Vinayak Majhi1*  , Sudip Paul1
, Sudip Paul1 and Goutam Saha2
and Goutam Saha2
1Department of Biomedical Engineering, North-Eastern Hill University, Shillong, India, 793022
2Department of Information Technology, North-Eastern Hill University, Shillong, India, 793022
Corresponding Author E-mail : majhi.vinayak@gmail.com
DOI : https://dx.doi.org/10.13005/bpj/2006
Abstract
After two hundred years of the Shaking Palsy by Dr. James Parkinson, we have revealed many factors and causes behind Parkinson’s disease (PD). Before Shaking Palsy the symptoms were known as some disorders. 5000 years ago in Ayurveda, the Indian medical manuscript and 2500 years ago in Nei Ping, the first Chinese medical manuscript some disorders were mentioned those are similar to PD and also several treatment procedures were also described. This proves that PD is not a disease that evolved only in modern industrial age. But it is true that, after Shaking Palsy, this PD comes into spotlight of the modern medical practices. To understand this disease we need to go through the complete etiology of PD including Genetical and Environmental factor that may lead us to the different causative factors of PD. Each factor has its unique signification and outburst as a multiple combination of different Parkinsonian symptoms. In this review we will discuss about all possible etiological factors related to PD with different Parkinsonian symptoms categorized with motor and non-motor symptoms. Before going to the brief review, we will also discuss about several milestone researches which actually open a new window in PD research on its time.
Keywords
Etiology of Parkinson’s disease; Mitochondria; Motor Symptoms; Non-Motor Symptoms; Substantia Nigra
Download this article as:| Copy the following to cite this article: Majhi V, Paul S, Saha G.Systematic and Symptomatic Review for Parkinson’s Disease. Biomed Pharmacol J 2020;13(3). |
| Copy the following to cite this URL: Majhi V, Paul S, Saha G.Systematic and Symptomatic Review for Parkinson’s Disease. Biomed Pharmacol J 2020;13(3). Available from: https://bit.ly/2QgSqBP |
Introduction
Parkinson’s disease (PD) is a most affective and completely incurable neurodegenerative disorder after Alzheimer’s disease, mostly found in elderly population1. There are near about 10 million people suffer in Parkinson’s disease.2 United States alone spends near about $25 billion per year in the treatment of Parkinson’s disease.3 According to the US Census Bureau population projection, the PD patients will increase approximately 930,000 by 2020 and in 2030 the affected PD patient will be near about 1,238,000.4 In figure: 1 we can see the approximate number of PD patients in different countries.5, 6
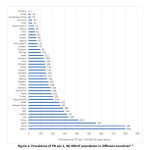 |
Figure 1: Prevalence of PD per 1, 00, 000 of population in different countries5, 6 |
This statistics shows the importance of concernment about Parkinson’s disease. From 1915 there are more than 85,000 paper published on Parkinson’s disease.1
The diagnosis of any disease can be initially done through four different stages.
Subjective Study, where patient itself tells his/her problems.
Objective Study, where a medical practitioner observes the patient and tries to find new unexpressed symptoms or justify the expressed symptoms stated by the subject.
Pathological Study, where the patient is told to perform different pathological tests like urine, stool, cholesterol, blood etc.
Imaging and Radiological Study, here medical practitioners guide the patient to perform different radiological test to view the actual projection of the affected area like CT Scan, MRI, EEG, EMG etc.
These four methods are generally used alternatively in case of every disease diagnosis, but besides this there are several other studies can be done for understanding the disease situation and progress method or the cause of occurrence. This type of study include Genetical study like protein sequence analysis, DNA sequencing etc.
In case of diagnosis of Parkinson’s disease the objective study takes most important role. Clinical rigidity, resting tremor, bradykinesia and postural instability are the four main symptoms for diagnosis of PD. The pathogenic mechanism of protein, conformational changes and the cause of neurodegeneration are still unknown to us.1 In pathological study there are few biomarkers can describe the occurrence of Parkinson’s disease like Colonic biopsy and Skin biopsy to find the α-synuclein staining biomarker, Serum/plasma test biomarker used as uric acid, glutathione, other low molecular weight compound. In Imaging and Radiological study we have positron emission tomography (PET) scan to identify C-dihydrotetrabenazin and F-dopa biomarker, Single-photon emission computed tomography (SPECT) to identify I-2β-carbomethoxy-3β-(4-iodophenyl)tropane (I-CIT) biomarker, Specialised MRI for diffusion tensor imaging and Transcranial sonography Cardiac imaging for I-metaiodobenzylguanidine biomarker. In genetic study Multiplex Ligation-dependent Probe Amplification and gene sequencing is being done.7
Now a day’s Neuropathological diagnosis method is the most used diagnosis procedure for PD but in general there are no standard pathological diagnosis procedure established. The only factor that makes PD different form the other neurodegenerative diseases that is the moderate or severe loss of neuron in Substantia Nigra pars compacta (SNpc) with Lewy bodies in surviving SNpc neurons.7
If we consider the several researches which are progressed after Shaking Palsy it is quite difficult to find the actual cause of occurring neurodegeneration for PD but there are several other clinical syndromes those come to in consideration leading towards PD. These clinical entity and syndrome are now called as “Parkinsonian Syndromes” or the entity of individual factor called as “Parkinsonism”.8 In this concern the Parkinsonian syndrome may be present in different disease also like one study by Yun Chen. et al. it was found that there were 22 different symptoms those overlap in 14 different neurological insults like Alzheimer’s disease, Huntington’s disease, PANDA, Brain Tumour, Blast induced TBI etc.9 Other point that also justify, PD is not a unique neurodegenerative disease, is Parkinsonian syndrome can be found in neurofibrillary tangles where Lewy bodies are not affected. The highly variable nature of idiopathic Parkinsonian syndrome in the beginning of PD those are more stable in extreme stage. Lewy bodies and nigral neuronal loss can be found in several other neuro degenerative disease which occur in elderly ages without having Parkinsonian syndrome so we cannot say lewy bodies are the associative factor for idiopathic parkinsonism.8 In later stage of this review we will discuss about the etiology of Parkinson’s disease with the different Symptoms related to Parkinson’s disease with an overview of milestone research on Parkinson’s disease starting from the Shaking palsy.
Milestone of Clinical Intervention in Parkinson’s Disease
Parkinson’s disease was clinically described by Dr. James Parkinson in 181710 but the name “Parkinson’s Disease” was given by Jean-Martin Charcot11 Parkinson observed six different people, three of them were his patient another two met in street and the other one was observed in distance, before describing the clinical symptoms of this disease. After this he described the posture pattern of this disease and festinating gait including tremor and its expanding nature trough out the body with passing day.12
Charcot in 1881 first observed that the tremor is not essential for having PD and he also described that PD has its unique significance than other tremorous disorders. He also included several other symptoms like rigidity, slowed movements, hunched posture and a tendency of soft speech. In further studies by Charcot and his students, they found bradykinesia in face and contracted forehead muscles that caused forehead wrinkle. In cause he described that the patient having Parkinson’s in generally keep their eyes open for very long times that may cause of having wrinkle on their forehead. He tried to cure those patients with different chemical compound like camphor, zinc oxide, silver nitrate etc. but the reason behind using these was not described by the Charcot. When he found there was no effect of this medication of the patient he discovered some new therapeutic methods of giving vibration to the patient. To provide rhythmic vibration Charcot develop a special type of electrically operated chair called “shaking chair”, besides this, one of his student, Gilles de la Tourette developed a special type of helmet that can capable for giving vibration to the patients head. With these therapy they were able to improve some sensory symptoms and rigidity of the patient but the tremor remained unchanged.13
In 1887 Sir William Richard Gowers from London published his work in “Manual of Diseases of the Nervous System” where he wrote his personal experience with 80 PD patients. He first found that PD is slightly male predominance.14
Dr. Paul Richer and Henri Meige first describe the clinical and morphological data of progressive PD with pictorial evidence in 1895. The different PD patient’s portrait give and objective view of the PD. This was the new kind of specimen for describing a disease. It was called “scientific artwork”.15, 16
Robert Henry Clarke and Sir Victor Horsley in their collaborative work developed stereotaxic equipment for targeting brain nuclei for hyperkinetic disorder where PD also a hyperkinetic disorder.17
Hans Willige in 1911 describe the juvenile form of Parkinson’s disease.18
Russell Meyers in 1940 describe the involvement of basal ganglia for Parkinsonian tremor and rigidity.19
In 1953 Irving S. Cooper observed two different patients; one of them was 36 years old having severe Parkinsonism and another was 38 years old who had post-encephalitic parkinsonism. After the surgery on right anterior choroidal artery the rigidity and resting tremor in contralateral extremities was disappeared for both the patients.20
In 1910 dopamine was first discover by George Barger and James Ewens.21 But the use of dopamine in Parkinsonian syndrome using levodopa was first prescribed by Oleh Hornykiewicz and H. Ehringer in 1960. They first discover the involvement of dopamine in PD due to the deficiency of dopamine in striatum of basal ganglia.22
All these discoveries are the milestones to the progressive research of Parkinson’s disease which lead us to more concern about the Parkinson’s disease. In modern twenty first century there are several diagnosis methods and drugs also been developed but these discoveries are the main concrete milestone in the field of PD research.
Etiology of Parkinson’s Disease
In early days it was thought to be Parkinson disease have mainly two factors Genetical and Environmental factors.23 After the industrial revolution the use of many poisonous chemical, toxic materials increased, that causes illness, internal injury and several other diseases induced by the industrial waste outcome some of which chemical may cause Parkinson’s disease.24 Similarly Genetical causes are also considered as single gene Mendelian disorder. In genome studies for complex disease, the non-coding DNA is considered as a risk factor of having the different risk polymorphism and also the gene regulatory allele-dependent differences. In case of Parkinson’s disease there are few genetic risk can be found by the involvement of neuronal cell subpopulation which affects the brain region.25 But after several studies and research it was found that the main generic cause of happening PD is the dopamine deficiency in nigrostriatal dopamine system. In this section we will discuss about all the different factors that may involved in causing PD.
Canonical Etiology of Parkinson’s Disease
Dopamine Deficiency
Dopamine is a neurotransmitter which exists intra-neuronally throughout the different pathway of the central nervous system. In the occurrence of PD the pigmented cell of Basal ganglia where Substantia Nigra and Ventral Tegmental Area are degenerated and the natural production of dopamine is also depleted. As dopamine controls the neurotransmission so the loss of dopamine creates different motor disability dysfunctions like tremor, posture instability, bradykinesia etc. In adverse effect of dopamine degeneration the neuronal loss may occur.25 To maintain the dopaminergic deficiency L-dopa is used to make dopamine balance because direct use of dopamine have no effect in brain because it cannot reach through the blood brain barrier. But during the synthesis of dopamine from L-dopa produces oxidant agent that create several reactive oxygen species like Hydrogen peroxide, Hydroxyl ion etc. which can damage the cellular membrane of neuron. For that reason it was found that higher use of L-Dopa can damage the more neuronal cell in Substantial Nigra.26
Nigral Glutathione Deficiency
Nerve cell is highly metabolically active cell in the body. The balance of oxygen and glucose maintains the healthy nature of nerve cell. When this metabolic balance is disturbed, the free radical in the cell increases, glutathione, the natural antioxidant agent cannot detoxify the metabolic free radicals which causes the oxidative stress. Increasing oxidative stress is considered to be a cause of neurodegenerative disease like PD. Glutathione helps to detoxify the superoxide and hydroxyl radicals. The deficiency of glutathione in substantial Nigra region may cause severe oxidative damage,27 that may increase the chance of occurring PD. It was found that the Glutathione deficiency in Substantia Nigra of a PD patient is near to 40% than a controlled subject.28
Mitochondrial DNA Mutation
During the ATP synthesis in mitochondria electron transfer through the protein complexes to the molecular oxygen and generate a proton gradient in the inner membrane of the mitochondria, finally this proto gradient is used to produce the ATP and it also maintain the calcium level in the cell. There are four protein complexes (I-IV) in mitochondrial electron transport chain. Beside this mitochondrial also generate several reactive oxygen species as a byproduct that can damage the DNA, protein and lipid. In the time of evolution mitochondria provide the genetic material to the nuclease but some form of DNA remain in the mitochondria this DNA is called mitochondrial DNA which independently replicates the cell cycle and nuclear genome also. This replication creates multiple copies of mitochondrial DNA which is described as mutant mitochondrial genome and this phenomenon is called Heteroplasmy. When this Heteroplasmy comes to some threshold level it causes several biochemical dysfunctions. This mitochondrial mutation can also be one of the cause of neurodegenerative disease like PD.29 Mitochondrial dysfunction has two major properties like generation of reactive oxygen species (ROS) and decreasing complex I enzyme activity. Degeneration of Complex I activity have influence in the generation of more ROS in Substantial Nigra which increases the oxidative stress in the neuronal cell and degeneration of neuronal cell in Substantial Nigra increases the risk of having PD.30
Hereditary form of Parkinsonism
Sometimes it is found that PD has some hereditary effect by which in some families PD comes generation after generation. Generally PD is considered as monogenetic disorder means single abnormal gene mutation in autosomes causes the disease. According to the PD genomic classification 18 different genomic loci are generally considered which we call as PARK with ascending chorological order like PARK1, PARK2…PARK18 etc. There are seven individual genes are mostly associated with Autosomal recessive form or in Autosomal dominant form of parkinsonism. The Autosomal recessive forms PARKIN (PARK2), PINK1 (PARK6), DJ1 (PARK7) are the responsible factor for Early Onset Parkinson’s Disease (EOPD). In Autosomal dominant form there are four major locus, SNCA (PARK1, PARK4), LRRK2 (PARK8), VPS35 (PARK17), EIF4G1(PARK18) they are responsible for Classical PD like different Parkinsonian symptoms, effect on cognitive and behavioral changes.31, 32
Infectious Cause of Parkinson’s Disease
Parkinson’s disease can be caused by different kind of viral or bacterial infection there are several record can be found where Parkinsonian symptoms are broadly appear within or after the infectious period. In general if the Substantial Nigra is being affected by the infectious disease then chances of occurring PD may increase.
Gastrointestinal Infection Caused PD
Gastrointestinal (GI) inflammation can alter the microbiota compositions. In PD gastrointestinal disorders are commonly found.33 But this disorder are mostly developed before developing the acute PD symptoms. Dysbacteriosis can also increases the chances of having oxidative stress which may influence in developing PD symptoms.34 This gastrointestinal dysfunctions can affect the autonomous nervous system that is enteric nervous system (ENS) of Gut wall. The ENS communicates with the brain bidirectionally through vagus nerve which is called brain-gut axis. Pathological peptides travels between Gut and Brain through the neuronal chain of neuron and fiber from ENS and vagus.35
An overactivity in GI can hamper the peripheral immune cells response. This may disturb the integrity of the blood-brain barrier (BBB) and its role against bacterial lipopolysaccharides (LPS) and other toxins. It was found that the PD patient always have 50% more intestinal microbiota populations compare to a control subject.34
The infectious diseases that lead to PD reported are as follows36
Japanese Encephalitis (caused by Japanese encephalitis virus a mosquito-borne flavivirus)
HIV Encephalopathy (Long running HIV infectious brain damage)
Encephalitis lethargica (sleeping sickness transmitted by tsetse fly)
Coxsackie B viral infections (caused flu, gastrointestinal diseases even death spread through dirty open wound, coughing )
Subacute sclerosing panencephalitis (Caused by measles virus in childhood)
Poliomyelitis (Caused by poliovirus)
Saint Louis encephalitis (spread through infected mosquito)
Western equine encephalitis (spread through Culex and Culiseta mosquito)
West Nile virus (transmitted through bird and mosquito)
Epstein-Barr virus (Human gammaherpesvirus 4, one of the human herpesvirus)
Mycoplasma pneumonia (bacterial respiratory infection)
Syphilis (Sexually transmitted disease by bacterial infection)
Borreliosis (Infectious disease caused by Borrelia bacteria)
Toxoplasmosis (Opportunistic infections caused by Toxoplasma gondii in basal ganglia)
Neurocysticercosis (infection caused by the egg of Taenia solium)
Tuberculosis (caused by bacteria named Mycobacterium tuberculosis)
Malaria (caused by plasmodium parasite transmitted through female Anopheles mosquitoes)
Toxicity Caused Parkinson’s Disease
In everyday life starting from agricultural sites to large industrial sector many toxic compounds are used either to increase productivity or as a protective agent. Several pesticides, herbicides are used in agriculture which are deposited in either soil or in the water. Industrial wastes also create pollution to the environment in all the way like soil, air and water too. These toxic chemicals badly affect our body organs and tissues. In several studies it was found that after the industrial revolution the occurrence of PD incident increases. With previously discussed statistics we can say it will increase more day by day. In this section we will discuss about few toxic compounds that increase the risk factors of having PD.
MPTP (1-methyl 4-phenyl 1,2,3,6-tetrahydropyridine) is a neurotoxicant inducer that causes Parkinson’s disease within three days after toxification. Generally it is distribute on street as toxification drug. MPTP inhibit the formation of dopamine by affecting dopaminergic neuron in Substantial Nigra.
Carbone disulphide (S=C=S) was previously used as pesticide which can also causes PD with different Parkinsonian symptoms. In modern times the uses of Carbone disulphide is banned but sever industrial uses are still there with this compound. Carbone disulphide reduces the formation of dopamine from L-Dopa by reacting with the essential agent pyridoxal 5-phosphate which helps in synthesis of dopamine from L-Dopa.36
Manganese (Mn) is an essential traced element in the body which helps to maintain biological function. Excess exposure of manganese causes the PD by destroying the tyrosine hydroxylation which helps in formation of dopamine.36
Paraquat ([(C₆H₇N)₂]Cl₂) is mainly used as herbicides in agricultural sector. The use of Paraquat as an herbicide is for the electron interceptor between ferredoxin acceptors and NADP. It also reduces the O2 to super oxidant O(2-) which reduces the photosynthesis. Similarly the Paraquat also affects the mitochondrial electron transportation chain in a cell. In mice model it is tested that Paraquat induces dopaminergic degeneration in the Substantia Nigra.37
Rotenone (C23H22O6) is used as a insecticides which affects the well water. It is mostly use in treating the parasitic mites in poultry. The direct nigrostriatal infusion can affect the dopamine formation by inhibiting the tyrosine hydroxylation which causes the several Parkinsonian symptoms.38
Other toxic chemicals like Glyphosate herbicide, Toluene (solvent used in Painting colour), Organophosphate, n-hexane (used as a solvent for extraction of vegetable oil), Methanol, Maneb (Manganese based fungicide), Heroin pyrolysate, Ecstasy (3,4-Methylenedioxymethamphetamine), Cyanide poisoning (Sodium cyanide, Potassium cyanide produced by bacteria and fungus), Copper(Cu), Dieldrin (Pesticide), Mercury etc. are have few potential effect on Parkinsonian symptoms generation.6, 24, 36
Symptoms of Parkinson’s Disease
Parkinson’s disease symptoms can be classified into two major categories which are Motor Symptoms and Non-Motor Symptoms. In which motor symptoms are the major diagnostic factor for the detection of Parkinson’s disease.
Different Motor Symptoms Related to Parkinson’s Disease
The clinical aspects of PD basically have the PIGD form that is Postural instability and gait disorders but it is actually one of the subtype of PD symptoms.39
In central nervous system motor system is the main responsible part that governs the body movement it is consist of two different parts that is pyramidal and extrapyramidal system. The disorder in motor system causes the involuntary movement.40 The motor symptoms are occurred only in the situation of motor system disorder. There are several motor symptoms are found that are directly or indirectly related to PD.
Akinesia
Akinesia is a motor disability symptom in which a person is unable to move their muscle on their own. A similar sign of this symptom is freezing, inability of standing, writing, even speaking, It is one of the four cardinal symptoms of PD.41 In one study it was fund that 47% patients of total 6620 patient in Germany having PD confirmed the symptom of Akinesia.42 Sometimes we called this symptom as Gait Disturbance. There is several form of this Akinesia symptom based on their level of motor dysfunctionalities and it is divided into some sub group.
Retropulsion and Pulsion
A tendency of stepping back is called Retropulsion and Pulsion is a stepping forward direction. Both of these test is important for gait disturbance analysis. In generally a person with normal gait takes complete one or two step. But in this case a patient takes uncountable steps for instead of taking a single step. This Pulsion and Retropulsion can initiate when a patient tried to start walking or changing the direction of the movement.24
Freezing of Gait
Freezing of Gait (FOG) is most embarrassing and awkward type of symptom. With this symptom a patient cannot move for a few seconds when he/she wants start walking for this reason it is called “Magnetic Feet” symptoms.24 FOG is justified as the disturbance in Basal Ganglia especially in motor sensory feedback loop dysfunction. In a study of 91 patients by N. Giladi et al. it was found that 53% of all patients with FOG.43 The duration or the frequency of having Fog depends upon circumstances and action taken. The anxiety of walking can increase the frequency, besides the rhythmic walk can also bypass the occurrence of FOG.24 FOG can also have some types depending upon the occurrence of FOG.44
Destination Hesitation(adjusting steps after arriving in the destination)
Hesitation in tight quarters (Freeze in front of doors narrow space or in change of floor pattern like carpet to tiles)
Open space hesitation(Freeze in open space)
Start hesitation(Difficulties in start moving)
Turn hesitation(Difficulties in taking turn)
Turning
Turning or changing direction is also very difficult for the PD patient which is quite other than turn hesitation. Here a patient does not freeze in a turning but because of this turning difficulties patient may fall down while turning. Basically a turning like motion is result of balance, coordination, and equilibrium. For a PD patient all these things going towards worse day by day so normally it becomes difficult while taking turn.24
Shuffling Gait
In shuffling gait condition patient stooped waking and shuffling his steps with slow arm movement while walking or sometimes arms are always held in front of the body. In his situation toe and heel overlapped.45 This symptoms can also be thought as the effect of posture instability, rigidity and impaired movement.24
Festinating Gait
Festinating gait (FSG) symptom was first discovered by Dr. James Parkinson and it was mentioned in his novel work Shaking Palsy. With FSG, patient tries to maintain the centre of gravity while they are always lean in forward direction and have a chance to fall down by the face, to avoid this PD patient used to make small steps that make the patient of having the pace of running. In a study done by Giladi, N et al. it was found that 32% of 81 patients experienced FSG more than one time in last thirty days before the study conducted [46]. Another study by Ou, Ruwei et al. with 140 PD patients in China, found 29.2% patients who reported FSG.47
Foot Drag
Parkinson patients with Foot Drag gait condition drag their foot either one or both depending upon the dysfunction which hamper the continuous motion of movement. Sometimes with these difficulties climbing the stair also become very difficult.48
Bradykinesia
The slowness of movement is called as Bradykinesia. This is the adverse effect of basal ganglia disorder.49 It is very difficult for any PD patient with Bradykinesia in continuous repetitive movement like finger tapping.50 Sometimes functional electrical simulation (FES) found to be quite helpful for getting relief from Bradykinesia of PD patient.51 Bradykinesia also varies with patient’s emotion. Sometime patient with excitement can perform much faster task then normally dose in Bradykinesia. This phenomena is called “kinesia paradoxica”.42
Hypokinesia
While Bradykinesia refers to slowness of movement in the time of execution, the Hypokinesia refers as a less movement activity.52 It is measured by the activity monitoring system where we observe how much activity is performed by a patient in a day. The causing factor of Hypokinesia is the basal ganglia disorder. One of the common symptoms to identify the Hypokinesia is the less number of eye blinking that also causes the eye irritation.24
Hypomimia
The reduction of facial expression in PD patient is a noticeable objective symptom which is called as Hypomimia. In some cases it was found that the patient with Hypomimia had to reduce their quality of life for this disorder. In early diagnosis for this symptoms become quite difficult because of the ignorance or misunderstanding of the symptomatic feature. To overcome this issue PD patient are suggested to react on some event very frequently.53 In a study done by S M, Fereshtehnejad et al. with 314 idiopathic PD patient in Southern Sweden, found that 91.6% patient having Hypomimia.54
Hypophonia
This symptom of PD marked as slowness of voice. When the PD affect the vocal cord muscle then the loudness of the patient voice decreases. In general 70% to 90% PD patients are found with this disorder.55 Sometimes speech therapy also helped in improving this disorder. It can be treated with percutaneous collagen augmentation.56
Dysarthria
In some PD patient the speech disorder found due to the effect of Bradykinesia involved in mouth, throat and chest muscle. The main cause, behind it is the damage in central or peripheral nervous systems.57 Reduction of frequency range of a PD patient indicate the symptoms of Dysarthria.58
Dysphagia
Sometimes it is called as the difficulties in shallowness. Dysphagia varies from 40% to 95% of PD patient. Because of this disorder several other complication may occur like dehydration, Nutrition deficiency, lungs infection, coughing and difficulties in breathing also.57
Dystonia
Dystonia is defined as a involuntary muscle contraction.59 Sometimes it’s also felt painful due to muscle rigidity. In case of Dystonia, basal ganglia involvement is considered. United calefactory also considered for Dystonia.36 Dystonia can also be divided into two broad categories.
Continuous Dystonia
Twisted and repeated motion due to continuous contraction of muscle.36 Continuous Dystonia also classified into two major groups
Primary Dystonia
This is described as when a person having only Dystonia and there is no other neurological disorder is found. Primary Dystonia can also have some sub classes like
Adult Onset Dystonia
When person suffers in Dystonia only in adulthood like after the age of 30.
Centralized Dystonia
Dystonia affects in full body.
Childhood Onset Dystonia
This is also called Early onset Dystonia mostly happen in childhood, affecting the leg, arm hand. The problem encounters during the difficulties in twisting or bending the body or arm or leg.
Focal Dystonia
It is also a kind of adult onset Dystonia mainly affected in the special parts of the body like Foot which is called Foot Dystonia and Oromandibular Dystonia, affecting the face, jaw, tongue which creates difficulties in opening and closing mouth.
Inherited Dystonia
Dystonia that passes through genetically from parent to child.
Segmental Dystonia
This type of Dystonia affects different adjacent part of the body. It also categorized in to some groups like, Axial Dystonia, affects the midline of the body like chest, back. Brachial Dystonia affects on arm or trunk. Cranial Dystonia, affecting any part of the head. Crural Dystonia, affects leg or in trunk. When Dystonia affects two or more unilateral body parts then it’s called Multifocal Dystonia.
Sporadic Dystonia
When a person found to be affected by Dystonia causing Genetical influence but in his family there is no history of Dystonia.
Secondary Dystonia
It is the resultant Dystonia due to brain injury or adverse effect of medication.
Fluctuating Dystonia
The severity of Dystonia that varies in different period of the day.36
Postural Instability
Posture is defined as the orientation of the body during movement taking the body mechanical supports agent, the gravitational force while the balance is maintained by the body posture in movement. So posture instability problems define as the difficulties in maintain the body posture that should to be in equilibrium, it also affects the maintaining the balance while in motion. It was found to be most difficult to maintain the normal lifestyle with this disorder. This predominant symptom of PD mostly found in the later stages of the PD progression.60, 61 To identify the postural instability, a person is pushed with precaution and it can be found that the pushed person moves with short few steps in the direction of the pushing force, before come to a stable condition.24
Rigidity
Rigidity is like stiffness in body arm, leg. This Stiffness can be demonstrate like increasing resistance while stretching the muscle,62 It is also one of the symptoms of Parkinson’s disease. But cause of stiffness depends upon other various factor excluding basal ganglion involvement, so this symptom usually not taken as a predominant symptoms of PD.63 Pathophysiology of this stiffness can be described by the involvement of brain stem, spinal cord, higher cortical circuits, for this reason the occurrence of rigidity in PD is difficult to justify.63 Sometimes FOG can be misunderstood with the Rigidity. Patient can complain about the Stiffness while having different types of FOG. The stiffness can only be diagnosed by the trained clinician with proper experiment and diagnosis through EMG, MRI etc.
Tremor
In Parkinson’s disease tremor is the only one essential symptom. Basically tremor is a rhythmic involuntary movement of muscle where the frequency of tremor occur between 4Hz to 6 Hz. Pill-rolling tremor is one of the identifying marks for Parkinson’s disease where the contracted index finger tries to touch the thumb.42 Tremor can also be classified into two broad categories that is essential and Parkinsonian tremor.
Essential Tremor
Essential Tremor (ET) is the tremor coming from the heredity of a patient. In general there may not be any possibility of having PD while having ET. But it was found that the chances of occurring PD may increase with ET.64 Essential tremor may have several types like Dystonic tremor, Isolated chin tremor, isolated voice tremor, primary orthostatic tremor, primary writing tremor position specific tremor, task specific tremor, but all are not so related with PD.36
Parkinsonian Tremor
Parkinsonian tremor is the PD specific tremor occurs due to degeneration of dopaminergic cells in Substantia Niagara.65 Parkinsonian tremor can be classified into several types like Action tremor, Kinetic tremor, Resting tremor and Postural tremor.
Action Tremor
Action tremor is happened with voluntary muscle movement. Action tremor can be subdivided into two major groups like Kinetic Tremor and Postural Tremor.
Kinetic Tremor
The presence of tremor while voluntary movement done, is called Kinetic Tremor.66 Kinetic tremor can also subdivided in three major types depending upon the occurrence of the tremor, like Intention Tremor, Simple Kinetic Tremor and Task specific Kinetic tremor.
Intention Tremor
This type of tremor occurs due to voluntary movement towards a target. For example try to touch something may increase the frequency of tremor when it appears closer to the target.67
Simple Kinetic Tremor
This type of kinetic tremor happens with voluntary movement but there is now goal or task is undefined. Simple rhythmic muscle contraction relaxation of elbow or forearm during motion is an example of this type of tremor. In Simple Kinetic Tremor the frequency of tremor remain unchanged during its occurrence.68
Postural Tremor
Postural tremor happens when patient try to maintains his posture against the gravitational force.66 Postural Tremor can also be classified into two sub categories, one is Isometric Tremor and another is Position Specific Postural Tremor.
Isometric Tremor
This type of tremor occurs when patient tries to maintain his posture while holding some object like lifting something or moving some object from one place to another place. Basically this type of tremor can occur with other tremor also.68, 69
Position Specific Postural Tremor
It is also a variation of Postural Tremor. This kind of tremor occur only when patients hold a particular posture like “wing-beating” a tremor when hand comes near to the mouth or nose.70
Resting Tremor
This type of tremor occurs to a person in rest. That means no balance or kinetic motion to maintain the body posture is involved against gravitation force. The common pill rolling tremor is a most appropriate example of resting tremor in PD.42 Resting tremor can occur in different body parts like arm, hand and leg also. 90% of PD patients generally report of having resting tremor. Resting tremor may also happen with people having Essential tremor but on those cases the tremor may decrease while patient having walk. Any patient having PD, resting tremor may increase while walking71 and these are the basic difference between Parkinsonian Resting tremor and Essential Resting tremor. The frequency of resting tremor lies between 4Hz to 6Hz.66
Kinesia Paradoxica
This symptom is quite ambiguous by its nature because of its sudden occurrence. It is actually a sudden transient ability by some external stimuli of a PD patient to perform any task what they previously unable to perform. A life threatening event or some external stimuli can initiate this symptom.72 The cause behind this phenomenon can be hypothetically derived through the theory of brain plasticity, that is the ability of brain for changing the structural and functional organization to adopt new functional requirements.73
Falls
A recurrent falling is a motor dysfunction symptom for a PD patient. Approximately 70% of PD patient fall down once in a year.74 Fall can occur when a PD patient generally changes his position like sitting to standing, standing to walking, or while changing the direction of movement.24 A PD patient may realize the fall when it about to happen but unable to resist due to loss of balance. Approximately 50% of the PD patient feared about falling.75
Different Non-Motor Symptoms of Parkinson’s Disease
Non motor symptoms are considered as diverse effect of Parkinson’s disease. According to the neuron atomic stand point these non-motor symptoms can be divided into five major groups that is the symptoms related to cortical dysfunction, Symptoms of Basal Ganglia dysfunction, Brainstem related symptoms, Spinal cord related symptoms and Symptoms related to peripheral nervous system].76
Symptoms Related to Cortical Dysfunction
Cortical dysfunction includes the Cognitive Disorder where the 30% PD patients are having Dementia mostly after the age of 70.77 Different Psychiatric disorder in PD also related to cortical involvement.
Delusion is also very common symptoms in PD patients, mainly in younger patients. Delusion occur due to the anti-parkinsonian medicinal effect or the fear about the disease.76
Dysexecutive syndrome also a kind of cognitive disorder mainly having the deficiency in making response in natural way, or the problem in information generation. It also affects the behavior of PD patient, generally patient becomes more reserve in behavior.78
Similarly Apathy is also one kind of dementia found in PD patient with effect of lack of motivation, interest and energy mostly found in preliminary stages of dementia of PD patients [24].
Symptoms of Basal Ganglia Dysfunction
Most common basal ganglia disorder is Impulse control disorder (ICD), which is a behavioral disorder. Hypersexuality, compulsive shopping, binge eating, Compulsive Gambling are the most common ICD found in early stages of PD. Besides this, patients may also have compulsive motor behavior which is known as punding.76
Brainstem related symptoms: Depression is one of the major non-motor symptoms which are related to Brainstem. Depression in PD sometimes very common, starting from low value of 4% to maximum 70% PD patients have depression of different kind. Different depressive nature like Apathy (lack of motivation, interest, and energy), Crying, Withdrawal from society, suicidal tendency, Dysphoria (feeling uneasy), irritation, sadness, brooding (engaged in deep thought that causes sadness), Pessimism (thinking about worse to be happen) are found in PD patients whether in general PD patients have less guilt felling than other controlled subjects.76
Anxiety is also a very common symptom for PD. 40% patients are found with anxiety with PD. Different types of anxiety may have in different PD patient like Phobia, Panic, fear of institutionalization, urge of dying etc.76, 79
Majority of PD patients are found with Sleep Disorder. Sleep disorder can be defined as excessive day time sleeping, stay awake in night, rapid eye movement (a state of sleeping when dreams completely take place). In the stage of Rapid Eye Movement patient may express huge physical movement like kicking, arm swinging etc. Sleep disorder also includes Muscle twitching, in sever case it was found that leg is pretend to be walking or running by their own violation.24, 36 Sleep attack is also a rare non-motor symptoms of PD.80
Spinal Cord Related Symptoms
Autonomic Dysfunction like Gastrointestinal Disturbances (bloating, Loss of appetite, pain, nausea, vomiting, and distension), Urological Dysfunction (detrusor over activity, urinary incontinency, frequent urinary episodes), Sexual Dysfunction (arousal difficulties, reaching orgasm, erectile dysfunction, Sexual dissatisfaction, premature ejaculation), Excessive Sweating, Orthostatic Hypotension (fatigue, standing dizziness), Sialorrhoea, Swallowing disorders are the most different non-motor symptoms related to PD. Autonomic Dysfunction is caused when autonomic nervous system (ANS) does not work properly. Generally 70% to 80% PD patients are found to be having with Autonomic Dysfunction.76, 81
Symptoms Related to Peripheral Nervous System
Visual Disturbance (motion perception, colour discrimination, contrast sensitivity ), Constipation, Pain (Pain in leg, arm, shoulder, genital pain, Oral Pain, Diffuse Pain), Burning sensation, Tingling Sensation, Tightening Sensation are mostly found in PD patients.36, 76
Conclusion
All the above discussed motor and non-motor symptoms are needed to be considered for the diagnosis of PD patients, although in preliminary diagnosis only motors symptoms are considered for identifying PD patients. It is not a mandatory that, one patient should have all the above discussed motors and non-motors symptoms together. But it may present majorly or minorly to a patient depending upon the Parkinson’s stage. The benefit of discussing above mentioned symptoms is that, it will lead us to find good diagnosis procedure in early detection of PD. It can also support to prevent the patient’s conditions to be more critical. The etiological knowledge about Parkinson’s disease leads us to understand the different causing factors of PD. In the time of diagnosis of PD patient these entire causing factors related to the PD may lead us to determine the root causes of the disease which will help us to treat patient most accurately. Each etiological factor has its different journey path towards complete outcome of different Parkinsonian symptoms. In each path follows different affected sites of the human body that generate many different types of motor and non-motor symptoms. These combinations of symptoms can help us to choose the proper etiological factor for having Parkinson’s disease. Complete etiological study with all possible symptoms is very much helpful in proper diagnosis of PD even in early stages also. Besides this knowledge of different causing factor of having PD also help in choosing proper medication, or other therapy, that exactly fits with the detected etiological factor. As we know that neurodegenerative disease like PD, cannot be cured completely, so proper early detection may help us to prevent in spreading this deadly disease furthermore.
Conflict of Interest
There is no conflict of interest.
Funding Source
There is no funding source.
Reference
- Cacabelos, R., Parkinson’s Disease: From Pathogenesis to Pharmacogenomics. International journal of molecular sciences, 2017. 18(3): p. 551.
CrossRef - Parkinson’s Disease Statistics, in Parkinsons News Today. 2019, BioNews Services, LLC.
- Understanding Parkinson’s Statistics. [cited 2019 Apr 04]; Available from: https://parkinson.org/ Understanding-Parkinsons/Statistics.
- Marras, C., et al., Prevalence of Parkinson’s disease across North America. npj Parkinson’s Disease, 2018. 4(1): p. 21.
- Gupta, B. and A. Bala, Parkinson’s disease in India: An analysis of publications output during 2002-2011. International Journal of Nutrition, Pharmacology, Neurological Diseases, 2013. 3(3): p. 254-262.
CrossRef - Parkinson’s Disease. [cited 2019 Apr 04]; Available from: http://www.viartis.net/parkinsons.disease/.
- Kalia, L.V. and A.E. Lang, Parkinson’s disease. The Lancet, 2015. 386(9996): p. 896-912.
CrossRef - Calne, D.B., Is “Parkinson’s disease” one disease? Journal of neurology, neurosurgery, and psychiatry, 1989. Suppl(Suppl): p. 18-21.
CrossRef - Chen, Y., et al., The involvement of secondary neuronal damage in the development of neuropsychiatric disorders following brain insults. Frontiers in neurology, 2014. 5: p. 22.
CrossRef - Parkinson, J., An Essay on the Shaking Palsy (London: Sherwood, Neely and Jones). 1817.
- Charcot, J., Lectures of the Diseases of the Nervous System, translated by G. Sigerson, London, The New Sydenham Society, 1881.
- McDonald, C., et al., 200 Years of Parkinson’s disease: what have we learnt from James Parkinson? Age and Ageing, 2018. 47(2): p. 209-214.
CrossRef - Goetz, C.G., The history of Parkinson’s disease: early clinical descriptions and neurological therapies. Cold Spring Harbor perspectives in medicine, 2011. 1(1): p. a008862.
CrossRef - Gowers, W.R., A Manual of Diseases of the Nervous System: Diseases of the Spinal Cord and Nerves. The Journal of Nervous and Mental Disease, 1887. 14(2): p. 123-125.
CrossRef - Richer, P. and H. Meige, Etude morphologique sur la maladie de Parkinson. Nouvelle iconographie de la Salpêtriere, 1895. 8: p. 361-371.
- Ruiz-Gómez, N., The ‘scientific artworks’ of Doctor Paul Richer. Medical Humanities, 2013. 39(1): p. 4-10.
CrossRef - Horsley, V. and R.H. Clarke, The structure and functions of the cerebellum examined by a new method. Brain, 1908. 31(1): p. 45-124.
CrossRef - Willige, H., über paralysis agitans im jugendlichen alter. Zeitschrift für die gesamte Neurologie und Psychiatrie, 1911. 4(1): p. 520.
CrossRef - Meyers, R., The modification of alternating tremors, rigidity and festination by surgery of the basal ganglia. Research publications-association for research in nervous and mental disease, 1940. 21: p. 602-665.
- Cooper, I.S., Ligation of the anterior choroidal artery for involuntary movements-parkinsonism. The Psychiatric Quarterly, 1953. 27(1): p. 317-319.
CrossRef - Hornykiewicz, O., Dopamine miracle: From brain homogenate to dopamine replacement. Movement Disorders, 2002. 17(3): p. 501-508.
CrossRef - Ehringer, H. and O. Hornykiewicz, Verteilung Von Noradrenalin Und Dopamin (3-Hydroxytyramin) Im Gehirn Des Menschen Und Ihr Verhalten Bei Erkrankungen Des Extrapyramidalen Systems. Klinische Wochenschrift, 1960. 38(24): p. 1236-1239.
CrossRef - Schapira, A.H.V., Etiology of Parkinson’s disease. Neurology, 2006. 66(10 suppl 4): p. S10-S23.
CrossRef - Mosley, A.D., R. D.S.;, and A. Samii, The Encyclopedia of Parkinson’s Disease (Facts on File Library of Health and Living). 2nd ed. 2009: Infobase Publishing.
- Pierce, S.E., et al., Parkinson’s disease genetic risk in a midbrain neuronal cell line. Neurobiol Dis, 2018. 114: p. 53-64.
CrossRef - Perry, T.L., D.V. Godin, and S. Hansen, Parkinson’s disease: a disorder due to nigral glutathione deficiency? Neurosci Lett, 1982. 33(3): p. 305-310.
CrossRef - Smeyne, M. and R.J. Smeyne, Glutathione metabolism and Parkinson’s disease. Free radical biology & medicine, 2013. 62: p. 13-25.
CrossRef - Sian, J., et al., Alterations in glutathione levels in Parkinson’s disease and other neurodegenerative disorders affecting basal ganglia. Ann Neurol, 1994. 36(3): p. 348-55.
CrossRef - Reeve, A.K., K.J. Krishnan, and D. Turnbull, Mitochondrial DNA mutations in disease, aging, and neurodegeneration. Ann N Y Acad Sci, 2008. 1147: p. 21-9.
CrossRef - Moon, H.E. and S.H. Paek, Mitochondrial Dysfunction in Parkinson’s Disease. Experimental neurobiology, 2015. 24(2): p. 103-116.
CrossRef - Klein, C. and A. Westenberger, Genetics of Parkinson’s disease. Cold Spring Harbor perspectives in medicine, 2012. 2(1): p. a008888.
CrossRef - Puschmann, A., Monogenic Parkinson’s disease and parkinsonism: clinical phenotypes and frequencies of known mutations. Parkinsonism Relat Disord, 2013. 19(4): p. 407-15
CrossRef. - van Kessel, S.P. and S. El Aidy, Bacterial Metabolites Mirror Altered Gut Microbiota Composition in Patients with Parkinson’s Disease. Journal of Parkinson’s disease, 2019. 9(s2): p. S359-S370.
CrossRef - Ilie, O.-D., et al., Minireview on the Relations between Gut Microflora and Parkinson’s Disease: Further Biochemical (Oxidative Stress), Inflammatory, and Neurological Particularities. Oxidative Medicine and Cellular Longevity, 2020. 2020: p. 4518023.
CrossRef - Weis, S., et al., Effect of Parkinson’s disease and related medications on the composition of the fecal bacterial microbiota. npj Parkinson’s Disease, 2019. 5(1): p. 28.
CrossRef - Jankovic, J. and E. Tolosa, Parkinson’s disease and movement disorders. 2007: Lippincott Williams & Wilkins.
- Manning-Bog, A.B., et al., The herbicide paraquat causes up-regulation and aggregation of alpha-synuclein in mice: paraquat and alpha-synuclein. J Biol Chem, 2002. 277(3): p. 1641-1644.
CrossRef - Betarbet, R., et al., Chronic systemic pesticide exposure reproduces features of Parkinson’s disease. Nat Neurosci, 2000. 3(12): p. 1301-6.
CrossRef - Kotagal, V., Is PIGD a legitimate motor subtype in Parkinson disease? Annals of clinical and translational neurology, 2016. 3(6): p. 473-477.
CrossRef - Knierim, J., Neuroscience Online Chapter 6: Disorders of the Motor System. 1997, The University of Texas Health Science Center at Houston.
- Cubo, E. and C.G. Goetz, Akinesia, in Encyclopedia of the Neurological Sciences (Second Edition), M.J. Aminoff and R.B. Daroff, Editors. 2014, Academic Press: Oxford. p. 102.
CrossRef - Jankovic, J., Parkinson’s disease: clinical features and diagnosis. Journal of Neurology, Neurosurgery & Psychiatry, 2008. 79(4): p. 368.
CrossRef - Giladi, N., et al., Freezing of gait in patients with advanced Parkinson’s disease. Journal of Neural Transmission, 2001. 108(1): p. 53-61.
CrossRef - Lai, D.T.H., M. Palaniswami, and R. Begg, Healthcare sensor networks: challenges toward practical implementation. 2011: CRC Press.
- Johns, P., Clinical neuroscience: an illustrated colour text. 2014: Elsevier Health Sciences.
- Giladi, N., et al., Gait festination in Parkinson’s disease. Parkinsonism & Related Disorders, 2001. 7(2): p. 135-138.
CrossRef - Ou, R., et al., Festination in Chinese patients with Parkinson’s disease. Clinical Neurology and Neurosurgery, 2015. 139: p. 172-176.
CrossRef - Aquino, C.C., E. Slow, and A.E. Lang, Dystonic Pseudo Foot Drop. Movement disorders clinical practice, 2015. 2(3): p. 295-298.
CrossRef - Berardelli, A., et al., Pathophysiology of bradykinesia in Parkinson’s disease. Brain, 2001. 124(Pt 11): p. 2131-46.
CrossRef - Chapuis, S., et al., Impact of the motor complications of Parkinson’s disease on the quality of life. Movement Disorders, 2005. 20(2): p. 224-230.
CrossRef - Popa, L. and P. Taylor, Functional electrical stimulation may reduce bradykinesia in Parkinson’s disease: A feasibility study. Journal of Rehabilitation and Assistive Technologies Engineering, 2015.
CrossRef - van Hilten, J.J., et al., Bradykinesia and hypokinesia in Parkinson’s disease: what’s in a name? Journal of Neural Transmission, 1998. 105(2): p. 229-237.
CrossRef - Ricciardi, L., et al., Rehabilitation of hypomimia in Parkinson’s disease: a feasibility study of two different approaches. Neurological Sciences, 2016. 37(3): p. 431-436.
CrossRef - Fereshtehnejad, S.-M., Ö. Skogar, and J. Lökk, Evolution of Orofacial Symptoms and Disease Progression in Idiopathic Parkinson’s Disease: Longitudinal Data from the Jönköping Parkinson Registry. Parkinson’s disease, 2017. 2017: p. 8.
CrossRef - Cooper, R.M. and S. Khan, Chapter 50 – Extubation and Reintubation of the Difficult Airway, in Benumof and Hagberg’s Airway Management (Third Edition), C.A. Hagberg, Editor. 2013, W.B. Saunders: Philadelphia. p. 1018-1046.e7.
CrossRef - Berke, G.S., et al., Treatment of Parkinson Hypophonia With Percutaneous Collagen Augmentation. The Laryngoscope, 1999. 109(8): p. 1295-1299.
CrossRef - Tjaden, K., Speech and Swallowing in Parkinson’s Disease. Topics in geriatric rehabilitation, 2008. 24(2): p. 115-126.
CrossRef - Pinto, S., et al., Dysarthria in individuals with Parkinson’s disease: a protocol for a binational, cross-sectional, case-controlled study in French and European Portuguese (FraLusoPark). BMJ open, 2016. 6(11): p. e012885-e012885.
CrossRef - Tolosa, E. and Y. Compta, Dystonia in Parkinson’s disease. Journal of Neurology, 2006. 253(7): p. vii7-vii13.
CrossRef - Kim, S.D., et al., Postural Instability in Patients with Parkinson’s Disease. CNS Drugs, 2013. 27(2): p. 97-112.
CrossRef - Bloem, B.R., Postural instability in Parkinson’s disease. Clinical Neurology and Neurosurgery, 1992. 94: p. 41-45.
CrossRef - Berardelli, A., A.F. Sabra, and M. Hallett, Physiological mechanisms of rigidity in Parkinson’s disease. Journal of neurology, neurosurgery, and psychiatry, 1983. 46(1): p. 45-53.
CrossRef - Baradaran, N., et al., Parkinson’s disease rigidity: relation to brain connectivity and motor performance. Frontiers in neurology, 2013. 4: p. 67-67.
CrossRef - Tarakad, A. and J. Jankovic, Essential Tremor and Parkinson’s Disease: Exploring the Relationship. Tremor and other hyperkinetic movements (New York, N.Y.), 2019. 8: p. 589-589.
CrossRef - Deuschl, G., et al., The pathophysiology of parkinsonian tremor: a review. Journal of Neurology, 2000. 247(5): p. V33-V48.
CrossRef - Onanong, J., J. Priya, and B. Roongroj, Pathophysiology of parkinsonian tremor: a focused narrative review. Asian Biomedicine, 2017. 10(s1): p. s15-s22.
- Liaison, O.o.C.a.P. Tremor Fact Sheet. 2018 2019 Jul 06 [cited 2019 Apr 04]; Available from: https://www.ninds.nih.gov/Disorders/Patient-Caregiver-Education/Fact-Sheets/Tremor-Fact-Sheet.
- Kumar, H. and M. Jog, A patient with tremor, part 1: making the diagnosis. CMAJ : Canadian Medical Association journal = journal de l’Association medicale canadienne, 2011. 183(13): p. 1507-10.
CrossRef - Bain, P.G., The management of tremor. Journal of Neurology, Neurosurgery, and Psychiatry, 2002. 72(suppl 1): p. i3.
CrossRef - Fahn, S., J. Jankovic, and M. Hallett, Chapter 18 – Tremors, in Principles and Practice of Movement Disorders (Second Edition), S. Fahn, J. Jankovic, and M. Hallett, Editors. 2011, W.B. Saunders: Edinburgh. p. 389-414.
CrossRef - Thenganatt, M.A. and E.D. Louis, Distinguishing essential tremor from Parkinson’s disease: bedside tests and laboratory evaluations. Expert review of neurotherapeutics, 2012. 12(6): p. 687-696.
- Banou, E. Kinesia Paradoxa: A Challenging Parkinson’s Phenomenon for Simulation. in GeNeDis 2014. 2015. Cham: Springer International Publishing.
CrossRef - Bach-y-Rita, P., Brain plasticity as a basis of the development of rehabilitation procedures for hemiplegia. Scandinavian Journal of Rehabilitation Medicine, 1981. 13(2-3): p. 73.
- Bloem, B.R., J.A. Steijns, and B.C. Smits-Engelsman, An update on falls. Current opinion in neurology, 2003. 16(1): p. 15-26.
CrossRef - Wood, B.H., et al., Incidence and prediction of falls in Parkinson’s disease: a prospective multidisciplinary study. Journal of neurology, neurosurgery, and psychiatry, 2002. 72(6): p. 721-725.
CrossRef - Stacy, M., Nonmotor symptoms in Parkinson’s disease. Int J Neurosci, 2011. 121 Suppl 2: p. 9-17.
CrossRef - Aarsland, D., et al., Frequency of dementia in Parkinson disease. Archives of Neurology, 1996. 53(6): p. 538-542.
CrossRef - Ceravolo, R., et al., The epidemiology and clinical manifestations of dysexecutive syndrome in Parkinson’s disease. Frontiers in neurology, 2012. 3: p. 159.
CrossRef - Chen, J.J. and L. Marsh, Anxiety in Parkinson’s disease: identification and management. Therapeutic advances in neurological disorders, 2014. 7(1): p. 52-59.
CrossRef - Schapira, A.H., Sleep attacks (sleep episodes) with pergolide. The Lancet, 2000. 355(9212): p. 1332-1333.
CrossRef - Zesiewicz, T.A., et al., Autonomic Nervous System Dysfunction in Parkinson’s Disease. Curr Treat Options Neurol, 2003. 5(2): p. 149-160.
CrossRef








