1, 8. Stephen et al. (2014) discussed about human clinical trials (HCTs) conducted with synthetic formulations for treatment of blepharitis, they also didn’t include any HCTs for drugs from natural origin10. In this review we have summarized the HCTs with synthetic drugs in conventional dosage forms, synthetic drugs in novel drug delivery systems and formulations from natural origin for the management of blepharitis (Table 3).
Table 3: Human clinical trials with novel drug delivery systems and formulations of natural origin in treatment of blepharitis.
|
Formulation/ Method |
Type of trial, Preferred dosage and duration of therapy |
Major findings |
Side effects |
Reference
|
|
Azasite® (Azithromycin 1% ophthalmic solution in durasite) |
Randomised, prospective placebo controlled study in 10 patients. 1-2 drops Once daily for One month |
Effective for anterior and posterior blepharitis. Improves drug bioavailability, tissue penetration, sustained delivery |
Foreign body sensation, stinging, sticky eye sensation |
[13] |
|
0.25% Povidone iodine and DMSO gel |
Retrospective chart review, 17 patients.Twice daily applying in eyelid margin, One week |
Effective in treatment of blepharoconjunctivitis and demodex blepharitis |
No reported adverse effects |
[35-37] |
|
Tea tree face wash (Terpineol containing face wash) |
Retrospective study, 135 patients with demodectic blepharitis.Scrubbing on eyelids and eyelashes, 4 weeks |
Essential oil of tea tree oil, 4 Terpineol kills demodex folliculorum. Safe and effective in ocular tissues. |
Skin dryness, burning and redness in people with acne. |
[39, 41, 42] |
|
Blephapad combo. (Wet wipes containing 4 Terpineol, hyaluronic acid and aloe) |
Open label, randomised controlled studies, 18 patients. Place wet wipes, 3-5 mints with slight pressure. Twice daily, 4weeks |
Blephapad combo more effective than standard treatment. Useful in patients with blepharitis and meibomian gland dysfunction. |
Soreness, itching, redness |
[44] |
| Blephagel ®
Poloxamer gel based cosmetic cleanser. |
Open study without comparator, 33 female subject.Eyelid cleansing and massaging twice daily, 21 days |
Effective and acceptable for routine use to patients with blepharitis and sensitive eyes. |
Prickling, watering eyes | [45] |
|
MGO Manuka honey eye cream. (Treated eyes and control eyes were compared in baseline) |
Randomised, paired eye investigator-masked trail, 25 healthy human subjects. Applied at night on eyelids, 14 days |
Manuka honey cream is a natural antibacterial and anti-inflammatory agent. Safe to use in blepharitis patients |
No significant side effects. Transient ocular stinging. | [46] |
|
Posiformin 2%® eye ointment. (2% bibrocathol Treatment group compared with placebo group) |
Multi-center, randomized, double-masked, placebo-controlled parallel-group comparison study, 197 patients.Apply 3 times on eyelids, daily, 2 weeks |
Compared to placebo, patients received bibrocathol shows high improvement. |
Ocular discomfort |
[47] |
|
Indraductal meibomian gland probing. (Pre-treatment compared with post treatment after 6 months) |
Longitudinal study, 16 blepharitis patients. Occluded gland probed with 2 mm maskin cannula. |
Targets mainly severe posterior blepharitis patients. Safe and long effective procedure |
No worsen symptoms and adverse effects. |
[48] |
Discussion
In synthetic therapy eye drops of antibiotics alone or in combination with steroids are given for the management of blepharitis. Azithromycin, erythromycin, norfloxacin, tobramycin, moxifloxacin, doxycycline and minocycline are the most commonly used antibiotics. These are recommended for the short term applications because of development of antibiotic resistance, steroid induced intra ocular pressure raise and other complications as listed in the Table 2. Novel drug delivery systems and formulations with natural origin are reported to be more effective and safe with minimum side effects 31, 32.
Azithromycin, a broad spectrum antibiotic is prescribed in the form of eye drops. In a study reported by Jodi Luchs (2010) azithromycin combined with durasite drug delivery vehicle in Azasite® and this combination contains polycarbophil known to improve the bio adhesiveness of formulation followed by drug penetration to cornea, conjunctiva and eyelids and further improves effectiveness in the treatment of blepharitis 13, 33, 34. Low dose Povidone iodine is very safe and effective antiseptic in ocular tissues. It interacts with cells via poisoning electron transport system, inhibits cellular respiration and destabilize cell membrane. In two different studies, Povidone iodine has been reported in the form of gel formulation for topical application in the eyelashes and eyelids for demodex blepharitis and blepharo-conjuctivitis without any reported side effects 35-38.
Terpineol is the essential oil from tea tree oil which is very effective against microorganisms causing skin and ocular infection especially against demodex mite, within 4 weeks 39-41. The efficacy of terpineol has been studied in two different formulations of face wash and wet wipes 42. The wet wipes also had hyaluronic acid and aloe, which are very effective anti-inflammatory agent 43. Daily hygiene and use of tea tree face wash or wipes has been found to be very safe and effective in reducing the symptoms of all type of blepharitis44.
Blephagel® is a poloxamer based cosmetic gel for cleansing the eyelid in patients with sensitive skin or eyes or contact lens users. It removes mucous, debris, bacteria from eyelid and hydrates eyelid skin. Blephagel´s soothing effect help to use in periocular region routinely without any adverse effects 45.
Manuka honey has antibacterial and anti-inflammatory effect which helps to treat blepharitis symptoms. From study conducted in blepharitis patients with manuka honey loaded microemulsion eye cream found to be more safe and tolerable in periocular area without any adverse effects 46. Bibrocathol (4,5,6,7-Tetrabromo-1,3,2-benzodioxabismol-2-ol) is a topical antiseptic available as 2 or 5 % eye ointment with liquid paraffin, white soft paraffin, and lanolin. According to Pavel et al (2012), the ointment found to be safe and well tolerable in patients with blepharitis 47.
Fermon et al (2015) conducted HCT to treat meibomian gland dysfunctioning by intra-ductal meibomian gland probing using 2 mm cannula under biomicroscopy. Meibomian gland dysfunction is a major problem in severe posterior blepharitis. Long term relief is possible by single treatment itself 48.
Conclusion
Blepharitis is an inflammatory disorder of eyelids and manly observed in school going children with poor hygienic conditions. If remained unattended, this infection may lead to keratopathy, permanent eyelid morphology change, and corneal neovascularization. Topical antibiotics, steroids and calcineurin inhibitors are the recommended first line therapy but their safety and duration of treatment is largely unknown. When compared with synthetic agents, formulations developed with natural ingredients were found to be equally effective with minimum side effects for treatment of blepharitis.
Acknowledgements
I offer my deepest gratitude towards Amrita School of Pharmacy for their constant guidance and facilities.
Conflicts of interest
authors have no conflict of interest.
Funding Source
There are no funding sourse.
Reference
- Christopher MP. Diagnosis and management of blepharitis: an optometrist’s perspective. Dove press journal: clinical optometry 2016; 71-78.
CrossRef - G Nageswar R, SilpaS, Sweta P, HumaR, Bhaskar T, Arttatrana P. Prevalence of ocular morbidity among children aged 17 years or younger in eastern india. Clinical Ophthalmology 2018; 12:1645-1652.
CrossRef - Ajith KD, Ajoy BN. Prevalence of ocular morbidities among school children in a rural block of cachar, Assam. Journal of Evolution of Medical and Dental Sciences 2017; 6:4124-4127.
CrossRef - Vasantha M, Siva SR. Morbidity pattern of geriatric population attending rural community health centre, south India. Akshantala Journal of Research in Preventive and Social Medicine 2017; 1:12-16.
- Ann MT, Alexander J, Leelamoni K, Natasha R, Swati P, Harsha. Prevalence and Predictors of Ocular morbidity among Primary School Children of Urban Kerala. National Journal of Research in Community Medicine 2015; 4:268-277.
- Bansal A, KanthamaniK et al. Ocular Morbidity in School going Children of Kolar District, South India. J Clin Biomed Sci. 2012; 2:175-184.
- Gupta Y, Sukul RR, Gupta M, Phougat A, Jain R, Varshney A. School eye survey in rural population in UP, India. Nepal J Ophthalmol 2011; 3: 78-79.
CrossRef - Katherine D, Bennie HJ. Medical management of Blepharitis. curr.opin.ophthalmol 2015; 26: 289-294.
CrossRef - Ronald ES, Charles WF. Chronic Blepharitis: A review. CLAO journal 1995; 21:200-206.
- Stephen P et al. Treatment of Blepharitis: Recent Clinical Trials. Ocular Surface 2014. doi: 10.1016/j.jtos.2014.05.005
CrossRef - Mihaela AI, ConstantinC, MihaiL, Daniela L, Mircea T, Simona RG, Alexandra B, Carolina C, Monica N, Sabina AZ, Daniel B. Current and future applications of confocal laser scanning microscopy imaging in skin oncology (Review). ONCOLOGY LETTERS 2019; 17: 4102-4111.
- Justin S et al. Randomised double masked trial of eyelid cleansing treatment for blepharitis. The Ocular Surface 2018; 16:77-88.
CrossRef - Jodi L. Azithromycin in DuraSite® for the treatment of blepharitis. Clinical Ophthalmology Dove press journal 2010:4: 681–688.
CrossRef - Roland L. Mechanisms of Resistance to Macrolides and Lincosamides: Nature of the Resistance Elements and Their Clinical Implications. Antimicrobial Resistance2002; 34:482-492.
CrossRef - Sonia P, SushmitaK, Savleen K, PandavS S. Steroid-induced Glaucoma: An Avoidable Irreversible Blindness. Journal of Current Glaucoma Practice 2017; 11(2):67-72.
CrossRef - Giacomo DB, Agostino SV. Oral azithromycin and oral doxycycline for the treatment of Meibomian gland dysfunction: A 9‑month comparative case series. Indian Journal of Ophthalmology 2019:67:464-470.
CrossRef - Atsuki F, Yuichi O, Nobuyuki E, Eiichi U, Shigeki O, Naoki K et al. Therapeutic effects of 0.1% tacrolimus eye drops for refractory allergic ocular diseases with proliferative lesion or corneal involvement. Br J Ophthalmol 2014; 98:1023–1027.
CrossRef - Samir SS. Topical Tacrolimus in anterior segment inflammatory disorders. Eye and Vision 2017; 4:1-7.
CrossRef - Stephen P, Paul Karpecki MD, Victor LP. Treatment of Blepharitis: Recent Clinical Trials. Ocular Surface 2014; doi: 10.1016/j.jtos.2014.05.005
CrossRef - Harikrishnan KV, Rajashree R., Mukesh M, Remya R. Role of omega -3 fatty acids in the treatment of cardiovascular disorders. JPR 2012; 5140-5143.
- Annie S, Daniel NJ, Henry DP, Scheffer CGT. Managing Blepharitis: Tried-and-True and New Approaches. Clinical Update: cornea 2012; 29-31.
- Jose L, Fernando A, Jaime Q, Renzo R. Comparative clinical study of norfloxacin 0.3% and chloramphenicol 0.5% opthalmic solutions in the treatment of acute bacterial conjunctivitis, blepharitis, and blepharoconjunctivitis. Current Therapeutic Research 1992; 52:64-69.
CrossRef - Foulks GN, Borchman D, Yappert M, Kakar S. Topical azithromycin and oral doxycycline therapy of meibomian gland dysfunction: a comparative clinical and spectroscopic pilot study. Cornea 2013; 32:44-53.
CrossRef - Basak SC, KaladharK, Subburaj T. Doxycycline hyclate delayed release capsules with sodium starch glycolate as a pH-dependent pore forming agent. Indian J Pharm Sci2004; 66:704–707.
- Mehdi Z, Neda R, Sanaz S. Comparison of therapeutic effect of topical azithromycin solution and systemic doxycycline on posterior blepharitis. Int J. Opthalmol 2016; 9:1016-1019.
- Hun L, Kyung M, Eung KK, Tae I. Minocycline controls clinical outcomes and inflammatory cytokines in moderate and severe meibomian gland dysfunction. Am J Ophthalmol 2012; 154:949-957.
CrossRef - Junya N, Atsuhiro N, Ryota H, IwaoT. A Case of Seborrheic Blepharitis; Treatment with Itraconazole. Jpn. J. Med. Mycol 2002; 43:189-191.
CrossRef - Michael R, Sanjay NR. Efficacy of Topical Cyclosporin 0.05% in the Treatment of Posterior Blepharitis. Journal of ocular pharmacology and therapeutics 2006;22: https://doi.org/10.1089/jop.2006.22.47
CrossRef - Fernando ESN, Helena MMR, Bernardo KM, Daniela AM, Brenda BC, Ricardo H, Ruth MS, Richard YH. Tacrolimus Ointment for Refractory Posterior Blepharitis. Current Eye Research 2017: DOI: 10.1080/02713683.2017.1339805 1-6.
CrossRef - Rahul B, Prachi K. Comparison of the safety and efficacy of topical Tacrolimus (0.03%) versus dexamethasone (0.05%) for subepithelial infiltrates after adenoviral conjunctivitis. Indian Journal of Ophthalmology 2019; 67:594-598.
CrossRef - Tinu TS, Litha T, Anil KB. Polymers used in ophthalmic in Situ gelling system, International Journal of Pharmaceutical Sciences Review and Research 2013; 20:176-183.
CrossRef - Jackson WB. Blepharitis: current strategies for diagnosis and management. Can J Ophthalmol 2008:43:170-179.
CrossRef - Krenzer KL, Zhang JZ, Coffey MJ, Richardson ME. Safety of repeated topical ocular administration of a polycarbophil-based formulation in several models of ocular surgery in rabbits. J Cataract Refract Surg2012; 38:696-704.
CrossRef - Esen KA, Jason V, Rozemarijn SV, Kurt B, Thierry A, Kendall DP et al. Ocular Surface Distribution and Pharmacokinetics of a Novel Ophthalmic 1% Azithromycin Formulation. Journal of Ocular pharmacology and therapeutics 2009; 25:433-439.
CrossRef - Jesse SP, Kara C, Kevin SS, Joseph AC. Demodex Blepharitis Treated with a Novel Dilute Povidone-Iodine and DMSO System: A Case Report. Ophthalmol Ther 2017; 6:361–366.
CrossRef - Pelletier JS, Capriotti KD, Stewart KS, Barone SB, Capriotii JA. A Novel Transdermal Ophthalmic Preparation for Blepharitis in a Dilute Povidone-Iodine and Dimethyl Sulfoxide (DMSO) System: A Case Series. EC Ophthalmology 2018; 9: 129-134.
- Jesse SP, Kevin PS, Kara C, Joseph AC. Rosacea Blepharoconjunctivitis Treated with a Novel Preparation of Dilute Povidone Iodine and Dimethylsulfoxide: a Case Report and Review of the Literature. Ophthalmol Ther 2015; 4:143–150.
CrossRef - Diana GH, Alejandro JV, Gustavo AM, Lorena LO. Demodex and rosacea: Is there a relationship. Indian Journal of Ophthalmology 2018; 66:36-38.
CrossRef - Chen WS, Sean T, HosamS, Anny MS Cheng, Scheffer CG Tseng. Safety and efficacy of 4-terpineol against microorganisms associated with blepharitis and common ocular diseases. BMJ Open Ophth 2018; 1-6.
- Gao YY, Di Pascuale MA, Li W, A Baradaran Rafii, Elizondo A, C-L Kuo, Raju VK, S C G Tseng. In vitro and in vivo killing of ocular Demodex by tea tree oil. Br J Ophthalmol 2005; 89:1468–1473.
CrossRef - Yucel K, Erhan Z. Evaluation of the efficacy of tea tree oil on the density of demodex mites (acari: demodicidae) and ocular symptoms in patients with demodectic blepharitis. J. Parasitol 2018; 104: 473–478.
CrossRef - Orla M, Veronica O, Aoife L-McK. The efficacy of tea tree face wash, 1, 2-Octanediol and microblepharoexfoliation in treating Demodex folliculorum blepharitis. Contact Lens and Anterior Eye.2018; 41:77–82.
CrossRef - Divya G, RajithaP, Swati G, Jayakumar R, Sabitha M. Acitretin and aloe-emodin loaded chitin nanogel for the treatment of psoriasis. European Journal of Pharmaceutics and Biopharmaceutics 2016; 107:97–109.
CrossRef - Valentina DL, Adriano C, Giovanna CS, Gabriele P, Donatella B, Vincenzo S. Efficacy and Safety of Wet Wipes Containing Hy-Ter®Solution Compared with Standard Care for Bilateral Posterior Blepharitis: A Preliminary Randomized Controlled Study.Ophthalmol Ther 2019; 8:313–321.
CrossRef - Serge D. Tolerability and acceptability of Blephagel: a novel eyelid hygiene aqueous gel. Clinical Ophthalmology 2012; 6: 71–77.
CrossRef - Jennifer PC, Michael TM Wang, KalaivarnyG, Ilva DR, Simon S, Chee SL et al. Randomised masked trial of the clinical safety and tolerability of MGO Manuka Honey eye cream for the management of blepharitis. BMJ Open Ophth 2017; 1-10.
CrossRef - Pavel AB, Nikolai S, YuriyD, Andrei K, NikN, Matthias M et al. Successful treatment of blepharitis with bibrocathol (Posiformin® 2 %). Graefes Arch ClinExpOphthalmol 2012; 250:1869–1875.
CrossRef - Fermon S, Hindi Zaga I, Alvarez MD. Intraductal meibomian gland probing for treatment of blepharitis. Arch SocEspOftalmol 2015; 90:76–80.
CrossRef








