Manuscript accepted on :30-Sep-2020
Published online on: --
Plagiarism Check: Yes
Reviewed by: Nithesh Naik
Second Review by: Victor B Oti
Final Approval by: Dr Patorn Piromchai
Tiffani Shavira Arnetha1, Bethy Suryawathy Hernowo2, Melia Juwita Adha3 and Andri Rezano4*
1Faculty of Medicine, Universitas Padjadjaran, Sumedang, Indonesia, 45363.
2Department of Anatomic Pathology, Faculty of Medicine, Universitas Padjadjaran/ Hasan Sadikin General Hospital, Bandung, Indonesia, 40161.
3Department of Obstetrics and Gynecology, Faculty of Medicine, Universitas Padjadjaran/Hasan Sadikin Hospital, Bandung, Indonesia, 40161.
4Department of Biomedical Sciences, Division of Cell Biology, Faculty of Medicine Universitas Padjadjaran, Sumedang, Indonesia, 45363.
Corresponding Author E-mail: andri.rezano@unpad.ac.id
DOI : https://dx.doi.org/10.13005/bpj/2028
Abstract
Breast cancer is a complex disease that encompasses various kinds of molecular subtypes with heterogeneous characteristics for each type. More information is needed to guide treatment decisions. This study aims to estimate the prevalence of breast cancer subtypes and to determine the relationship between molecular subtypes and overall survival (OS) for breast cancer patients. Retrospective analysis was conducted to examine 468 breast cancer cases diagnosed from January 2011 to September 2011 and had a radical mastectomy at Hasan Sadikin General Hospital Bandung. Age, clinical staging, and molecular subtypes were analyzed on 63 patients from medical records. The patient’s conditions were followed up within five years. Molecular subtypes of breast cancer were divided into luminal A, luminal B, HER2, and triple-negative based on receptor characteristics. Patient OS was measured by Kaplan-Meier analysis and the Log-rank test to estimate outcome differences among subtypes. Luminal A (46%) subtypes were the most prevalent, followed by HER2 (27%), triple-negative (14,3%), and luminal B (12,7%). These tumors were commonly found in women above 40 years old. OS analysis showed a significant difference between subtypes. Luminal A and triple-negative tumors were associated with good and worse prognosis respectively. In conclusion, information on molecular classification in breast cancer patients was necessary for estimating treatment implications and breast cancer patient prognosis.
Keywords
Breast Cancer; Molecular Classification; Therapeutic Response; Receptor Characteristics; Patient Outcome.
Download this article as:| Copy the following to cite this article: Arnetha T. S, Hernowo B. S, Adha M. J, Rezano4 A. Relationship Between Molecular Subtypes and Overall Survival of Breast Cancer in Bandung. Biomed Pharmacol J 2020;13(3). |
| Copy the following to cite this URL: Arnetha T. S, Hernowo B. S, Adha M. J, Rezano4 A. Relationship Between Molecular Subtypes and Overall Survival of Breast Cancer in Bandung. Biomed Pharmacol J 2020;13(3). Available from: https://bit.ly/342XHEE |
Introduction
Breast cancer is a malignant proliferation of epithelial covering ductus or lobules of the breast. It develops through a multistep process including genetic alteration, and the pathogenesis of this disease has not yet been elucidated.1 Amount of breast cancer patients is increasing every year, including in Indonesia.2 Breast cancer incidence rates are 42 per 100.000 Indonesian female population.2 According to Riskesdas 2013, West Java was ranked as the third-highest breast cancer incidence rates, counted 6,701 cases per year.3 However, it nonetheless represents a significant fraction of cancer-related death in women.
Currently, people have more options for breast cancer treatment, while biological prevention has been recently developed to improve patients’ quality of life. Clinicians use St Gallen breast cancer guidelines to determine the management of early breast cancer. It incorporates tumor size, histological grade, vascular invasion, and lymph node status.
Initially, breast cancer phenotypes were investigated using the loss of heterozygosity analysis at a molecular basis to indicate tumor suppressor gene inactivation.4 Then, it was followed identification of key genomic loses, gains, and amplified loci in breast cancer, suggesting the early framework for molecular classification, including low grade and high grade.5
Early diagnosis can lead to a good prognosis. In some developed countries, the five-year survival rates of breast cancer patients are above 80% due to early detection.1 Breast cancer prognosis had a close relation to the survival rate. Generally, the overall survival (OS) rate is measured within five years starting from the first year of diagnosis.
In this recent decade, there has been a new grouping method for breast cancer by molecular analysis. This method could help to estimate the therapeutic response and patient’s prognosis.6,7 Molecular subtypes of breast cancer could be grouped based on the status of estrogen receptor, progesterone receptor, expression of Human Epidermal Receptor (HER2), and index of Ki-67. This method at least has identified 4 groups: luminal A, luminal B, HER2, and triple-negative.8 According to biomolecular profile, luminal A has the best prognosis and triple-negative has the worst prognosis.9
Related to the issue, Indonesia especially Hasan Sadikin General Hospital which is chosen as a referred hospital in West Java have not had specific data about the distribution of breast cancer patients based on molecular subtypes and the relationship between molecular classification of breast cancer and five-year OS rates. Therefore, this study aims to determine the relationship between the molecular subtypes of breast cancer and OS in Hasan Sadikin General Hospital, Bandung.
Material and methods
The study was an analytical retrospective cohort study that used medical records of breast cancer patients in Surgery Department Hasan Sadikin General Hospital in January until September 2011. The patient’s conditions were followed up until September 2016. Molecular classifications were obtained from immunohistochemical examination and categorized as follows: luminal A (ER+ and/or PR+, HER2-), luminal B (ER+ and/or PR+, HER2+/-, Ki-67 >20%), HER2 (ER-, PR-, and HER2+), and triple-negative (ER-, PR-, HER2-).10
Data collections were obtained from medical records of inpatient and outpatient care Hasan Sadikin General Hospital. We selected patients diagnosed with breast cancer during from January to September 2011 and had a radical mastectomy. Molecular subtypes were categorized by the result of the immunohistochemical examination in the Anatomic Pathology Department. Besides, age, stadium, molecular type, last month inpatient care/follow up, and the last condition (alive/dead) were recorded. Patients who did not undergo any follow up control to the hospital were contacted by phone. Unreachable patients would be defined as out of observation (censor) and recorded based on the last month of the hospital visit.
Data analysis was carried out using SPSS for Windows 22nd version. Univariate analysis was performed to observe frequency distribution and proportion from each variable. Bivariate analysis was performed to see the relationship between the dependent variable (OS rates) and the independent variable (molecular classification). Patient OS was measured by the Kaplan-Meier method and verified by the log-rank test as our previous study conducted.6 A value of p <0.05 was considered a statistically significant relationship. Ethical clearance of this study was obtained from the Health Research Ethics Committee Faculty of Medicine Universitas Padjadjaran (No. 526/UN6.C1.3.2/KEPK/PN/2016).
Results and Discussions
Four hundred and sixty-eight breast cancer cases were examined using the Kaplan-Meier method. Among these cases, 405 cases were excluded because of incomplete medical record status. Therefore, 63 cases were included in this study. Of 63 cases, there were 17 cases died during the length of observation.
Table 1: Characteristics distribution of breast cancer patients
| Characteristics | Frequency (n) | Percentage (%) | Dead |
| Age | |||
| – ˂ 40 | 9 | 14.3 | 2 |
| – ≥ 40 | 54 | 85.7 | 15 |
| Stadium | |||
| – I | 2 | 3.2 | 0 |
| – IIA | 9 | 14.3 | 2 |
| – IIB | 15 | 23.8 | 1 |
| – IIIA | 18 | 28.6 | 2 |
| – IIIB | 14 | 22.2 | 8 |
| – IIIC | 4 | 6.3 | 3 |
| – IV | 1 | 1.6 | 1 |
| Molecular Subtypes | |||
| – Luminal A | 29 | 46 | 5 |
| – Luminal B | 8 | 12.7 | 1 |
| – HER2 | 17 | 27 | 5 |
| – Triple negative | 9 | 14.3 | 6 |
As seen in Table 1, most breast cancer patients ages are ≥ 40 years old (85.7%). The oldest age is 72 years old and the youngest age is 27 years old. The average age of patients at diagnosis is 48.79 years old. Most patients (28.6%) come to the hospital with an advanced stadium (IIIA).
An Immunohistochemical record at Anatomic Pathology Department showed that luminal A had the highest percentage of cases (46%), followed by HER2 (27%), and triple-negative (14.3%), and luminal B (12.7%). According to the clinical stadium, luminal A represented the highest percentage of cases with stadium IIB, luminal B had a higher percentage with stadium IIB dan IIIA, HER2 had a higher percentage with stadium IIIA and triple-negative had a higher percentage with stadium IIIB. The characteristic distribution of breast cancer patients and its prevalence toward clinical status could be seen in Table 2.
Table 2: Prevalence of molecular classifications and clinical stadium
| Characteristics | Luminal A | Luminal B | HER2 | Triple-Negative |
| Age | ||||
| – ˂ 40 | 6.3% | 0% | 3.2% | 4.8% |
| – ≥ 40 | 39.7% | 12.7% | 23.8% | 9.5% |
| Stadium | ||||
| – I | 1.6% | 1.6% | 0% | 0% |
| – IIA | 9.5% | 3.2% | 0% | 1.6% |
| – IIB | 14.3% | 3.2% | 4.8% | 1.6% |
| – IIIA | 9.5% | 3.2% | 12.7% | 3.2% |
| – IIIB | 9.5% | 1.6% | 4.8% | 6.3% |
| – IIIC | 1.6% | 0% | 3.2% | 1.6% |
| – IV | 0% | 0% | 1.6% | 0% |
We observed that 17 patients died during follow up: 35% out of 17 cases belonging to triple-negative type, 29.4% HER2 and luminal-A type, and 5.8% luminal-B type. Kaplan Meier curves in Figure 1 showed that luminal A was associated with the highest survival rates (76.8%) whilst triple negative was associated with the lowest survival rates (15%). Luminal B was associated with a better survival rate (66.7%) than HER2 (61.6%). Luminal A had the highest average survival months among other molecular types (respectively, Luminal A=53.84 months, Luminal B=53 months, HER2=34.59 months, triple negative=21.95 months). The log-rank test showed there were statistically significant differences in survival among four molecular subtypes (p=0.001).
Table 3: Five-year OS rates of breast cancer patients based on molecular classification
| Five-year survival rates analysis | Luminal A | Luminal B | HER2 | Triple-Negative |
| Five-year survival rates | 0.768 | 0.667 | 0.616 | 0.150 |
| Average survival (months) | 53.840 | 53.000 | 34.590 | 21.950 |
| p | 0.001 | |||
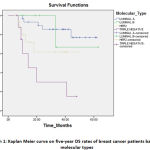 |
Graph 1: Kaplan Meier curve on five-year OS rates of breast cancer patients based on molecular types |
Molecular classifications of breast cancer have become an essential indicator in estimating prognosis and selection of therapy. This is the first study in Indonesia which analyzed five-year survival rates based on molecular subtypes. This study result is appropriate with St. Gallen International Expert Consensus in 2009 which confirmed the use of ER, PR, HER2, and Ki-67 as biomarkers to define a molecular subtype of breast cancer.11
In this study, luminal A is the predominant molecular type compared to other molecular types (respectively, luminal A 46%, HER2 27%, triple-negative 14.3%, and luminal B 12.7%). This result is similar but a little bit lower than reported by Zhang (60.8%).12 Several studies had a different sequence in the distribution of molecular subtypes. Bennis, et al reported that luminal A is the highest percentage of cases (53.6%) followed by luminal B (16.4%), HER2 (12.6%), and triple-negative (12.6%). This could be due to the amount of sample, incomplete data, and other factors that may contribute to the result of each study.
In term of five-year survival rates, luminal A had the highest survival probability whilst triple-negative had the lowest survival probability compared to other molecular types (respectively, luminal A (76.8%), luminal B (66.7%), HER2 (61.6%), and triple-negative (15%). Puig vives, et al observed a higher probability of five-year survival (luminal A: 91.5%, luminal B: 85.8%, HER2: 78.6%, and triple-negative: 76.3%).13 Higher degree of healthcare service, economical status, and women awareness could be the reason of this difference results.
Luminal A and B types were known for expressing ER and PR biomarkers. Breast cancer that had hormone overexpression like luminal A and luminal B had a higher survival rate compared to non-hormonal overexpression. This could be explained because they were responsive toward endocrine therapy such as tamoxifen and aromatase inhibitor.14 Proliferation rate of luminal A type is lower than luminal B since luminal B has higher Ki-67 index (>20%). Therefore, luminal B has a higher mortality rate than luminal A. This result is similar to most molecular breast cancer studies.15,16
Furthermore, overexpression and amplification of HER2 reported reaching 20-30% in the population.17 This is similar to our study result (27%). HER2 overexpression is linked to a higher degree of the histopathological result, bigger tumor size, lymph node metastasis, higher relapse probability, and lower survival rate. In this study, HER2 had a lower percentage of survival rate compared to the Luminal type. This could be happened due to overexpression of HER2 enhance proliferation, angiogenesis, and angioinvasion of cancer cells.18
Triple-negative is characterized by negative expression of ER/PR and HER2. This type has a lower response rate towards endocrine therapy (taxane) and therapeutical target (trastuzumab). This type had a higher sensitivity using chemotherapy. Our study result observed that triple-negative had the lowest survival probability than other molecular types (15%). CK5/6 overexpression, mutation of Ki-67, p53, and NF-κB cause a higher proliferation rate, uncommon metastasis pattern, and worse prognosis. Hereditary factor-like BRCA1 mutation was also known to make this type have lower survival rate.19
The log-rank test showed there were statistically significant differences in survival among four molecular subtypes (p=0.001). This may be explained because each molecular type showed different characteristics not only clinically but also in the molecular sequence of cancer biology.
The limitation of this study is incomplete medical records. This triggers difficulty in determining molecular types, therapy regiment assessment, and patient follow up. Therefore it is advisable to fill the medical record completely and clearly to facilitate further research.
Molecular analysis using immunohistochemical examination could explain the heterogenicity of breast cancer in molecular sequence, so it could be used to assess prognosis and therapy accurately and specifically.
Conclusion
There is a significant relationship between molecular classifications of breast cancer and five-year OS rates. Thus, this study recommends a combination of breast cancer molecular analysis and clinicopathological status to assess the prognosis of patients accurately and specifically.
Acknowledgment
The authors would like to express gratitude for all staff of the Department of Anatomic Pathology, Faculty of Medicine, Universitas Padjadjaran/Hasan Sadikin General Hospital, and also all staff of Medical Record Installation, Hasan Sadikin General Hospital for their help to accomplish this project.
Funding Source
This work was supported by independent source of funding.
Conflict of Interest
There is no conflict of interest existed.
References
- Sun YS, Zhao Z, Yang ZN, et al. Risk factors and prevention of breast cancer. Int J Biol Sci. 2017;13(11):1387-97.
- International Agency for Research on Cancer (IARC)/WHO. GLOBOCAN 2018: Estimated cancer incidence, mortality, and prevalence in Indonesia in 2018. 2018. [cited 2020 June 7]. Available from: https://gco.iarc.fr/today/online-analysis-map?v=2018&mode=population&mode_population=continents&population=900&populations=900&key=asr&sex=2&cancer=20&type=0&statistic=5&prevalence=0&population_group=0&ages_group%5B%5D=0&ages_group%5B%5D=17&nb_items=10&group_cancer=1&include_nmsc=1&include_nmsc_other=1&projection=natural-earth&color_palette=default&map_scale=quantile&map_nb_colors=5&continent=4&rotate=%255Bnull%252Cnull%252C0%255D.
- Pusat Data dan Informasi. Situasi Penyakit Kanker. Buletin Jendela Data dan Informasi Kesehatan. 2015;1:8-9.
- Reis-Filho JS, Simpson PT, Gale T, Lakhani SR. The molecular genetics of breast cancer: the contribution of comparative genomic hybrid- ization. Pathol Res Pract 2005; 201: 713e25.
- Simpson PT, Reis-Filho JS, Gale T, Lakhani SR. Molecular evolution of breast cancer. J Pathol 2005; 205: 248e54.
- Rezano A, Kuwahara K, Yamamoto-Ibusuki M, Kitabatake M, Molthiya P, Phimsen S, et al. Breast cancers with high DSS1 expression that potentially maintains BRCA2 stability have poor prognosis in the relapse-free survival. BMC Cancer. 2013;13:562
- Rezano A, Pan CE, Istiqomah AA, Zada A. Association of Ki-67 expression and response of neoadjuvant chemotherapy in invasive breast cancer patients in Bandung. Int J Integr Health Sci. 2018;6(2):80-3.
- Eroles P, Bosch A, Fidalgo JAP, Lluch A. Molecular biology in breast cancer: intrinsic subtypes and signaling pathways. Cancer Treat Rev. 2012;38(6):698–707.
- Alizart M, Saunus J, Cummings M, Lakhani SR. Molecular classification of breast carcinoma. Diagnostic Histopathology. 2012;18(3):97–103.
- Tashima R, Nishimura R, Osako T, Nishiyama Y, Okumura Y, Nakano M, et al. Evaluation of an optimal cut-off point for the Ki-67 index as a prognostic factor in primary breast cancer: a retrospective study. PLoS ONE. 2015;10(7):e0119565.
- Harbeck N, Thomssen C, Gnant M. Gallen 2013: Brief Preliminary Summary of the Consensus Discussion. Breast Care. 2013;8(2):102–109.
- Zhang HM, Zhang BN, Xuan LX, Zhao P. Clinical characteristics and survival in the operable breast cancer patients with different molecular subtypes. Chinese Journal of Oncology. 2009;31(6):447–51.
- Puig-Vives M, Sánchez MJ, Sánchez-Cantalejo J, Torrella-Ramos A, Martos C, Ardanaz E, et al. Distribution and prognosis of molecular breast cancer subtypes defined by immunohistochemical biomarkers in a Spanish population-based study. Gynecol Oncol. 2013;130(3):609–
- Schnitt SJ. Classification and prognosis of invasive breast cancer: from morphology to molecular taxonomy. Mod Pathol. 2010;23(2):60–
- Hennigs A, Riedel F, Gondos A, Sinn P, Schirmacher P, Marmé F, et al. Prognosis of breast cancer molecular subtypes in routine clinical care: a large prospective cohort study. BMC Cancer. 2016;16(1):734.
- Bao P, Peng P, Gu K, Wu C, Huang Z, Gong Y, et al. Long-term survival analysis of different breast cancer molecular subtypes : Shanghai Breast Cancer Survival Study. Chinese Journal of Surgery. 2015;53(12):928–
- Bennis S, Abbass F, Akasbi Y, Znati K, Joutei KA, El Mesbahi O, et al. Prevalence of molecular subtypes and prognosis of invasive breast cancer in north-east of Morocco: retrospective study. BMC Research Notes. 2012;5(1):436.
- Bhattacharjee RN, Timoshenko AV, Cai J, Lala PK. Relationship between cyclooxygenase-2 and human epidermal growth factor receptor 2 in vascular endothelial growth factor c up-regulation and lymphangiogenesis in human breast cancer. Cancer Sci. 2010;101(9):2026–
- Ossovskaya V, Wang Y, Budoff A, Xu Q, Lituev A, Potapova O, et al. Exploring molecular pathways of triple-negative breast cancer. Genes Cancer. 2011;2(9):870–







