Sumathi C Samiappan1* , Rajesh Pandiyan2
, Rajesh Pandiyan2 , Sampathkumar Palanisamy1
, Sampathkumar Palanisamy1 , Sivakumar Ramalingam1
, Sivakumar Ramalingam1 , Renuka Saravanan1
, Renuka Saravanan1 , Sheik Abdulla Hameed1
, Sheik Abdulla Hameed1
1Department of Chemistry and Biosciences, Srinivasa Ramanujan Centre, SASTRA University, Kumbakonam, Tamil Nadu, India. 612001
2Department of Biochemistry, Karpagam University, Coimbatore, Tamil Nadu, India. 641021
Corresponding Author E-mail : sumathi.cs@src.sastra.edu
DOI : https://dx.doi.org/10.13005/bpj/1973
Abstract
The present study intends to study the biofilm forming indwellers of dental braces. Following standard pure culture techniques, twenty-eight strains were isolated and purified. Mostly the isolated colonies were Gram positive cocci and gram negative rod shaped bacteria. In mannitol salt agar (MSA) the golden yellow colour colonies were observed. The six isolates with yellow colour colonies confirms Staphylococcus aureus. Six isolates produced green colour colonies on Cetrimide agar confirmed as Pseudomonas aeruginosa. On blood agar supplemented with 5% sheep blood, nine isolates showed β -hemolysis, three isolates showed α-hemolysis and other isolates showed no hemolysis. All isolates tested were non lactose fermentors. Then the isolates were screened for the biofilm formation and were confirmed by Congo red agar method. Some of the isolates showed black colonies with a dry crystalline consistency which indicated positive for biofilm formation. The biofilm formation was also evaluated qualitatively by tube assay. Totally four isolates produced strong biofilms, six isolates produced moderate biofilm, seven isolates formed weak biofilms. Four isolates with strong biofilm formation chosen for further work. In antibiotic sensitivity test to observe the zone formation. Antibiotic resistance of biofilm forming bacteria was tested. The ethanol extracts of turmeric were separated by thin layer chromatography. Curcumin found as more effective compound when compared to the demethoxy curcumin and bis demethoxy curcumin against biofilm forming bacteria. Similarly, dry ginger extracts were also effective against biofilm forming bacteria. Ginger had more effective inhibition of biofilm formation than turmeric fractions.
Keywords
Antibiotic Resistance; Biofilm Forming Bacteria; Curcumin; Dental Braces; Dry Ginger; Orthodontic Wires
Download this article as:| Copy the following to cite this article: Samiappan S. C, Pandiyan R, Palanisamy S, Ramalingam S, Saravanan R, Hameed S. A. Targeting the Extracellular Polysaccharide Production (EPS) by Biofilm Forming Bacteria from Orthodontic Brackets and Wires Through Antiquorum Sensing Action of Bioactive Compounds from Curcuma longa and Zingiber officinale. Biomed Pharmacol J 2020;13(2). |
| Copy the following to cite this URL: Samiappan S. C, Pandiyan R, Palanisamy S, Ramalingam S, Saravanan R, Hameed S. A. Targeting the Extracellular Polysaccharide Production (EPS) by Biofilm Forming Bacteria from Orthodontic Brackets and Wires Through Antiquorum Sensing Action of Bioactive Compounds from Curcuma longa and Zingiber officinale. Biomed Pharmacol J 2020;13(2). Available from: https://bit.ly/31CcxBj |
Introduction
Biofilm formation by bacteria is a serious issue in health aspects because it is difficult to eliminate and control. The patients under orthodontic treatment with fixed type of dental brackets are loaded with biofilm forming bacteria. Hyperplastic form of gingivitis commonly observed in patients with fixed orthodontic appliances that include the use of brackets (Papaioannou et al., 2012). Single strand or multi strand wires act as habitats for biofilms bacteria (Jongsma et al., 2013). Biofilm formation leads to several problems like gingivitis, white spot lesions, cavities, enamel demineralization and other infectious diseases (Demeling et al., 2009; Ren et al., 2014). Biofilm related complications during orthodontic treatment occur due to several reasons such as resistance towards antibiotics, biocides, surfactants, predators and phagocytosis. It requires high doses (100-1000 times) of antibiotic to kill biofilms than planktonic cells (Merrit et al., 2000). The composition of biofilms includes a hard surface, microbes (inter or intraspecies) and glycocalyx (Dunne et al., 2000). The biofilm forming bacteria produce sticky material consists extracellular polysaccharides, proteins, nucleic acids and lipids. EPS helps bacteria to interact with the environment (Simoes et al., 2010).
Oral biofilm depends on component species, dietary components, oral hygiene, host defense, flushing of saliva etc. (Marsh, 2003). The inhibition of biofilm development including prevention of attachment of Cariogenic bacteria, manipulation of cell signalling mechanisms, delivery of effective antimicrobials or enhancement of the host defense could be the strategies to prevent dental caries (Marsh, 2006). The presence of biofilm bacteria changes the microbial communities of oral cavity. Use of antibiotics regularly or improperly to control infections caused by bacteria is ineffective due to development of microbial resistance towards drugs (Dimopoulus et al., 2013). This mechanism helps bacteria to withstand extreme environmental conditions and drugs. An alternative approach is expected to develop drugs to treat infections caused by drug resistant bacteria.
Plant bioactive compounds are alternative strategy to reduce the virulence nature of infectious pathogens. Plant based molecules are used as base for drug designing and production in pharmaceutical industries. Plant bioactive compounds have antibiofilm potential that are highly safe and no toxic effects (Essawi and Srour, 2000). In the present study, two plants were chosen to control biofilm forming bacteria.
Turmeric (Curcuma longa L.) belongs to aromatic spices. The bioactive compound curcumin, which is extracted from rhizomes of turmeric. It is a well-known compound having many biological potentials and used to treat variety of diseases. The biological activities attributed to curcumin/turmeric include anticancer, anti-inflammatory, anti-oxidant, anti-microbial, anti-angiogenic, neuroprotective, immunomodulatory effects and enhanced wound healing.
Ginger (Zingiber officinale) is one of the most frequently used ingredients in folk medicine and cooking. Ginger extracts showed strong antioxidant (Stoilova et al., 2007), antibacterial, antifungal, anticancer and anti-inflammatory activities (Habib et al., 2008). Essential oils (ethanolic extract) of ginger have been studied for their antimicrobial activity against different bacteria including E.coli, S.typhi (Meliani et al., 2014; Maekawa et al., 2015). Essential oils of ginger have been used for preventing biofilm formation by Pseudomonas aeruginosa PA14 (Kim and Park, 2013), Staphylococcus aureus (Lee et al., 2014), Candida albicans (Agarwal et al., 2008) and Escherichia coli ATCC 25922, but did not show anti biofilm effect against S. typhimurium (Nikolić et al., 2014).
The objective of the present study is to isolate and screen biofilm forming bacteria adhering to the dental brackets. The characterization of the virulence factors and antibiotic resistance of biofilm forming bacteria is quite important. The effort was made to control the biofilm forming bacteria using ethanolic extracts of turmeric and ginger. For approval antibiofilm potentials of curcumin against severe infections caused by biofilm forming bacteria, further comprehensive studies are needed.
Materials and Methods
Sample Collection
Orthodontic brackets and wires were used for isolation of biofilm forming bacteria were collected, transferred into sterile nutrient broth and transferred to the laboratory from 22 healthy individuals. The samples were collected at KSR Institute of Dental science and Research hospital, Tiruchengode, Tamil Nadu, India.
Isolation of Biofilm Forming Bacteria
Using sterile swabs, inoculum was spread onto sterile nutrient agar and incubated at 37°C for 24 hours. The pure bacterial colonies obtained were further sub cultured and maintained in nutrient agar medium at 4˚C for further studies. The microbiological methods were done by following standard pure culture techniques.
Characterization of Biofilm Forming Bacteria
The isolated biofilm forming bacteria was subjected to further characterization. Gram staining and motility tests were performed. Oxidase test was done for identification of the organisms. Based on the gram staining results, the isolates were streaked on to selective and differential media such as Mannitol salt agar (MSA), Cetrimide agar, Mac Conkey agar and Blood agar. Then the inoculated plates were incubated at 37˚C for 24 hours.
Screening of Biofilm Forming Bacteria
Congo Red Agar Method
This method is based on the characteristic cultural morphology of biofilm-forming bacteria on Congo red agar (CRA) medium. The isolates were streaked on the Muller Hinton agar (HIMEDIA) supplemented with 0.8g/l of Congo red dye and incubated for 48 hours at 37°C. The production of black colored colonies with a dry crystalline consistency indicated biofilm formation. Non biofilm forming strains produced red colored colonies, which helps for differentiation from biofilm forming bacteria (Mathur et al., 2006).
Tube Assay
Qualitative assessment of biofilm formation was determined by the tube staining assay (Christensen et al., 1982). Isolates were inoculated in 10ml trypticase soy broth (TSB) with 5% sucrose and incubated for 24 hours at 37°C in static and rotary condition. The tubes were decanted, washed with phosphate buffer saline (PBS) (pH 7.3), dried and stained with 0.1% crystal violet. Excess stain was removed by washing the tubes with deionized water. Formation of biofilm was confirmed with the presence of visible film on the wall and bottom of the tube. However, the liquid interface did not indicate biofilm formation (Mathur et al., 2006).
Antibiotic Sensitivity Test
Biofilm forming bacterial isolates were screened for drug resistance on Mueller Hinton agar (MHA) against the following antibiotic discs: Streptomycin (10mg), Levofloxacin (5mg), Norfloxacin (10mg), Novobiocin (30mg), penicillin (10mg). The cultures were prepared by growing in nutrient broth at 37˚C for 24 hours until reaching an optical density equivalent to 0.5 on the McFarland scale. The cultures were individually swabbed on the agar surface and aseptically placed the antibiotic discs. Four antibiotic discs were arranged on the agar surface of a plate. The inoculated plates were incubated at 37˚C for 24 hours under aerobic condition. The zone of inhibition was measured by comparing standards of Kirby-Bauer disc-diffusion method according to Clinical Laboratory Standards Institute (CLSI).
Extraction of Turmeric and Ginger
Fresh rhizomes of turmeric were cleaned, washed with deionized water, sliced and dried in sun for one week and again. The turmeric rhizomes were ground into a coarse powder. The organic solvent ethanol was chosen for extraction of curcumin from turmeric. About 2g of ground turmeric powder was extracted with 30ml ethanol for 2hrs under agitation at room temperature. The supernatant was collected and the residual solid was washed with 10ml of the same solvent. The two supernatants were combined for each treatment. The extracts were filtered and allowed to evaporate for 5 days to get fine crystals (Liu et al., 2008). Similarly, dry ginger rhizome powder was subjected to ethanol extraction following the above method.
Separation of Curcuminoids by TLC
Ethanol extracts of turmeric were separated on TLC for presence of different curcuminoids. TLC pre-coated silica gel plate were developed using glass beaker, which was pre-saturated with mobile phase for 20 min and each plate was developed up to a height of about 6.8 cm. Chloroform : methanol mobile phase was used with composition 95: 5. After development, plates were removed and dried. Spots were analyzed.
Antibiofilm Activity- Agar Diffusion Assay
The Muller Hinton agar plates were prepared. Then the isolated bacteria were swabbed on the MHA plates. Using sterile well cutter, wells were made and the extract (30μl) was added (turmeric and dry ginger) in to the wells. Then the plates were incubated at 37˚C for 24 hours. After that the zone formation was observed.
Antibiofilm Activity- Microtiter Plate Assay
The effect of turmeric and dry ginger extracts on the formation of biofilm was qualitatively estimated by a method described by Xiao et al (2007) 150μl of exponentially growing cells were dispensed in 96-well cell culture plates. 50μl plant extracts were added to the wells and incubated for 24 hours at 37°C. The medium without extracts was used as the non-treated control. It was observed that only ethanolic extracts showed significant anti biofilm activity. After incubation, media and unattached cells were decanted and washed with Phosphate Buffer Saline (PBS). Then the plate was air dried and stained with 0.1% (w/v) Crystal Violet (Sigma- Aldrich, Germany). Excess stain was washed off thoroughly with 95% ethanol and plates were kept for drying. Optical density (OD) was measured using micro ELISA auto reader at wavelength of 490 nm. These OD values were considered as an index of attachment to surface.
Results and Discussion
Isolation of Biofilm Forming Bacteria
Bacterial strains were isolated on nutrient media, totally 28 isolates were obtained and purified. Colony morphology was observed on nutrient agar plate for these isolates (Table 1).
Characterization of Biofilm Forming Bacteria
The isolates were found to be mostly in gram positive cocci and gram negative rod shaped bacteria. Among the 28 isolates, 21 isolates are gram positive cocci shaped bacteria, seven isolates are gram negative short rod shaped bacteria. On performing motility test, all the gram positive cocci are non-motile and all the gram negative isolates are motile bacteria.
The isolates also showed both positive and negative for oxidase test. In gram positive cocci shaped bacteria, 14 isolates are oxidase positive, 8 isolates are oxidase negative. In gram negative rod shaped bacteria 6 are oxidase positive (Table 1). The isolates were streaked on to selective and differential media, for identification of bacteria. The golden yellow colour colonies were observed on Mannitol salt agar (MSA). Among the 21 gram positive cocci shaped bacteria, nine isolates produced yellow colour colonies. They were identified as Staphylococcus aureus (Table 1). The isolates were produced green colour colonies on Cetrimide agar that is identified as Pseudomonas sp. The gram negative short rod shaped bacteria only streaked on Cetrimide agar, from that all six isolates were produce green colour colonies. These six isolates were identified as Pseudomonas sp. Blood hemolysis was observed on blood agar supplemented with 5% sheep blood. Nine isolates were showed β- hemolysis; three isolates were showed α-hemolysis and other isolates showed no hemolysis. Six Gram negative rod shaped bacteria were produce β- hemolysis, three gram positive cocci shaped bacteria were showed β- hemolysis. α- hemolysis were produced by gram positive cocci shape bacteria. Lactose fermenting and non-lactose fermenting bacteria were observed on the Mac Conkey agar plate. Pink colour colony represents lactose fermenting bacteria and the white colour colony represents non lactose fermenting bacteria. All isolates were produce white colour colony so that the isolates confirmed as non-lactose fermenting bacteria (Table 1).
Table 1: Morphology and biochemical characteristics of bacteria isolated from orthodontic brackets and wires
| Isolates | Colony morphology | Gram’s Reaction | Motility | Oxidase | MSA | Blood agar | Mac Conkey | Cetrimide |
| 1 | Small circular- blue tinge | G+ve cocci | Non motile | Negative | Colorless | No lysis | NLF | – |
| 2 | Small circular- creamy | G+ve cocci | Non motile | Negative | No growth | No lysis | NLF | – |
| 3 | Small irregular green tinge | G-ve short rod | Motile | Positive | Colorless | β hemolytic | NLF | Green colour |
| 4 | Small circular mucoid | G+ve cocci | Non motile | Positive | No growth | No lysis | NLF | – |
| 5 | Small circular pin point | G+ve cocci | Non motile | Negative | Yellow colour | No lysis | NLF | – |
| 6 | Small irregular blue green | G-ve short rod | Motile | Positive | Colorless | β hemolytic | NLF | Green colour |
| 7 | Small circular pin point | G+ve cocci | Non motile | Negative | Colorless | α hemolytic | NLF | – |
| 8 | Small circular pin point | G+ve cocci | Non motile | Positive | Yellow colour | No lysis | LF | No green colour |
| 9 | Small circular-creamy | G+ve cocci | Non motile | Negative | No growth | No lysis | NLF | – |
| 10 | Small circular pin point | G+ve cocci | Non motile | Negative | Colorless | No lysis | NLF | No green colour |
| 11 | Small circular pin point | G+ve cocci | Non motile | Positive | Yellow colour | No lysis |
LF |
No green colour |
| 12 | Irregular mucoid | G+ve cocci | Non motile | Positive | Yellow colour | β hemolytic | NLF | No green colour |
| 13 | Small circular pin point | G+ve cocci | Non motile | Negative | Yellow colour | No lysis | NLF | – |
| 14 | Small circular pin point | G+ve cocci | Non motile | Negative | Yellow colour | No lysis | NLF | – |
| 15 | Irregular blue green tinge | G-ve short rod | Motile | Positive | Colorless | β hemolytic | NLF | Green colour |
| 16 | Small irregular blue green tinge | G-ve short rod | Motile | Negative | Colorless | No lysis | NLF | No green colour |
| 17 | Irregular blue green tinge | G-ve slender rod | Motile | Positive | Colorless | β hemolytic | NLF | Green colour |
| 18 | Creamy irregular mucoid | G+ve cocci | Non motile | Positive | Yellow colour | β hemolytic | NLF | No green colour |
| 19 | Small circular white color | G+ve cocci | Non motile | Negative | No growth | No lysis | NLF | – |
| 20 | Small circular white color | G+ve cocci | Non motile | Negative | Colorless | β hemolytic | NLF | – |
| 21 | Small circular yellowish creamy | G+ve cocci | Non motile | Positive | Colorless | α hemolytic | NLF | – |
| 22 | Circular creamy white | G-ve short rod | Motile | Positive | No growth | β hemolytic | NLF | Green colour |
| 23 | Small circular creamy yellowish | G+ve cocci | Non motile | Negative | Colorless | No lysis | NLF | – |
| 24 | Small irregular blue green tinge | G+ve cocci | Non motile | Positive | No growth | No lysis | NLF | – |
| 25 | Small circular transparent | G+ve cocci | Non motile | Negative | No growth | No lysis | NLF | – |
| 26 | Small irregular blue green tinge | G-ve short rod | Motile | Positive | No growth | β hemolytic | NLF | Green colour |
| 27 | Small circular white color | G+ve cocci | Non motile | Negative | Yellow colour | No lysis | NLF | – |
| 28 | Irregular creamy mucoid | G+ve cocci | Non motile | Positive | Yellow colour | α hemolytic | NLF | – |
Biofilm Formation Assay
Christensen Tube Method
The biofilm formation was also evaluated qualitatively by tube assay. The tubes were stained with crystal violet and the entire isolates shows adherence to the walls and bottom of the test tube. There are 28 isolates were isolated from that 18 isolates were producing biofilms. In that four isolates were strong biofilms formers, seven isolates were found to form moderate biofilm and seven isolates produced weak biofilms. Ten isolates lack biofilm forming activity.
Congo Red Agar Method
The isolates showed strong biofilm formation in tube method was further confirmed by Congo red agar method. The four strong biofilm forming isolates were streaked onto congo red agar plate, the isolates (3,6,8,11) showed black colonies with a dry crystalline consistency confirmed biofilm formation (Table 2). The isolates 3 and 6 were identified as Pseudomonas sp. and isolates 8 and 11 were identified as Staphylococcus aureus.
Table 2: Strong biofilm forming bacteria on congo red agar
| S. No | Isolates | Name of bacteria |
| 1 | 3 | Pseudomonas sp. |
| 2 | 6 | Pseudomonas sp. |
| 3 | 8 | Staphylococcus aureus |
| 4 | 11 | Staphylococcus aureus |
Antibiotic Sensitivity Test
Antibiotics such as Novobiocin (30mg), Penicillin (10mg), Levofloxacin (5mg), Streptomycin (10mg), and Norfloxacin (10mg) were showed both sensitive and resistant to against the biofilm forming bacteria. In Novobiocin, four gram positive cocci are sensitive, others are resistant to Novobiocin. In penicillin antibiotic all isolates were produce resistant. In Levofloxacin seven isolates were produced sensitive, two are intermediate. In streptomycin eight isolates produce sensitive, two are intermediate. In Norfloxacin nine isolates were produce sensitive and one was produce intermediate (Table 3).
Table 3: Antibiotic sensitivity results of biofilm forming bacteria
| Isolates | Novobiocin 30 | Penicillin 10 | Levofloxacin 5 | Streptomycin 10 | Norfloxacin 10 |
| 1 | R(14mm) | – | – | – | – |
| 2 | R(12mm) | R(NZ) | S(21mm) | IM(14mm) | S(17mm) |
| 3 | R(NZ) | R(NZ) | S(30mm) | S(20mm) | S(33mm) |
| 4 | R(14mm) | R(NZ) | IM(18mm) | IM(14mm) | IM(16mm) |
| 5 | R(NZ) | – | – | – | – |
| 6 | R(NZ) | R(NZ) | S(30mm) | S(20mm) | S(33mm) |
| 7 | S(34mm) | – | – | – | – |
| 8 | – | R(NZ) | – | S(21mm) | S(26mm) |
| 9 | – | R(NZ) | S(22mm) | S(15mm) | S(18mm) |
| 11 | – | R(16mm) | S(30mm) | S(32mm) | S(32mm) |
| 12 | – | R(NZ) | S(20mm) | S(21mm) | S(27mm) |
| 13 | S(33mm) | – | – | – | – |
| 14 | IM(20mm) | – | – | – | – |
| 15 | R(NZ) | – | – | – | – |
| 17 | R(NZ) | R(NZ) | S(30mm) | S(18mm) | S(31mm) |
| 18 | – | R(NZ) | IM(18mm) | S(21mm) | S(25mm) |
| 22 | R(NZ) | – | – | – | – |
| 26 | R(NZ) | – | – | – | – |
| 27 | S(33mm) | – | – | – | – |
| 28 | S(28mm) | – | – | – | – |
Extraction and Separation of Curcuminoids by TLC
Ethanol extracts were tested on TLC for presence of different curcuminoids. That is curcumin, demethoxy curcumin, bis demethoxy curcumin. Curcumin is more effective compound than the demethoxy curcumin and bis demethoxy curcumin (Fig. 1).
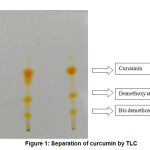 |
Figure 1: Separation of curcumin by TLC |
Anti Biofilm Activity
Agar Diffusion Assay
Control of biofilm forming bacteria using extract of turmeric and dry ginger by the method of agar diffusion assay was done. The zone of inhibition was measured on only the 4 strong biofilm forming bacteria. Dry ginger extracts showed more effective inhibition by the isolates than turmeric extracts (Table 4).
Table 4: Anti biofilm activity by using dry ginger and turmeric (agar diffusion assay)
| S. No | Bacteria | Dry Ginger | Turmeric |
| 1 | Pseudomonas sp. | 11 mm | NZ |
| 2 | Pseudomonas sp. | 13 mm | 10 mm |
| 3 | Staphylococcus aureus | 12 mm | 9 mm |
| 4 | Staphylococcus aureus | 14 mm | 11 mm |
Microtiter Plate Assay
The extraction of turmeric and dry ginger respectively showed effective inhibition against biofilm formation. In this, the same strong biofilm is used. This checked on microtiter plate by using ELISA reader in 490nm. The effect of dry ginger extract on biofilm forming was confirmed by this experiment (Table 5).
Table 5: Anti biofilm activity confirmed by the method microtiter plate assay (OD at 490nm)
| S. No | Bacteria | Ginger | Turmeric | Control |
| 1 | Pseudomonas sp. | 0.096 | 0.323 | 0.498 |
| 2 | Pseudomonas sp. | 0.0147 | 0.374 | 0.865 |
| 3 | Staphylococcus aureus | 0.154 | 0.357 | 0.540 |
| 4 | Staphylococcus aureus | 0.122 | 0.405 | 0.645 |
Biofilms are a consortium of various microorganisms which is a major source for the formation of dental plaques. A number of studies have shown an increase in the prevalence of enamel opacities following multi bonded orthodontic therapy. It is generally accepted that the presence of fixed orthodontic appliances contributes to the accumulation of plaque which in turn may lead to the development of areas for enamel demineralization presenting clinically as enamel opacities. Orthodontic therapy, especially with fixed devices, causes a disruption in the homeostasis of the oral micro biota. This disruption is due to the increase in plaque retention (Balenseifen and Madonia, 1970) and as such a common effect is increase in species that can be considered as pathogenic to different oral tissues. Usually this concerns the hard tooth tissues and specifically an increase in the demineralization of enamel leading to an increase in white spot lesions or even eventually to caries lesions (Gorelick et al., 1982; Chapman et al., 2010). These orthodontic appliances tend to cause a shift of the lesions from posterior to anterior teeth and from inter proximal to vestibular and lingual sites (Mizrahi et al., 1983). Among the many orthodontic appliances, orthodontic brackets may play a significant role in the enamel demineralization because they are attached to the dentition continuously during almost all of the orthodontic treatment period and their complex design provides a unique environment which impedes access to the tooth surfaces for cleaning. Biofilms are a consortium of various microorganisms which is a major source for the formation of dental plaques (Fournier et al., 1998). In this study, isolation of the biofilm forming bacteria adhering to orthodontic brackets and wires and its inhibition was studied. The prime causative organism for this enamel demineralization (white spot lesion) is mutans streptococci. Cariogenic mutans streptococci are currently classified into seven species, Streptococci cricetus, Streptococci ratti, Streptococcus mutans, Streptococcus sobrinus, Streptococcus downei, Streptococcus ferus, and Streptococcus macacae. Of these Streptococcus mutans and Streptococcus sobrinus have been the most frequently isolated from the oral cavity (Ann et al., 2004). In the present study, samples of the tooth swabs taken from people using brackets and wires. The samples were inoculated onto nutrient agar plates and were purified based on their different in colony morphology. Then identified by morphological and biochemical test. In this study to got more number of Pseudomonas sp and Staphylococcus aureus. These two were produce strong biofilm. In recent years, the much of the research have been focused to identify alternative medicines to treat the infections caused by the drug resistant organisms. Various chemicals have been tested for their antibiofilm activities. Unfortunately, those chemicals cannot be used as drug molecules to treat the diseases associated with the biofilm (Cowan, 1999). In present study, to alternate the chemical compounds, to used natural herbal products (dry ginger and turmeric) for control of biofilms. The bioactive compounds were extracted using the solvents-hexane and ethyl acetate. In present study, the herbal (dry ginger and turmeric) products were extracted using the solvent ethanol. The inhibition activity of both the solvents against biofilm formation was analyzed. The hexane solvent extract was found potentially effective in the inhibition of biofilms on orthodontic brackets in comparison to the ethyl acetate extract (Devangana Bhuyan et al., 2015).
Conclusion
In present study, the ethanol extraction of ginger and turmeric is used to the control of biofilm forming on orthodontic brackets. The ethanol extraction of ginger has more potentially effective inhibition of biofilms on orthodontic brackets and wires when compared to the ethanol extraction of turmeric.
Conflict of Interest
All authors have no conflict of interest.
Funding Source
No funding was received for this project.
References
- Agarwal, V., Lal, P and Pruthi, V. Prevention of Candida albicans biofilm by plant oils. Mycopathologia, 2008; 165(1): 13-19.
- Ann, S. J, Lim, B. S, and Yang, H, C. Quantitative analysis of the adhesion of cariogenic streptococci to orthodontic metal brackets. Angle Orthodontics., 2004; 75:666-671.
- Balenseifen, J. W, and Madonia, J. V. Study of dental plaque in orthodontic patients, Dent. Research., 1970; 49(2):320–324.
- Chapman, J. A, Roberts, W. E, Eckert, G.J, Kula, K. S, and Gonz´alez-Cabezas, C. Risk factors for incidence and severity of white spot lesions during treatment with fixed orthodontic appliances, J. Orthodont. Dentofac. Orthopedics., 2010; 138(2): 188–194.
- Christensen, G.D., Bisno, A.L, Simpsom, W.A, Beachey, E.H. Adherence of slime producing strains of Staphylococcus epidermidis to smooth surfaces. Infect Immun. 1982; 37:318–326.
- Cowan, M. M, Plant products as antimicrobial agents. Clinical Microbiol Rev., 1999; 12(4):564-582.
- Demling, A, Heuer, W, Elter, C, Heidenblut, T, Bach, R, Schwestka-Polly, Fr.W, and Stiesch-Scholz. M. Analysis of supra- and subgingival long-term biofilm formation on orthodontic bands. J. Orthodontics, 2009; 31; 202–206.
- Devangana, B, Madhubanti, M, Anamika, D, and Jabez, O. Removal of dental plaque formation using bioactive compounds from sea weeds. Chem. Pharm. Res. 2015; 71: 390-394.
- Dimopoulos G, Poulakou G, Pneumatikos IA, Apostolos, A, Marin H. K, Dimitrios K. M. Short- vs long-duration antibiotic regimens for ventilator-associated pneumonia: a systematic review and meta-analysis. Chest 2013; 144:1759-67.
- Essawi, T, and Srour, M. Screening of some Palestinian medicinal plants for antibacterial activity. J. Ethnopharm, 2000, 70: 343–349.
- Fournier, A, Payant, L, and Bouclin, R. Adherence of Streptococcus mutans to orthodontic brackets. Amer. J. Orthodont. Dentofac. Orthopedi., 1998; 114: 414-417.
- Gorelick, L, Geiger, A M, and Gwinnett A J. Incidence of white spot formation after bonding and banding,” J. Orthodont., 1982; 81(2): 93–98.
- Habib, S H M, Makpol, S, Hamid, N A A, Das, S, Ngah, W Z W, Yusof Y A M. Ginger extract (Zingiber officinale) has anti-cancer and anti-inflammatory effects on ethionine-induced hepatoma rats. , 2008; 63: 807-813.
- Jongsma, MA, Pelser, FD, van der Mei, HC, Atema-Smit, J, van de Belt-Gritter, B, Busscher, HJ, and Ren, Y. Biofilm formation on stainless steel and gold wires for bonded retainers in vitroand in vivo and their susceptibility to oral antimicrobials. Clin Oral Investig 2013; 17(4): 1209–1218. Jongsma, M A, van der Mei, H. C, Atema-Smit, J, Henk J Busscher, and Yijin Ren. In vivo biofilm formation on stainless steel bonded retainers during different oral health-care regimens. Int J Oral Sci. 2015; 7(1): 42–48.
- Kim, H S, and Park, H D. Ginger extract inhibits biofilm formation by Pseudomonas aeruginosa PA14, 2013, 8(9): e76106.
- Lee, K, Lee, J H, Kim, S I, Cho, M H, and Lee, J. Antibiofilm, anti-hemolysis, and anti-virulence activities of black pepper, cananga, myrrh oils, and nerolidol against Staphylococcus aureus. Appl. Microbiol., and Biotechnol., 2014; 98(22): 9447-9457.
- Liu, H, Qui, N, Ding, H, and Yao, R. Polyphenols contents and antioxidant capacity of 68 Chinese herbals suitable for medical or food uses. Food Res Int. 2008; 41:363–370.
- Marsh, P. D. Are dental diseases examples of ecological catastrophes? Microbiology. 2003; 149(Pt 2):279-294.
- Mathur, T, Singhal, S, Khan, S, Upadhyay, DJ, Fatma, T, Rattan, A. Detection of biofilm formation among the clinical isolates of staphylococci: An evaluation of three different screening methods. J. Medical Microbiol. 2006; 24 (1):25-9.
- Meliani, A, Nair, S, and Bensoltane, A. Cytobiochemical and antimicrobial investigations on essential oil of Zingiber officinale J. Essen.Oil Bearing Plan. 2014; 17(6): 1120-1129.
- Merritt, K, Victoria, M. H, Stanley A. B. Safety and cleaning of medical materials and devices. J. Biomed. Mat. Res. 2000; 53(2):131-6.
- Mizrahi, E. Surface distribution of enamel opacities following orthodontic treatment. Amer. J. Orthodontics Dentofacial Orthopedics. 1983; 84: 323-331.
- Nikolic, M, Vasic, S, Durdevic, J, Stefanovic, O, and Comic, L. Antibacterial and anti-biofilm activity of ginger (Zingiber Officinale (Roscoe)) ethanolic extract. Kragujevac J. Sci., 2014; 36: 129-136.
- Papaioannou, W,Athanasios, P, Haroula, K, Efterpi, K, and Margarita, M. Adhesion of Porphyromonas gingivalis and biofilm formation on different types of orthodontic brackets. Int J Dent. 2012; 1-6.
- Philip, D M. Dental plaque as a biofilm and a microbial community – implications for health and disease. BMC Oral Health. 2006; 6(Suppl 1): S14.
- Ren, Y, Jongsma MA, Mei L, van der Mei HC, Busscher HJ. Orthodontic treatment with fixed appliances and biofilm formation–a potential public health threat?. Clin Oral Investig. 2014;18(7):1711-8.
- Simões, M, Lúcia, S, Maria, J V. A review of current and emergent biofilm control strategies. LWT- Food Sci. Tech. 43(4): 573-583.
- Stoilova, I, Krastanov, A, Stoyanova,A, Denev, P, Gargova, S. Antioxidant activity of a ginger extract (zingiber officinale). Food chem.2007. 102: 764–770.
- Xiao, J, Zuo, Y, Liu, Y, Li, J, Hao, Y, Zhou, X. Effects of Nidus Vespae extract and chemical fractions on adherence and biofilm formation of Streptococcus mutans, Archives of Oral Biolo., 2007; 52:869-875.








