Muralidharan1 and Gundu H.R. Rao2
1Tekna Manufacturing, Chennai, India.
2Laboratory Medicine and Pathology, Director, Thrombosis Research, Lillehei Heart Institute, University of Minnesota.
Corresponding Author E-mail : gundurao9@gmail.com
DOI : https://dx.doi.org/10.13005/bpj/1913
Abstract
In 1885, the first ever recorded use of oxygen was documented for a medical purpose. The medical procedure was, to treat a patient with pneumonia. Oxygen was mainly used in hospitals, to treat patients with a variety of respiratory issues. The first form of portable medical grade oxygen was developed in 1950’s, which led to the clinical use of oxygen therapy. There is considerable observation based, as well as experimental evidence, to suggest that oxygen therapy exerts a significant physiological and pharmacological effects that improves cellular, tissue, and organ oxygenation, exerts anti-inflammatory, anti-bacterial effects, and improves tissue repair mechanisms. Despite this knowledge, the oxygen therapy to treat hypoxia related clinical conditions is limited. Since our interest is in the prevention of clinical complications related to cardiometabolic diseases, we discuss in this overview, pre-existing conditions, where oxygen therapy may play a very important role, in preventing hypoxia-mediated cell death, and protect the tissue and organ damage. Stroke affects 33 million individuals, worldwide every year and two-thirds of all strokes, occur in developing countries. Unlike developed countries, where stroke incidence has declined by 42% over the last four decades, stroke incidence rates have increased by >100% in developing, low-to middle-income countries. It is possible, that by developing a combined oxygen therapy (using Normobaric oxygen therapy followed by Hyperbaric oxygen therapy), significant number of stroke-related morbidity and mortality could be reduced. Another area of interest, that needs immediate attention is the COVID-19 related respiratory distress, hypoxia, organ failure and death. Like the stroke condition, early intervention with combined oxygen therapy, will significantly reduce hypoxia mediated, -inflammation, respiratory distress, organ failure and loss of lives, in Covid-19 patients. Efforts are in progress to test this hypothesis, in both stroke patients as well as Covid-19 patients, to validate the benefits or otherwise of combined oxygen therapy, in reducing the morbidity and mortality under these severe illness conditions.
Download this article as:| Copy the following to cite this article: Muralidharan G, Rao G. H. R. Oxygen as a Therapeutic Drug: Hyperbaric Oxygen Therapy. Biomed Pharmacol J 2020;13(2). |
| Copy the following to cite this URL: Muralidharan G, Rao G. H. R. Oxygen as a Therapeutic Drug: Hyperbaric Oxygen Therapy. Biomed Pharmacol J 2020;13(2). Available from: https://bit.ly/2BUlvix |
Introduction
Oxygen is an essential component of normal metabolism and is required by all tissues. A rough estimate of how much of oxygen each major tissue consumes is as follows: brain (48%), heart (25%), kidneys (15%), Skeletal muscle (50%) and skin (5%). It is mainly metabolized by the cytochrome- C mitochondrial enzymes (90%). Main metabolites of oxygen metabolism are carbon dioxide and water. Oxygen is also one of the most commonly used therapeutic agents. A large body of data suggests, that hyperoxia exerts an extensive sequence of physiological and pharmacological effects, improves tissue oxygenation, exerts anti-inflammatory and antibacterial effects, and augments tissue repair mechanisms.1 Despite its use in the treatment of a variety of clinical complications including, endothelial dysfunction (vascualry dysfunction), oxidative stress, hypoxia, infection, inflammation, diabetic foot ulcers, and tissue repair, many aspects of its physiologic and pharmacologic actions, lack evidence-based data. Normobaric hyperoxia is used via a wide variety of simple delivery systems, that allow delivery of oxygen of 24 to 90%. There is considerable evidence, to suggest a therapeutic role for oxygen in cerebral ischemic stroke, head injury, near drowning, asphyxia, and cardiac arrest.2-7 An area of controversy that is of great interest to us, is the use of Normobaric oxygen therapy in asphyxiated newborn infants. Available data support, an overall beneficial effect of hyperoxia (21% 0xygen) in this condition. We in India, will have an opportunity to test this hypothesis, in the World’s largest studies on babies with brain injury.
Brain injury during labour or childbirth, is one of the leading causes of epilepsy, in babies in some areas of the world. A common cause is perinatal asphyxia, -where oxygen is cut off to the foetal brain, damaging it. Imperial college, London, is leading the ‘Prevention of Epilepsy by Reducing Neonatal Encephalopathy (PREVENT) study in Bengaluru, India. Researchers from Imperial College and other institutions in the UK (3.4 million pounds project, funded by NIHR, UK) and India, will study around 60,000 women recruited from two major hospitals in South India, – Bengaluru Medical College and Calicut Medical College. There are several methods of non-invasive oxygen delivery to the neonates, -head box oxygen, nasal prongs, nasopharyngeal catheter. It is important to know the safety, efficacy, the risks, and the impact on lung function.8 All methods of oxygen administration needs supervision by trained personnel to detect and manage complications appropriately. In adults, oxygen therapy is prescribed for people who cannot get enough oxygen on their own. Some of the clinical conditions that require oxygen therapy include, chronic obstructive pulmonary disease (CODP), pneumonia, acute respiratory distress, asthma, bronchopulmonary dysplasia, heart failure, cystic fibrosis, and sleep apnea.
Hypoxia causes pulmonary vasoconstriction, without elevating adrenaline or catecholamines. This hypoxia induced vasoconstriction is not global but regional, -leading to an inadequate distribution of the blood though the various parts of the lungs. Hypoxia also seems to decrease cerebral blood flow. Despite the knowledge on the role of hypoxia and hyperoxia on central circulatory hemodynamics, much less is known about its effects on regional hemodynamics. According to the experts, tissue hypoxia activates a large variety of vascular inflammation and may lead to systemic inflammatory response, that in many cases culminates in multiple organ dysfunction and multiple organ failure.9-12 According to the Chinese investigators, progressive hypoxia is a characteristic manifestation in the clinical course of severe and critically ill patients with COVID-19 Pneumonia.13 In persons with high altitude sickness, levels of circulating proinflammatory cytokines increase, cause pulmonary or cerebral edema.14 Hypoxia can induce inflammation, inflamed lesions become severely hypoxic, as a result steep oxygen gradient will develop, followed by an increased metabolic demand, decrease in metabolic substrates, caused by thrombosis, trauma, compression (interstitial hypertension) and atelectasis. Furthermore, multiplication of intracelluar pathogens can deprive infected cells of oxygen.15
The inflammatory responses elicited by pathogens occur in the interstitial space, which is hypoxic. Blood supply to the site is restricted, because vessels are clogged with immune cells, thrombi, or fibrin.16 Due to rapid endothelial dysfunction, microthrombi may occur by activation of coagulation system, resulting circulatory dysfunction, suppression of oxygen utilization by mitochondria, -energy depletion and organ failure. The immune and coagulation systems are critically regulated by the endothelial cells, which regulate the blood flow to the organs and tissues, -endothelial dysfunction leads to organ dysfunction. Monitoring endothelial dysfunction both at regional vascular beds as well as in the central circulatory branches is very important. There are several devices available in the market, that can monitor changes in the flow velocity and provide information on endothelial dysfunction.17 Some of the devices in use include, CV Profilor (Hypertension Diagnostics TM of USA: hypertensiondiagnostics.com), Periscope (Genesis Medical System, Hyderabad, India: genesismedicals.com) and TM-Oxi (LD Technologies, Florida: www.ldteck.com). The commercial devices dedicated to PWV measurements estimate a regional assessment, measured between two vessels. However, we feel that a regional measurement of vascular dysfunction is more precise for evaluation of the health of the vessels.
According to Singhal and associates, there is a renewed interest in the Normobaric oxygen (NBO) therapy or inhaled high-flow oxygen, because of its practical benefits.18 It is simple, widely available, and quite effective. Recent data suggests, that NBO may have rapid effects in stroke patients, and can be started promptly after symptom onset. Studies have demonstrated, that NBO slows down the process of ischemic cell death after stroke. According to the researchers, this “stopping the stroke clock” effect, may provide an opportunity to extend the time window for thrombolysis.” Alternately, a combination therapy of NBO and thrombolysis, can be initiated in ambulatory conditions under the supervision of critical care providers. A new study suggests, that an NBO may even be protective in permanent cortical ischemia.19 A follow-up of a similar study using novel 2-D multivoxel MR spectral reflectance imaging, and speckle flowmetry, found that NBO provides cerebral perfusion and oxygenation in ischemic regions, and inhibits peri-infarct depolarizations.20 Authors speculate, that successful results from on-going studies on hyperoxia trials, may ultimately yield a combined therapeutic approach, where NBO is started in the field or in the ambulance and subsequently combined with HBO, infusion of super-oxygenated solution or thrombolysis.
Oxygen therapy in one form or the other, is used to treat a variety of medical conditions. Medical institutions use oxygen therapy in different ways. Some of the common conditions, which the oxygen therapy is recommended include, anemia (severe), acute respiratory distress, brain abscess, brain injury, burn, decompression sickness, cardiac failure, carbon monoxide poisoning, crushing injury, diabetes foot ulcers, gangrenes, infection of skin with tissue loss, non-healing wounds, radiation injury, skin grafts, vision loss sudden and painless.21-31 Internet search on common uses of hyperbaric oxygen therapy (HBOT), reveals that HBOT, is a type of treatment commonly used to speed up healing gangrenes, stubborn wounds, in which tissues are starved for oxygen. Wound injuries damage the blood vessels, which release fluid leaks into the tissue and cause swelling. The elevated pressure in chamber increases the amount of oxygen in the blood, breaks cycle of swelling, oxygen starvation and tissue death. HBOT encourages the body’s oxygen radical scavengers to seek out the problem molecules and allow healing to continue. HBOT helps bock, the action of harmful bacteria, and other pathogens, and helps the immune system. HBOT encourages the formation of new collagen and new skin cells.
Discussion
SARS CoV-2 virus has created an unprecedented COVID-19 pandemic worldwide. Of the total hospitalized COVID-19 patients, 89% had at least one of the pre-existing chronic conditions. About half, had high blood pressure and obesity, according to the Centers for Disease Control (CDC), USA. And about a third, had diabetes and a third had cardiovascular (CVD) disease. According to the Chinese researchers, clinical manifestation of COVID-19 are heterogenous. During the time of admission COVID-19 patients reported as having at least one comorbidity, diabetes (10-20%), hypertension (10-15%), or other cardiovascular diseases and cerebrovascular diseases (7-40%). Analysis of 1590 hospitalized patients in China, revealed that mean average age was 49 years. The most prevalent comorbidity was hypertension (16.9%), followed by diabetes (8.2, %). They found that circulatory and endocrine comorbidities, were common among patients with COVID-19 patients, leading to their conclusion, – that circulatory diseases remained the most common category of comorbidities32 Since area of our interest is the prevention of acute cerbrovascular and cardiovascular events, we will limit our discussions to treatment of oxygen therapy for thrombosis and stroke.
Harvard researchers Professor Singhal and associates, based on their extensive work on the oxygen therapy of ischemic stroke, suggested a combined therapeutic approach, where NBO is started in the field or in the ambulance, and subsequently combined with HBO, infusion of super-oxygenated solution or thrombolysis.20, 33 There has been more than 100 per cent increase in incidence of stroke in low- and -middle income countries, including in India from 1979-2008.34 Stroke is a major global public health problem and is the second leading cause of death worldwide. Appropriate timely interventions could significantly reduce the morbidity and mortality associated with stroke. Stroke is a sudden interruption of the blood supply to the brain. Most common cause is a blockage of a cerebral artery by a blood clot. Suggestions made by Professor Singhal of Harvard group, seems to be timely and useful, for the prevention of hypoxia induced tissue damage and the conditions that follow deprivation of much needed oxygen to the brain tissue. TEKNA Oxygen delivery systems, a part of the TEKNA Manufacturers of Chennai, India, is developing a variety of NBO and HBO systems, for use in oxygen therapies. Scientific and technology advisers for this group are suggesting these entrepreneurs, to work with the Neurosurgeons and Neurologists, to develop a combination oxygen therapy for stroke victims.
The results of the studies done by Professor Singhal and associates demonstrated that Normobaric (NBO) oxygen therapy is neuroprotective (20). They used Magnetic Resonance Spectroscopy, to follow the effect of Oxygen therapy in ischemic stroke patients. Choda and Rao have demonstrated that changes in blood flow can be followed by using Infrared thermal imaging.34, 35
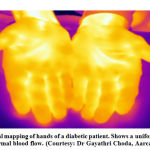 |
Figure 1: Thermal mapping of hands of a diabetic patient. |
This kind of imaging technology has been used in vascular surgery for brain mapping36 Using infrared imaging, real-time vascular occlusion and reperfusion of the vessels of the brain with blood during surgery, has been demostrated in earlier studies.37 Shown in the Figure 1 is a thermal map of hands of a diabetic, who is under robust medical management. There is an even and symmetrical thermal image, suggesting uniform blood supply. In order to successfully test the benefits or otherwise of combined oxygen therapy, there are efforts in progress in Bengaluru, India, to develop a comprehensive stroke prevention strategy, between the staff of the TEKNA Oxygen therapy group (www.hyperbaric-chmaber.com), Chennai, India, thermal imaging technologists (Aaraca Research Pvt. Ltd. https: //aaracaresearch.com), and the NewroRehab (newrorehab.com) group. Results of the combined oxygen therapy efforts will be reported in our future publications.
Coronavirus 2019 (Covid-19) pandemic, has created a public health crisis worldwide. The SARS CoV-2 virus is affecting 212 countries around the world. The most common pattern of coagulopathy observed in patients with COVID-19, is characterized by elevations in fibrinogen and D-dimer levels. This correlates with parallel rise in markers of inflammation (C-reactive Protein). Unlike classical sepsis mediated disseminated intravascular coagulation (DIC), the degree of activated partial thromboplastin (aPT) elevation is less than partial thromboplastin (PT) elevation. In view of these observations, treatment with low molecular weight heparins (LMWH), tissue plasminogen activator (tPA) or with antiproteases targeting plasmin, seems to be a better option. If effective and safe, these therapies could save lives by reducing the recovery time and freeing up more ventilators for other patients in need. Many COVID-19 patients who need a ventilator never recover. Although survival rates vary from country to country, a report from London’s Intensive Care National Audit and Research Center, found that 67% of reported COVID-19 patients from England, Wales, and Northern Ireland, receiving “advance respiratory support” died. A study in a similar patient group in China, found only 14% survived, after going on a ventilator. In New York City, an astronomical 80% of patients, who required ventilator at the height of this pandemic died, according to the city and state officials.
According to the Chinese investigators, progressive hypoxia is a characteristic manifestation in the clinical course of severe and critically ill patients with COVID-19 Pneumonia. Oxygen therapy plays an important role in the alleviation of respiratory distress. Hyperbaric Oxygen (HBO)Therapy (HBOT), is the most powerful oxygen therapy known, and may be the best choice of oxygen therapy for severe critically ill adult patients with COVID-19 Pneumonia.38, 39 Chinese researchers in Wuhan, China, performed HBO treatment in severe COVID-19 patients and concluded that, – “HBOT can effectively correct systemic hypoxia, benefit to improve circulation, and immune function. Early HBO treatment, may improve the total efficiency of systemic support treatments, reduce the use of mechanic ventilation and lower mortality rate of severe or critically ill patients with COVID-19.” Prof. Paul Harch of Department of Medicine, Section of Emergency Hyperbaric Medicine, Louisiana State University, New Orleans, concluded, “With just 3-8 HBOTs the patients were bridged through the hypoxemic crisis phase of the infection and successfully discharged from the hospital.” The author suggests that HBOT applied earlier in the disease process, would prevent the deterioration that leads to the significant morbidity and mortality of COVID-19 infection.40
In an analysis of more than 4,000 covid-19 patients, evaluated between March1st and April 7th, at the NYU Langone Health facilities, one of the strongest predictors of critical illness- defined as involving I.C.U. care or mechanical ventilation – was the patient’s oxygen saturation, on arrival at the hospital.41 “The more we look, the more likely it becomes that blood clots are a major player in the disease severity and mortality from Covid-19,” Bikdeli says.42 Infection may also lead to blood vessel constriction. Reports are emerging of ischemia in the fingers, and toes, -a reduction in blood flow that can lead to severe hypoxia, tissue, and organ death.43 SARS CoV-2 targets blood vessels, hence people with comorbidities such as diabetes and hypertension, with pre-existing damage to those vessels, face higher risk of serious illness.32 In a small pilot study of 250 Covid-19 cases, conducted by Dr Cosentini in Italy, half were found to have mild pneumonia, -but their oxygen saturation was not yet compromised. All these patients were discharged from E.R., and they were sent home with pulse oximeters. None of these patients required a ventilator (Richard Levitan et al: The New York Times May 10, 2020). We have several options, to help these patients who are suffering from an illness, which has no cure at the time of this writing. Having said that, we do have treatment options, that include various noninvasive methods of delivering oxygen, including Normobaric oxygen and Hyperbaric oxygen, patient positioning maneuvers, that open parts of lungs, and close monitoring, treatment of inflammation and thrombosis.
 |
Figure 2: Tekna Monoplace Hyperbaric Oxygen Chamber (Courtesy: TEKNA Manufacturers, Chennai, India) |
After reviewing the works of Harvard researchers, the critical care workers of New York City, and the Italian group, we have come to the conclusions, -that as suggested by Prof Aneesh Singhal of Harvard, and Dr. Paul Harch of Mississippi, there is a great need to develop a combined oxygen therapy, to address the hypoxia -mediated clinical complications, in the treatment of stroke patients, as well as in Covid-19 patients (20, 39- 45). We have initiated a dialogue, with the staff of the critical care, at the Columbia Asia Hospital, Bengaluru, Neurosurgery Group at the Mahaveer Jain Hospital, Bengaluru, and the science and technology experts at TEKNA Hyperbaric Oxygen Chamber (https://hpyerbaric-chambers.com) Manufacturers, Chennai, India. Combined oxygen therapy may play a very important tissue/organ protective role, in the treatment of stroke patients, as well as Covid-19 patients. Made in India, Tekna Hyperbaric Oxygen chambers will be validated for safety and efficacy, before using them for combined oxygen therapy (Fig 2). Results of these collaborative studies will be reported in our future publications.
Conclusion
Molecular oxygen has been used as a therapeutic drug for decades, under medical supervision to treat and manage hypoxic conditions, to protect the cells, tissues, and organs from irreparable damage and destruction. There are a variety of medical grade oxygen delivery systems to accomplish these goals. Having said that, this subject, ‘oxygen therapy’ remains, poorly understood and inadequately practiced. There are many comprehensive reviews, guidelines, and recommendations by professional organizations on this subject, and readers are urged to refer to them for further useful information and for clinical applications. In view of our interest in vascular biology, we have limited our discussions to two very specific areas, -management of hypoxia in stroke, and acute respiratory distress, in covid-19 patients. In both these conditions, where time is the essence, as hypoxia mediated damage occurs rapidly, developing a combination therapy using Normobaric oxygen and Hyperbaric oxygen, may prove to be very useful. In stroke patients, Normobaric oxygen therapy can be started as soon as symptoms start, by medical attendants and if needed, Hyperbaric oxygen therapy can be combined with Normobaric oxygen therapy, to obtain better outcomes. Of course, such therapies can be given independently, at the discretion of critical care clinicians. In the Covid-19 patients also, not all patients need HBO therapy. Using oximetry to follow the degree of hypoxia, the clinicians may provide NBO initially, and if needed proceed with the combined NBO and HBO treatments. Under the expert care of critical care clinician’s oxygen therapy, is safe and effective, in protecting tissue and organ damage in these seriously ill patients.
References
- Bitterman H: Bench-to-bedside review: Oxygen as a drug. Critical Care 13:205(2009). https://doi.org10.1186/cc7151.
- Bouachour G, Cronier P, Gouello JL et al: Hyperbaric oxygen therapy in the management of crush injuries: a randomized double-blind placebo-controlled clinical trial. J Trauma 41 (2):333-39, 1996.
- Sukoff MH, Ragatz RE: Hyperbaric oxygenation for the treatment of acute cerebral edema. Neurosurgery. 10:29-38, 1982
- Nemoto EM, Bettermann K: Basic physiology of hyperbaric oxygen in brain. Neurol Res. 29:116-126, 2007.
- Rockswold SB, Rockswold GL, Defillo A: Hyperbaric oxygen in traumatic brain injury. Neurol Res. 29:162-72, 2007.
- Rusyniac DE, Kirk MA, May JD et al: Hyperbaric oxygen therapy in acute ischemic stroke: results of the hyperbaric oxygen in acute ischemic stroke trial pilot study. Stroke 34:571-74, 2003.
- Singhal AB: Oxygen therapy in stroke: past, present and future. Int J. Stroke 4:191-200, 2006.
- Frey B, Shann F: Oxygen administration in infants: Review. Arch Dis. Childhood-Fetal and Neonatal Edition 2003; 88: F84-F88.
- Nathan C: Oxygen and the inflammatory cell. Nature. 17:675-676, 2003.
- Lefer AM, Lefer DJ: Pharmacology of the endothelium in ischemia-perfusion and circulatory shock. Ann Rev Pharmacol. Toxicol 33:71-90, 1993.
- Dietch EA: Gut failure: its role in the multiple organ failure: Pathophysiology and Basic Concepts of Therapy. New York: Thieme Medical Publisher;4-59, 1990.
- Buras J: Basic mechanism of hyperbaric oxygen in the treatment of ischemia-reperfusion injury. Int. J. Anesthesiol. Clin. 38: 91-109, 2003.
- Zhong X, Tao X, Tang Y, Chen R. The outcomes of hyperbaric oxygen therapy to retrieve hypoxemia of severe novel coronavirus pneumonia: first case report. Zhonghua Hanghai Yixue yu Gaoqiya Yixue Zazhi. doi: 10.3760/cma.j.issn.1009-6906.2020.0001.
- Hackett PH, Roach RC: High-altitude illness. N. Engl. J. Med. 345:107-14, 2001.
- Kempf VA, Lebiedziejewski M, Alitalo K et al: Activation of hypoxia-inducible factor-1 in bacillary angiomatosis: evidence for a role of hypoxia-inducible factor-1 in bacterial infections. Circ 111:1054-62, 2005.
- Hirota K: Involvement of hypoxia-inducible factors in the dysregulation of oxygen homeostasis in sepsis. Cardiovasc Hematol Disord Targets 15 (1):29-40, 2015.
- Rao GHR: Flow Velocity, Fluid Dynamics and Vascular Pathophysiology. Ann. Heart. 1 (1):1-8, 2016
- Singhal AB, Lo EH: Advances in emerging nondrug therapies for acute stroke 2007. Stroke 39:289-291, 2008
- Veltkamp R, Sun L, Herrmann O et al: Oxygen therapy in permanent brain ischemia: potential and limitations. Brain Res. 1107:185-191, 2006
- Singhal AB, Ratai E, Benner T et al: Magnetic resonance spectroscopy study of oxygen therapy in ischemic stroke. Stroke 38:2851-2854, 2007.
- Zamboni WA, Riseman JA, Kucan JO: Management of Fournier’s gangrene and the role of hyperbaric oxygen. J. Hyperbaric Med 5 (3): 177-186, 1990.
- Zamboni WA, Wong HP, Stephenson LL: Evaluation of hyperbaric oxygen for diabetic wounds: a prospective study. Underseas & Hyperbaric Med. 24 (3):175-79, 199720).
- Kalani M Jorneskog G Naderi N et al: Hyperbaric oxygen (HBO) therapy in treatment of a diabetic foot ulcers. Long-term follow-up. J. of diabetes and its complications 16 (2):153-58, 2002.
- Chen J: The effects of Hyperbaric Oxygen Therapy on Diabetic Retinopathy. Invest. Opt. Visual Sci. 44 (5): 4017-B720, 2003.
- Lampi LA, Frey G Dietze T et al: Hyperbaric oxygen intracranial abscesses. J. Hyperbaric Med. 4 (3):111-126, 1989.
- Mader JT, Adams Sr Sutton TE: Infectious disease: pathophysiology and mechanisms of hyperbaric oxygen. J. Hyperbaric Med. 2 (3):133-140, 2009.
- Cianci P, Lueders H, Lee H et al: Adjunctive Hyperbaric Oxygen Therapy Reduces the Need for Surgery in 40-80% Burns. J. Hyperbaric Med. 3 (2):97-101, 1988.
- Bennet MH, Weibel S, Wasiak J et al: Hyperbaric Oxygen Therapy for acute ischemic stroke. The Cochrane Database for Systematic Rev. 11 (11):CD004954. 2014.
- Carson S, McDonagh M, Russman B et al: Hyperbaric oxygen therapy for stroke: a systematic review of evidence. Clin Rehab. 18 (8): 819-33, 2005.
- Sharifi M Fares W, Abdel-Karim I et al: Usefulness of hyperbaric oxygen therapy after percutaneous coronary intervention for acute myocardial infraction or unstable angina. Am J. Cardiol. 93:1533-1535, 20014.
- Yogaratnam JZ, Laden G, Madden LA et al: Hyperbaric oxygen: a new drug in myocardial revascularization and protection? Cardiovasc Revasc. Med. 7:146-154, 2006
- Rao GHR: COVID-19 and Cardiometabolic Diseases: Guest Editorial. EC Cardiol.7.6(2020):08-12.
- Singhal AB Lo EH: Oxygen therapy in ischemic stroke: clinical aspects. Textbook of Hyperbaric Oxygen Therapy (Zhang JH ed.) 2008;115-134.
- Kamalaknnan S, Gudlavalleti ASV, Gudlavalleti VSM et al: Incidence & prevalence of stroke in India: A systematic review. Ind J. Med Res. 146 (2): 175-185, 2017. PMCID:5761027.
- Choda G, Rao GHR: Thermal Imaging for the diagnosis of early vascular dysfunctions: A case report. J. Clin Cardiol. & Diagn. 3 (1):1-7, 2020.
- Rojas E, Ochoa EEM, Lopez RL et al: Infrared thermography brain mapping surveillance in vascular neurosurgery for anterior communicating artery aneurism clipping. Surg Neurol Int. 9:188, 2018. PMID: 30294492.
- Watson JC, Gorbach AM, Pluta RM et al: Real-time detection of vascular occlusion and reperfusion of the brain during surgery by using infrared imaging. J. Neurosurgery. 2002. https://doi.org/10.3171/jns.2002.96.5.0918.
- Chen R, Zhong Xi, Tang Y et al: The outcomes of Hyperbaric Oxygen Therapy to serve and critically ill patients with COVID-19 pneumonia. 2020. https://oxycamaras.com.br/wp-content/uploads/2020/04/Outcome-of-HBOT-to-COVID19.pdf.pdf.pdf.pdf.pdf
- Zhong XL, Tao XL, Tang YC, et al. Effect of hyperbaric oxygen therapy to treat hypoxia in Severe novel coronavirus pneumonia patients: First case report. Chin J Nauti and Hyperb. Med. 2020,27 (2020-02-24). http://rs.yiigle.com/yufabiao/ 1182641.htm. DOI: 10.3760/cma.j.issn.1009-6906.2020.0001.
- Harch PG: Hyperbaric Oxygen Treatment of Novel Coronavirus ©VID-19) respiratory failure. Commentary. Med. Gas Res (Epub ahead of print). Available from: http://www.medgasres.com/preprintarticle.asp?id=282177
- Petrililli CM, Jones SA, Yang JY et al: Factors associated with hospitalization and critical illness among 4,103 patients with Covid-19 dieses in New York City. medRxiv preprint doi: https://doi.org/10.1101/2020.04.08.20057794.th
- Bikdeli B, Madhavan MV, Jimenez D et al: COVID-19 and thrombotic or thromboembolic disease: Implications for prevention, antithrombotic therapy and follow-up. JACC; April 2020. DOI:10.1016/j/jack.2020.04.031
- Wadman M, Couzin-Frankel, Kaiser J et al: How does coronavirus kill? Clinicians trace a ferocious rampage through body, form Brian to toes. Science; Posted in Biology, Coronavirus. 2020. Doi:10.1126/Science.abc3208
- Richard Levitan, Nicholas Caputo, Roberto Cosentiniand Jorge Cabrera: We treated older patients. Here’s how to save more of them. By: By Richard Levitan et al: NYT Opinion https://ift.tt/2x0x4pC
- Yan D, Shan J, Xiao-yan Z et al: The effects of combined hyperbaric oxygen on patients with post-stroke depression. J Phys Ther. Sci. 27 (5): 1295-1297, 2015. PMID:26157204.








