Shanti Gurung1, Navin Patil2, Karthik Rao3, Gunjan Chaudhary4*, Mohsin Nazeer5, George M Varghese5, Ram Bhutani5 and Amrita Parida6
1Pharmacology, Universal College of Medical Sciences, Bhairahawa, Nepal.
2Pharmacology, Universal College of Medical Sciences, Bhairahawa, Nepal.
3Medicine, KS Hegde Medical Academy , Mangalore, India.
4Anesthesia, Kalpana Chawla Medical College, Karnal, Haryana, India.
5Kasturba Medical College, Manipal , MAHE India.
6Pharmacology, Kasturba Medical College, Manipal, MAHE India.
Corresponding Author E-mail: navin903@gmail.com
DOI : https://dx.doi.org/10.13005/bpj/2016
Abstract
Comparing the efficacy of doxycycline and azithromycin in the treatment of patients with acne vulgaris. A total of 110 patients with acne vulgaris participated in this comparative, prospective, longitudinal study and were randomly assigned to two groups (azithromycin and doxycycline). Grading of scores were determined and recorded at baseline using the sign and symptom scores validated by Jerry KL Tan whereas the severity of acne was evaluated by counting the number of lesions. Patients were followed up for a period of 4 weeks. Clinical assessment was made at the end of 4 weeks and data was analysed. Pre and post treatment evaluations were done by using score scale where the number of non-inflammatory, inflammatory and total lesions were counted. Chi-square test was used to compare the results and p < 0.05 was considered to be statistical significant. The mean age group of the participants was 21.26 (SD=5.94) years. In both the study groups, the female participants outnumbered males and the male:female ratio was 1:3. With respect to the participants receiving Azithromycin, the percentage and severity of non-inflammatory lesions, in the mild category was 60% in the post treatment as compared to 40% in the pretreatment group which reveals positive outcome post treatment to Azithromycin. Similarly, in Doxycycline treated group, the percentage and severity of non- inflammatory lesions, in mild category was 63.6% in the post treatment as compared to 32.7% in the pretreatment group which reveals that there was improvement of approximately 30% case progressed from moderate to mild category. However, no statistically significant difference (p>0.05) in efficacy was found when the azithromycin treated group was compared with doxycycline treated group after one month of therapy. Both drugs were effective in reducing the severity of Acne vulgaris when compared separately before and after therapy with azithromycin being a little superior in the reduction of the percentage of number of inflammatory lesions than Doxycycline. The reduction in the percentage in the number of inflammatory lesions post 1 month was better with azithromycin group as compared to Doxycycline, whereas there was improvement with respect to the reduction in number of non-inflammatory lesions and total lesions in both groups but was not significant between the groups However, there was no significant difference between the efficacy of Azithromycin and Doxycycline treated group after one month period of therapy.
Keywords
Acne Vulgaris; Azithromycin; Doxycycline
Download this article as:| Copy the following to cite this article: Gurung S, Patil N, Rao K, Chaudhary G, Nazeer M, Varghese G. M, Bhutani R, Parida A. A Comparative Study on Efficacy of Azithromycin and Doxycycline in the Treatment of Acne Vulgaris at a Tertiary Care Centre. Biomed Pharmacol J 2020;13(3). |
| Copy the following to cite this URL: Gurung S, Patil N, Rao K, Chaudhary G, Nazeer M, Varghese G. M, Bhutani R, Parida A. A Comparative Study on Efficacy of Azithromycin and Doxycycline in the Treatment of Acne Vulgaris at a Tertiary Care Centre. Biomed Pharmacol J 2020;13(3). Available from: https://bit.ly/2I0defY |
Introduction
Acne Vulgaris is a chronic inflammatory disorder involving the blockage and/or inflammation of pilosebaceous follicles. It is clinically characterized by comedones, papules, pustules, nodules, cysts and scars. It may have an adverse effect on psychosocial and emotional impact in an individual which may lead to social phobias, withdrawal from society and clinical depression.1
It characteristically presents as non-inflammatory lesions, inflammatory lesions, or a mixture of both affecting mostly the face but sometimes also the back and the chest. A non-inflammatory lesion consists of closed comedones and open comedones. Inflammatory lesion present in the form of erythematous macules, papules and pustules in majority of cases.2
The most common causative organism for acne vulgaris is the anaerobic organism, Propionibacterium acnes (P. acnes). P. acnes is an anaerobic bacteria that can colonize the skin and hair follicles. Several studies have indicated that specific strains of P.acnes are commonly associated with acne vulgaris. P. acnes grows deep inside of the pores, where it feeds on the sebum produced by the sebaceous glands.1
Acne scar is a common complication to acne. It is of different types and is associated with either loss or increase in collagen. Ice pick scars, which are well defined depressed scars with irregular edges, or atrophic macular scars, which have a superficial shallow depression with wrinkled epidermis is associated with loss of collagen. Increase in collagen occurs in either hypertrophic and/or keloids which can be very disfiguring and causes psychosocial abnormalities in an individual.2
The main pathophysiology’s involved in the development of acne are follicular differentiation, excess sebum production, Propionibacterium acnes and inflammation.3
The general therapy in the treatment of acne vulgaris includes oral and topical therapy.[4] Topical therapy includes Benzoyl peroxide, Tretinoin, Azelaic acid. Among these benzoyl peroxide is considered a potent antimicrobial agent against bacteria. Benzoyl peroxide is a lipophilic drug which can easily penetrate stratum corneum and enters the pilosebaceous follicles after which it is rapidly broken down to benzoic acid and hydrogen peroxide and generates free radicals that harms the bacterial protein.5
Oral therapy includes antibiotics such as doxycycline, erythromycin, azithromycin, trimethoprim, etc. Among these, Azithromycin and doxycycline are nowadays used routinely in clinical practice worldwide.6,7
Methoology
Materials
Type of study
Prospective longitudinal study
Site of the study
Department of Dermatology and Venereology, Manipal Teaching Hospital, Pokhara.
Duration of study
One year (September 2016 to September 2017)
Sample size calculation
A prevalence of 80% was taken from the study66
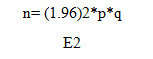
where, n= required sample size
p= prevalence
q= 100-p (when p is in percentage terms)
E= allowable error
Considering 10% dropouts and subjects that will miss follow up, sample size was 107. To increase the accuracy a sample size of 110 was taken for this study.
Selection criteria: All the patients visiting to the dermatology OPD of Manipal Teaching Hospital with the complaints of acne.
Inclusion criteria
All patients diagnosed with acne regardless of age and sex.
Patient who were willing to participate in the study.
Exclusion criteria
Pregnant and lactating women with acne.
The patients who failed to give consent.
Tools
Grading of Acne was done by using the sign and symptom score scale developed and validated by Jerry KL Tan.67
severity of acne was evaluated considering the number of non-inflammatory lesions, inflammatory lesions and total lesions as follows:
Severity was graded as 0(None), 1 (Mild), 2 (Moderate) and 3 (Severe).
Non Inflammatory lesions: 0 (absent), 1 (<20), 2 (20-100) and 3 (>100)
Inflammatory lesions: 0 (absent), 1 (<15), 2 (15-50) and 3 (>50)
Total lesions count: 0 (absent), 1 (<30), 2 (30-125) and 3 (>125).
Total cases were divided into 2 groups, each group contained 55 patients. Patients of Group 1 were given Azithromycin 500mg three times a week for one month and the patients of Group 2 were given Doxycycline 100mg once daily for one month. After a period of 4 weeks, each patients were followed up to evaluate number of non-inflammatory lesions, inflammatory lesions and total lesions count as mentioned above. The efficacy of either drugs were also measured with the efficacy parameters stated above.
Results
Table 1: Demographic characteristics of the study participants
| Study group | Mean | Standard deviation | Minimum age | Maximum age |
| Total sample | 21.26 | 5.94 | 13 | 56 |
| Azithromycin group (n=55) | 20.96 | 4.834 | 13 | 37 |
| Doxycycline group
(n=55) |
21.56 | 6.89 | 14 | 56 |
The mean age of study participants was 21.26 (SD=5.94) years, with the youngest participant being 13 years old and the oldest participant being 56 years old
Age group of the study participants
Table 2: Shows the age distribution of patients where maximum participants (56) belonged to age group of 20-29 years, followed by < 20 years (47). Only 1 participant was of age above 40 years
|
Age groups (Years) |
Frequency (n) | Percentage (%) |
|
< 20 |
47 | 42.72 |
| 20-29 | 56 | 50.90 |
| 30-39 | 6 | 5.45 |
| 40+ | 1 |
0.90 |
| Total | 110 |
100 |
 |
Figure 1: Gender distribution of the study population |
According to gender, there were more female participants comprising of 73 (66.4% ) than males 37 (33.6%)
Table 3: Comparison of clinical characteristics of acne in azithromycin and doxycycline treated groups before treatment and post 1 month of treatment
|
Lesion types |
Azithromycin
(n=55) |
Doxycycline
(n=55) |
P Value | Post 1 month treatment with Azithromycin | Post1 month treatment with Doxycycline | |
| No (%) | No (%) | |||||
| Non inflammatory lesions | 0 (None) | – | – |
.428 |
– | – |
| 1-19 (mild) | 22 (40) | 18 (32.7) | 33(60) | 35(63.6) | ||
| 20-100 (moderate) | 33 (60) | 37 (67.3) | 22(40) | 20(36.4) | ||
| >100 (severe) | – | – | – | – | ||
| Inflammatory lesions | 0 (none) | – | 1 (1.8) |
.444* |
1 | 1(1.8) |
| 1-14 (mild) | 23 (41.8) | 27 (49.1) | 35(63.6) | 33(60) | ||
| 15-50 (moderate) | 32 (58.2) | 27 (49.1) | 19(34.5) | 21(38.2) | ||
| >50 (severe) | – | – | – | – | ||
| Total lesions | 0 (none) | – | – |
.918* |
– | – |
| 1-29 (mild) | 9 (16.4) | 7 (12.7) | 41(74.5) | 43(78.2) | ||
| 30-125 (moderate) | 44 (80) | 46 (83.6) | 13(23.6) | 12(21.8) | ||
| >125 (severe) | 2 (3.6) | 2 (3.6) | 1(1.8) |
– |
||
The reduction in the percentage in the number of inflammatory lesions post 1 month was better with azithromycin group as compared to Doxycycline, whereas there was improvement with respect to the reduction in number of non-inflammatory lesions and total lesions in both groups but was not significant between the groups
Discussion
Acne vulgaris is a self-limiting inflammatory disorder of the pilosebaceous unit,which may run a chronic course. It is triggered by Propionibacterium acnes in adolescence and occurs by hypersensitivity of the sebaceous glands to normal circulating dehydroepiandrosterone (DHEA). It is a common skin disorder which can present with inflammatory and non-inflammatory lesions chiefly on the face but can also occur on the upper arms, trunk, and back. Common triggering factors include medications like Lithium, steroids, anticonvulsants; exposure to sunlight;endocrine disorders like PCOD and pregnancy. Heritability estimates range from 50-90%.8
Topical and oral medications can be used for treatment of acne. P. acnes, which is highly sensitive to a number of antimicrobial agents of different classes, including macrolides, tetracyclines, penicillins, clindamycin, aminoglycosides, cephalosporins, trimethoprim, and sulfonamides.9 Here, we have studied the efficacy of two drugs used routinely in clinical practice worldwide-Azithromycin and Doxycycline.
Azithromycin is a broad-spectrum macrolide antibiotic. It prevents bacteria from growing by interfering with their protein synthesis. It binds reversibly to the 50S subunit of the bacterial ribosome, thus inhibiting translation of mRNA. It is used in the treatment of acne due to its anti-bacterial, immunomodulatory and anti-inflammatory properties. Common side effects include diarrhea, nausea and abdominal pain, palpitations, angina, dyspepsia, flatus, vomiting, melena, jaundice, vaginal monilia, vaginitis, nephritis, dizziness, headache, vertigo, somnolence and fatigue.10
Doxycycline is a broad spectrum semi-synthetic tetracycline. It inhibits bacterial protein synthesis by reversibly binding to the 30S ribosomal subunit and preventing the association of aminoacyl-tRNA with the bacterial ribosome, thereby giving the immune system time to kill and remove the bacteria. Further inhibition of protein synthesis occurs in mitochondria through binding to the 70S ribosomes. Common side effects include nausea, vomiting, diarrhoea, epigastric burning and oesophagitis. Stevens-Johnson syndrome and toxic epidermal necrolysis may occur with the use of doxycycline. The accumulation of doxycycline in teeth and bones leads to discoloration of teeth. It may also cause enamel dysplasia, bone deformities and impairment in bone growth. It has also been associated with benign intracranial hypertension. 11
Oral antibiotics should be used for the shortest time possible to prevent antibiotic resistance. Studies have found that topical benzoyl peroxide with oral antibiotics may reduce the risk of developing antibiotic resistance.
In this study; improvements were seen, in various parameters assessing lesion severity, in patients with acne receiving both azithromycin and doxycycline separately. The reduction in the percentage in the number of inflammatory lesions post 1 month was better with azithromycin group as compared to Doxycycline, whereas there was improvement with respect to the reduction in number of non-inflammatory lesions and total lesions in both groups but was not significant between the groups The difference in the degree of improvement was, however, not statistically significant (p>0.05) for any of the efficacy parameters when compared with the outcome of Azithromycin treated group Vs. Doxycycline treated group for 1 month time. So the choice of the drug may depend on parameters like cost of drug and side effect profile of the drug rather than its efficacy. However, studies have also shown that the incidence of side effects is lower with azithromycin,12 while compliance is higher in azithromycin due to ease of administration.13
References
- Dawson AL, Dellavalle RP. Acne Vulgaris. BMJ 2013;346
CrossRef - Layton A.M. A review on the treatment of acne vulgaris. Int J Clin Pract 2006; 60(1):64-7
CrossRef - Harper JC. An update on the pathogenesis and management of acne vulgaris. J Am Acad Dermatol 2004; 5136-8.
- Rathi KS. Acne Vulgaris Treatment: The current scenario. IJD 2011;56(1):7-13
CrossRef - Thiboutot D, Gollnick H, Bettoli V, Dréno B, Kang S, Leyden JJ, et al. New insights into the management of acne: an update from the Global Alliance to Improve Outcomes in Acne group. J Am Acad Dermatol.2009; 60(5):1-50
- Harrison PV. A comparison of doxycycline and minocycline in the treatment of acne vulgaris. Clin Exp Dermatol 2003; 139:459–64.
- Bardazzi F, Savoia F, Parente G, Tabanelli M, Balestri R, Spadola G, et al. Azithromycin, a new therapeutic strategy for acne in adolscents. Dermatol Online J 2007; 13:4.
- Motosko CC, Zakhem GA, Pomeranz MK, Hazen A. Acne: a side-effect of masculinizing hormonal therapy in transgender patients. Br. J. Dermatol. 2019 Jan;180(1):26-30.
CrossRef - Katsambas A, Papakonstantinou A. Acne: Systemic Treatment. Clinics in Dermatology, 2004; 22: 412-18.
CrossRef - Scheinfeld NS, Tutrone WD, Torres O, et al. Macrolides in Dermatology. Clinics in Dermatology 2003;21:40-9.
CrossRef - Holmes NE and Charles P. Safety and Efficacy Review of Doxycycline. Clinical Medicine: Therapeutics, 2009;1:471-82
CrossRef - Kus S, Yucelten D, Aytug A. Comparison of efficacy of azithromycin vs. doxycycline in the treatment of acne vulgaris. Clinical and Experimental Dermatology 2005; 30(3):215-20.
CrossRef - Singhi MK, Ghiya BC, Dhabhai RK. Comparison of oral azithromycin pulse with daily doxycycline in the treatment of acne vulgaris. Indian J Dermatolvenereolleprol. 2003; 69(4):274-6.








