Julnar Karappara1, Prakashini Koteshwar2, Nitika C. Panakkal1 , Suresh Sukumar1
, Suresh Sukumar1
1Department of Medical Imaging Technology, Manipal College of Health Professions, Manipal Academy of Higher Education, Manipal, Karnataka, India
2Department of Radio diagnosis and Medical Imaging Technology, Kasturba Medical College, Manipal Academy of Higher Education, Manipal, Karnataka, India
Corresponding Author E-mail : nitikacp@gmail.com
DOI : https://dx.doi.org/10.13005/bpj/1899
Abstract
The number of CT scans have increased and the usage of CT in children is also rapidly increasing. As children are more prone to the effects of radiation, it is necessary to optimize the dose received by the patient. The purpose of this study was to develop a low dose, age-specific protocol for pediatric CT brain without jeopardising image quality. A total of 69 Subjects referred for routine CT brain were included in the study and categorized into three groups according to their age [1-4, 5-9, 10-16 years]. All the scans were performed in a 64 slice brilliance CT Philips using a newly developed brain protocol. The mAs used was adjusted for the different age groups. Effective dose was estimated from the Dose length product utilizing age-specific conversion factors, and the image quality was evaluated qualitatively using a 4 point scoring system by a radiologist. The effective dose was found to be 1.3±0.3 mSv for 1-4 years, 1.2±0.2 mSv for 5-9 years and 1.63 ±0.09mSv for 10-16 years resulting in a dose reduction up to 71 %, 59 % and 35 % respectively. None of the low dose CT- head studies was rated diagnostically unacceptable, however, for age groups [1-4, 5-9 years], the noise and image acceptability was graded suboptimal quality. There was a significant reduction in radiation doses imparted to patients undergoing CT examination of the brain without much loss of diagnostic information. Advanced technologies in newer CT models can be used in combination with age/size specific protocols resulting in significant reduction of radiation dose.
Keywords
Computed Tomography; Effective Dose; Pediatrics; Radiological Imaging
Download this article as:| Copy the following to cite this article: Karappara J, Koteshwar P, Panakkal N. C, Sukumar S. Optimization of Pediatric CT Brain Protocol to Achieve Reduced Patient Dose. Biomed Pharmacol J 2020;13(1). |
| Copy the following to cite this URL: Karappara J, Koteshwar P, Panakkal N. C, Sukumar S. Optimization of Pediatric CT Brain Protocol to Achieve Reduced Patient Dose. Biomed Pharmacol J 2020;13(1). Available from: https://bit.ly/2wHVRex |
Introduction
Computed Tomography (CT) is an imaging procedure that produces crossectional images of specific areas which help in the diagnosis of various disease conditions. Unlike most other modalities, the increased usage of CT has resulted in high exposure rates towards ionizing radiation among patients. CT currently is considered as a significant contributor to population dose from medical procedures[1]. Moreover, the usage of CT in children is rapidly increasing, and CT brain is the most frequent CT examination undertaken in pediatric population[2]. The increased rate of pediatric CT is mainly due to the introduction of high speed helical scanners that minimizes the need for sedation[3< /sup>]. The main drawbacks of CT examination is the radiation dose imparted to the patient. Radiation causes damage to the cell which leads to measurable somatic and genetic effects. These effects of radiation are seen both in adult and pediatric population and is a cause of concern to both. However, due to increased radiosensitivity, children are more susceptible to the risk of developing stochastic late effects as these occur more in cells which has the least maturity and specialisation, greatest reproductive activity and longest mitotic activity. Many technologies have been developed to reduce radiation exposure. Still, there is a requirement to optimise and adjust scan parameters [4]. However, decreasing the dose can increase noise that can deteriorate the image quality. As the quality of image in CT is primarily depended on the x-ray detected, technical factors in pediatric CT can be reduced as children have less thickenss and density bones[5]. Radiation dose can be decreased by choosing appropriate scan volume and adjusting scan parameters like pitch, kVp, mAs, rotation time, slice width, slice gap and usage of dose modulation techniques. However, the major disadvantage on the use of “automatic tube current modulation” for CT brain is the decreased image quality due to asymmetry in head shape when compared to other body parts, but it would be acceptable to use “automatic tube current modulation” provided diagnostic image quality is maintained[6]. Moreover, the large variations of body size and composition across the pediatric age groups, there is a need for developing age/size specific protocols. Therefore radiographers can reduce dose to the patient by selecting appropriate exam protocols and become less dependent on the scanners default protocols. Thus, the purpose of our study was to determine whether the newly developed age based protocol for pediatric CT could be used without jeopardising the image quality.
Materials and Methods
The study approval was acquired from the Institutional Research Committee, and Ethical Committee. By using convenience sampling technique, a total of 69 pediatric patients with age ranging from 1 to 16 years were included in the study. Pediatric patients whose head size were disproportionate to age such as microcephaly were excluded from the study as it could alter the dose received by the patient. The 69 patients were categorised into three groups according to their age[1-4,5-9 &10-16 years] with 23 patients in each group. All scans were done in a 64 slice brillance MDCT, Philips using a newly developed protocol with factors set according to the age. The low dose protocol was set using a 16 cm head mimicking water phantom with minimum settings and image quality was evaluated. Three different mAs settings were used for different age groups [80 mAs for 1-4 years, 100 mAs for 5-9 years, and 150 mAs for 10-16 years] while pitch was increased from 0.675 to 1 and rotation time was reduced from 1.5 to 0.5s for all the three groups. The dose length product was noted down from the CT console, and effective dose was calculated using “age-specific conversion factors” [table I][7]. Effective dose obtained was compared with standard protocol in which mAs and kVp was 300 and 120 ,respectively.
Table 1: Normalized values for effective dose per dose length product (DLP) for head and (standard) patient ages(7).
| Region of the body | Effective dose per DLP by age (mSv(mGy*cm)-1) | ||||
|
Head |
0 year | 1 year | 5 year | 10 years | Adult |
| 0.011 | 0.0067 | 0.0040 | 0.0032 | 0.0021 | |
Image Quality Analysis
Qualiy of the Image was evaluated qualiatively using a 4 point scoring system by an experienced radiologist on a digital PACS system. The parameters included were “noise and image acceptability”, “grey white matter differentiation”, “sharpness of subarachnoid space” “visualization of posterior fossa structures” and “streak artifacts”. The categories in each group were scored as 0,1,2 & 3 indicating as unaccepatable, suboptimal,acceptable/good and excellent respectively. Diagnostic acceptabilty was considered acceptable when there is sharpness in ventricular outlines and when tissue contrast is satisfactory. Grey white matter differentiation was evaluated in internal capsule,fourth ventricle and corona radiata. Sharpness of subarachnoid space was seen in ventricular margin, sulci and cisternal space. Visualization of posterior fossa structures was assessed by clear visualization of sigmoid sinus, vermis and cerebellar folia. Streak artifacts grading was based on the presence of streak artifacts affecting diagnosis,presence of streak artifacts not affecting diagnosis and streak artifacts absent. The quality of the image was evaluated by observing the most frequently (mode) occuring number from the given categories and percentage was taken for each category.
Results
Dose information was obtained from a total of 69 subjects. They were categorized into three groups based on their age [1-4, 5-9, 10-16 years] and each group had 23 subjects.
CT Radiation Dose
The mean effective dose and mean DLP for various pediatric age groups using the new protocol is shown in table II.
Table 2: Mean effective dose and DLP for various pediatric age groups using the new protocol
| Age
(years) |
DLP
(mGy*cm) |
mAs | Mean ED
(mSv) |
| 1-4 | 261 | 80 | 1.7 |
| 5-9 | 312 | 100 | 1.2 |
| 10-16 | 523 | 150 | 1.6 |
Statistical Analysis
“Mann Whitney U test” was used to compare the effective dose between the low dose protocol and the standard protocol for CT brain.
The low dose protocol brought about a 71 % decrease in dose for 1-4 year age group. Similarly, in 5-9 years and 10-16 years there was a 59 % and 35 % decrease in dose which is shown to be statistically significant (p<0.05).
Figure 1 shows the box plot of effective dose distribution for CT brain in different age groups in both low dose and standard protocols.
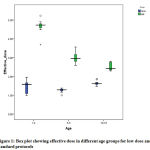 |
Figure 1: Box plot showing effective dose in different age groups for low dose |
Image Quality Analysis
Image quality was scored based on 5 quality aspects by a radiologist in blinded fashion using a 4 point scoring system. The image was analyzed based on “noise and image acceptability”, “gray white matter differentiation”, “sharpness of subarachnoid space”, “visualization of posterior fossa structures” and “presence of streak artifacts”.
None of the low dose CT brain studies were graded diagnostically unacceptable. However, for age groups 1-4 years and 5-9 years, out of 46 subjects, noise and image acceptability was graded suboptimal quality for 20 subjects. Among 69 subjects grey white matter differentiation was graded 2 for 35 subjects indicating good differentiation. Sharpness of subarachnoid space was graded 3 in a total of 37 subjects showing excellent interface of subarachnoid space with parenchyma. Visualization of posterior fossa structures was good in all the three age groups. The streak artifacts were absent in 57 subjects and were scored 2. [Table III].
 |
Table 3: Modal score of image quality based on 4 point scoring system |
Overall Image Quality for 1-4 Year Age Group
The overall image quality for 1-4 year age group using 80 mAs was found to have reduced diagnostic quality as there was a slightly greater noise and lack of gray white matter differentiation in about 48 % and 35 % of the patients respectively. However majority of the subjects were graded 2 or 3 indicating acceptable or excellent with respect to “gray white matter differentiation”, “sharpness of subarachnoid space”, and “visualization of posterior fossa”. Streak artifacts was absent in 18 subjects out of 23.
Overall Image Quality for 5-9 Year Age Group
The overall image quality for 5-9 year age group using 100 mAs was found to be diagnostically acceptable as majority subjects were scored 2 or 3 indicating acceptable or excellent quality with respect to gray white matter differentiation, sharpness of subarachnoid space, visualization of posterior fossa and absent streak artifacts (22 subjects out of 23). However, only 9 subjects showed suboptimal quality in terms of noise and image acceptability.
Overall Image Quality for 10-16 Year Age Group
The overall image quality for 10-16 year age group using 150 mAs was found to be diagnostically acceptable as majority subjects were graded acceptable or excellent quality according to image quality assessment criteria’s like “noise & image acceptability”, “gray white matter differentiation”, “sharpness of subarachnoid space”, and “visualization of posterior fossa”. Similarly, streak artifacts was absent in 17 subjects. However, only 7 subjects showed suboptimal quality in terms of “noise and image acceptability”.
We also assessed few cases [11 cases out of 69] which had abnormalities in the brain. Even though the number of such cases were less, the pathologies were well appreciated. Although, 80 and 100 mAs images depicted a slightly greater noise, they had adequate perceived resolution for routine clinical indications.
Discussion
There is a high probability of developing radiation-induced carcinoma in the pediatric population due to multiple factors such as “increased sensitivity, a small cross-sectional area in children and long latent period of oncogenic effects of ionizing radiation”[8]. Therefore it is always mandatory to perform pediatric CT in age/size protocols as there are variations in size of anatomical structures with age.
Various manipulations of techniques within CT protocols can bring a considerable reduction of patient dose. Tube current (mA) and radiation dose have a linear relationship, which means decreasing the mAs by 50% will reduce the dose by half[9]. Various studies have been done to optimize pediatric CT protocols. One such study conducted by Udayashankar et al[8] showed a 63 % decrease in dose using 80 mAs for 1-21 years for ventriculo-peritoneal shunt follow up cases. Whereas, a study conducted by Alice B Smith et al[6] showed a 55 % reduction in dose using z axis modulation and 25 % deceased dose using x-y-z axis modulation. For majority systems the maximum and minimum mAs values used differed by a factor of 3-4 consequently resulting in a dose difference by a factor of 2 or more for a CT brain examination[2]. The present study assessed the practicality of a low dose CT head protocol using a lower mAs according to age. Additionally the pitch was increased to 1 and rotation time was decreased to 0.5 ms. Even though a decrease in rotation time is assosciated with an increase in image noise as the “number of profiles for image reconstruction would reduce resulting in an need of increasing the radiation dose, a rotaion time of 0.5 ms should be used to achieve a balance between temporal and contrast resolutions and radiation dose”[10]. The mean effective dose using the low CT head protocol was found to be 1.7 mSv, 1.2mSv & 1.6 mSv for 1-4, 5-9 and 10-16 years respectively as compared to 4.6 mSv, 3.03mSv & 2.5mSv using the standard pediatric protocol[11]. The effective dose and DLP reported in the present study was found to be lower than the surveys conducted in UK[7], Switzerland [12] and Norway[13] as shown in table IV.
Table 4: Mean DLP and effective dose for various pediatric age groups in present work compared with data established in the literature.
|
Age |
Present study | Switzerland (12) | UK(7) | Norway(13) | ||||
| DLP
mGy*cm |
ED
mSv |
DLP
mGy*cm |
ED
mSv |
DLP
mGy*cm |
ED
mSv |
DLP
mGy*cm |
ED
mSv |
|
| 1-4 years | 261 | 1.7 | 332 | – | 270 | – | – | – |
| 5-9 years | 312 | 1.2 | 451 | – | 470 | – | 408 | 1.5 |
| 10-16 years | 523 | 1.6 | 805 | – | 620 | – | 511 | 1.8 |
However, a reduction in radiation dose is not the only outcome when exposure parameters are adjusted. There is also a significant decrease in image quality. In the present study, analysis of image quality was done qualitatively using a 4 point scoring scale. Even though none of the low dose head CT studies was graded diagnostically unacceptable, a clinically significant amount of subjects in age groups of 1-4 years and 5-9 years were scored with suboptimal image quality in terms of “noise and image acceptability” [figure 2, 3, &4]. A similar study conducted by Udayashankar et al[8] showed excellent image quality for 80 mAs using a 5 point scoring system. The image quality was also measured quantitatively for image noise by measuring the standard deviation of the pixel values by placing ROIs in 4 different locations. However, the image quality was mainly evaluated based on visualisation of ventriculoperitoneal shunt.
 |
Figure 2: Images of non -enhanced head CT in a 2 year old child at 250 (A) and 80(B) mAs. |
 |
Figure 3: Images of non -enhanced head CT in a 6 year old child at 250 (A) and 100(B) mAs. |
 |
Figure 4: Images of non -enhanced head CT in a 15 year old child at 250 (A) and 150(B) mAs. |
The increase in image noise in our study among 1-4 year and 5-9 year age group could be due to the lower mAs settings. However, it is suggestible to use lower mAs for cases where diagnosis has already been made, such as in follow up cases. Lower noise levels and thus higher doses are required to depict and characterize low contrast structures.Hence, an increase in mAs by a factor of 20 in the lower age groups can drastically improve the diagnostic quality of the image on our machine with only a minimal increase in dose (approximately 0.3 mSv) . Using advacned filters developed to reduce noisy images can also be adopted to solve this problem. A study conducted by Abidin et al [14] introduced a newer noise filterning technique called as Extreme learning machines (ELM method) that showed an efficient way to detect noisy pixels. Utilizing these filter techniques can help in reducing mAs without degrading image quality. Moreover, a study conducted by Cho-yin Chan et al showed that an mAs of 125-150 might be optimum level for pediatric [1-12 years] brain CT[2]. A few images were graded suboptimal with respect to gray white matter differentiaton for 1-4 years. However, it is known that the brain in < 2 years pediatric subjects are in the phase of development resulting in an incomplete myelination of white matter. Therefore to get good grey white matter differentiation there should be adequate myelination which has more water content. So, lack of grey white matter differentiation should not be considered as an quality criteria for patients <2 years. The study had various limitations which included a smaller sample size as the study was time bound. Also image quality was not evaluated quantitavily. Therefore, we could not correlate the objective image noise with subjective image quality. Nowdays scanners are equipped with lots of advanced softwares such as, 3D dose modulation, I dose and filtering techniques that help in maintaing the image quality when attempting to reduce the radiation dose. However the present study could not make use of these, due to its unavalability. Since there are a lot of centers or short set up diagnostic centers that might not be having these advanced softwares, developing age-specific pediatric protocols can definitely reduce the radiation dose significantly without compromising diagnostic accuracy in pediatric CT brain.
Conclusion
Our research has shown that developing age-specific pediatric protocols results in a significant decrease in effective dose without compromising diagnostic accuracy in pediatric CT brain. The present study showed a 71 %, 59% and 37% decrease in radiation dose for 1-4 years, 5-9 years and 10 -16 years respectively with acceptable image quality using age specific low dose protocol.
Acknowledgements
The authors would like to acknowledge the Institute research MCHP and ethics committee, Kasturba hospital for their support to undertake this study. We also extend our heartfelt gratitude to the faculties and Head of the department of Radio-diagnosis and imaging for their cooperation during data collection. We also acknowledge the support of department of Statistics for the guidance during data analysis and interpretation.
References
- Nations U, Scientific Committee. Sources And Effects Of Ionizing Radiation United Nations Scientific Committee on the Effects of Atomic Radiation. Vol. I. 2010. 1-2454
CrossRef - Chan CY, Wong YC, Chau LF, Yu SK, Lau PC. Radiation dose reduction in paediatric cranial CT. Pediatr Radiol. 1999;29(10):770–5.
CrossRef - Brenner DJ, Elliston CD, Hall EJ, Berdon WE. Estimated Risks of Radiation-. Ajr. 2001;176(2):289–96.
CrossRef - Hwang JY, Do KH, Yang DH, Cho YA, Yoon HK, Lee JS, et al. A survey of pediatric CT protocols and radiation doses in South Korean hospitals to optimize the radiation dose for pediatric CT scanning. Med (United States). 2015;94(50):1–9.
CrossRef - Mulkens T, Salgado R, Bellinck P. Dose Optimization and Reduction in CT of the Brain and Head and Neck Region. Radiation Dose from Multidetector CT. 2012. 135-151 p.
CrossRef - Smith AB, Dillon WP, Lau BC, Gould R, Verdun FR, Lopez EB, et al. Radiation dose reduction strategy for CT protocols: successful implementation in neuroradiology section. Radiology [Internet]. 2008;247(2):499–506.
CrossRef - P C Shrimpton, M C Hillier,M A Lewis MD. Doses from Computed Tomography (CT) Examinations in the UK – 2003 Review. Natl Radiol Prot Board [Internet]. 2005;57(March):1–107.
- Arvaniti M, Tudorascu D, Small WC, Little S. Low-Dose Nonenhanced Head CT Protocol for Follow-Up Evaluation of Children with Ventriculoperitoneal Shunt : Reduction of. 2008;802–6.
CrossRef - McNitt-Gray MF. AAPM/RSNA Physics Tutorial for Residents: Topics in CT Radiation Dose in CT1. Radiographics. 2002;22(6):1541–53.
CrossRef - Al Mahrooqi KMS, Ng CKC, Sun Z. Pediatric computed tomography dose optimization strategies: A literature review. J Med Imaging Radiat Sci . 2015;46(2):241–9.
CrossRef - Panakkal N, Yadav S, Dkhar W. Comparison of effective dose between adult and pediatric CT brain using dose length product. Int J pharma Biosci. 2015;6(4):37–42.
- Verdun FR, Gutierrez D, Vader JP, Aroua A, Alamo-Maestre LT, Bochud F, et al. CT radiation dose in children: A survey to establish age-based diagnostic reference levels in Switzerland. Eur Radiol. 2008;18(9):1980–6.
CrossRef - Friberg E. Doses from pediatric CT examinations in Norway Are pediatric scan protocols developed and in daily use? 2008;(1):1–9.
- Abidin Ç, Ulus Ç. An efficient noisy pixels detection model for CT images using extreme learning machines. Technical Gazette 25.2018:3:679-686.
CrossRef








