Thorax Cardiac Vascular and Endovascular Surgery Division, Department of Surgery, Udayana University / Sanglah General Hospital, Denpasar, Bali, Indonesia
Corresponding Author E-mail : ketut.putuyasa07@gmail.com
DOI : https://dx.doi.org/10.13005/bpj/1864
Abstract
Dialysis Related Steal Syndrome (DRESS) is one of the most terrible complications of arteriovenous fistula (AVF) creation that can produce hand ischemia. There are several methods to treat DRESS suitable regarding to the causes and conditions. DRESS present in a male 57 years old, with chief complain complain numbness and pain at rest on finger 4th and 5th left hand, weakness on hand grip after 2 weeks left brachial-basilic AVF creation for hemodialysis access. Physical examination there was found absent distal pulse of radial and ulnar artery, coldness on palmar and dorsal hand. Angiogram revealed preferential blood flow to brachio-basilic AVF access was detected with relative enlarge size of basilic vein without adequate blood flow to distal artery below the AVF. Double plication of basilic vein near the anastomosis brachial-basilic AVF was performed. Immediate gradual symptom resolution after plication and complete resolution was achieve in 1 month postoperative. Double plication of basilica vein of brachio-basilic AVF is effective treatment for DASS
Keywords
AVF; Dialysis Access; Plication; Steal Syndrome
Download this article as:| Copy the following to cite this article: Yasa K. P. Double Plication of Basilic Vein of Brachial-Basilic Arteriovenous Fistula as Effective Treatment for Dialysis Related Steal Syndrome (DRESS) : A Case Report . Biomed Pharmacol J 2020;13(1). |
| Copy the following to cite this URL: Yasa K. P. Double Plication of Basilic Vein of Brachial-Basilic Arteriovenous Fistula as Effective Treatment for Dialysis Related Steal Syndrome (DRESS) : A Case Report . Biomed Pharmacol J 2020;13(1). Available from: https://bit.ly/3aO9gAK |
Introduction
Overall incidence of steal syndrome in AVF is 1% to 9%, but can produce devastating complication hand ischemia (1), this frequency increases depending on the type of AVF (2, 3), and were predominantly (83%) brachial based (4).
There were several different term for hand ischemia related to vascular access such as hemodialysis access-induced distal ischaemia or HAIDI (3), distal hypoperfusion ischemic syndrome or DHIS (5), dialysis associated steal syndrome or DASS (6), arteriovenous access ischemic steal in hemodialysis or AVAIS (7), vascular access-induced steal syndrome or VASS (8), ischemic steal syndrome (ISS) associated with arteriovenous access (9).
Steal syndrome related to dialysis in AVF occurs when perfusion from the distal portion of the AVF become insufficient caused by more blood flowing towards the fistula than to the distal portion of the AVF , blood being diverted to support the access. It is one the most dreadful complications of vascular access creation. Diagnosis of steal syndrome related to dialysis is primarily clinical based on signs and symptoms of hand ischemia include pallor, absent distal pulse, coldness, pain, paraesthesia over hand and finger, weakness on hand grip, tissue loss such as ulcer or gangrene of fingers (6). Understand about pathophysiology is very importan for making diagnosis, investigation and management. Steal syndrome clinically is not simply blood diversion but also pressure changes within intravascular of distal portion of AVF to produce hypoperfusion and resultant poor perfusion pressures in the distal extremity (7).
There are several methods for treating DRESS in accordance with the different causes and conditions such as : endovascular treatment for peripheral arterial disease, plication with or without banding of venous segmen enlargement of AVF, ligation of outflow veins branches, revision using distal inflow (RUDI), proximalization of arterial inflow (PAI), distal revascularization and interval ligation (DRILL) or without interval ligation (6).
Case
A Male 57 years old, complain numbness and pain at rest on finger 4th and 5th left hand, weakness on hand grip after 2 weeks left brachial-basilic AVF creation for hemodialysis access. Physical examination there was found absent distal pulse of radial and ulnar artery, coldness on palmar and dorsal hand. There was no history of diabetes, coronary artery diseases, and cerebrovascular diseases. Chronic kidney disease (CKD) was diagnosed with routine hemodialysis 2 times a week, and Dialysis Associated Steal Syndrome (DASS) was supected. Internal jugular temporary catheter was inserted for hemodialysis vascular access. Catheter-directed angiography was performed to investigate any causes of DASS. Preferential blood flow to brachio-basilic AVF access was detected with relative enlarge size of basilic vein without adequate blood flow to distal artery below the AVF (Figure 1). Visible enlargement of basilic vein size (> 6 mm), and palpable strong thrill (Figure 3). Double plication of basilic vein near the anastomosis brachial-basilic AVF was performed under local anesthesia using Satinsky vascular clamp, double mattress and continuous suture with prolene until it reaches the desired size (double plication) (Figure 4 and Figure 5). The angiogram after plication show that arterial blood flow to distal was came back to normal (Figure 2), with significant palpable pulse of radial and ulnar artery. Immediate gradual symptom resolution after plication and complete resolution was achieve in 1 month postoperative.
 |
Figure 1: Preferential blood flow to brachial-basilic AVF before plication of basilic vein |
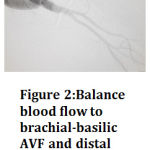 |
Figure 2: Balance blood flow to brachial-basilic AVF and distal artery after plication of basilic vein |
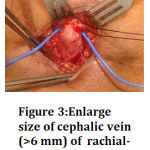 |
Figure 3: Enlarge size of cephalic vein (>6 mm) of rachial-cephalic AVF Click here to View figure |
 |
Figure 4: Satinsky clamping of cephalic vein brachial-cephalic AVF |
 |
Figure 5 : Double plication of cephalic vein of brachial-cephalic AVF |
Discussion
The severity of hand ischemia affects its management of DRESS. In grade 1 (mild) with few symptoms cool of extremity, no treatment needed. In grade 2 (moderate) with symtoms of intermittent claudication during dialysis, intervention sometimes needed. In grade 3 (severe) with symptoms of ischemic pain at rest or tissue loss, intervention is mandatory (6). In our case was classified as grade 3 (severe), therefore intervention was mandatory.
Others classification of haemodialysis access-induced distal ischemia was based on time onset after AVF creation, classified as ‘acute’ is less than 24 hours, ‘subacute’ is within 1 month or ‘chronic’ is over than 1 month (3). The other one classification is early, when less than 30 days or late when 30 or more day presentation (10). In our case was subacute, with symptoms occurs in 2 weeks after autogenous brachial-basilic AVF creation. As same as others report that subacute hemodialysis access-induced distal ischemia is 4 times more in autogenous AVF than grafts. Otherwise chronic onset was 91% more common in autogenous AVF and AVF creation in the cubital segment. In contrast, acute onset was 88% correlated with non-autogenous AVF (3).
Treatment strategy of DRESS depends on the causes, severity, and general condition (6). In our case the cause is high flow fistula access because in angiogram, the contrast preference flow toward fistula, without any signs of distal arterial obstructive disease. The criteria of high flow AVF is when flow as much as 1000-1500 ml/minute (2). In brachial-cephalic cubital AVF with steal syndrome there was significant higher volume flows were seen into venous segment fistula compared to those without steal (11). The principal treatment of high flow AVF are increased the resistance and reduced the flow into large lumen venous fistula. There are several methods can be used such as plication of venous segment near the anastomosis AVF, PTFE banding, or minimally invasive limited ligation endoluminal-assisted revision (MILLER) banding (2,6). Reverse of the limb ischemia symptoms and preserving the vascular access, are the goal of DRESS management (6). Success rate of distal revascularization-interval ligation (DRIL) procedure was 83% to 100%, therefore in many center it has become the preferred method to treat steal syndrome (1). Most patients with normal/high-flow AVFs with or without distal peripheral arterial disease, DRILL is effective as treatment (2), especially in patients who can tolerate a major operation (12). However, this operation was complex procedure.
The reports regarding plication of an AVF to treat ischemic steal syndrome was limited (1). There are reports about efficacy of plication to treat Ischemic steal syndrome with pathologic high flow and revealed good durability. It was reported that assisted primary patency was 87% at 1 year and 69% at 3 years, secondary patency was 90% at 1 year and 73% at 3 years (4). Plication should be considered as an alternative treatment before performance of a DRILL procedure, and may be an effective treatment to treat steal syndrome (1), because DRILL was the most frequent choice for late intervention (9). In our case we performed double plication with immediate gradual symptom resolution and complete resolution was achieve in 1 month postoperative. Narrowing of the vein lumen of AVF longitudinally, has a goal to reduce blood flow towards the fistula and improve circulation to the distal forearm (13).
References
- Yaghoubian A and de Virgilio C. Plication as Primary Treatment of Steal Syndrome in Arteriovenous Fistulas. Ann Vasc Surg, 2009 ; 23 :103-7.
CrossRef - Tordoir J.H.M, Dammers R, van der Sande F.M. Review : Upper Extremity Ischemia and Hemodialysis Vascular Access. Eur J Vasc Endovasc Surg, 2004 ; 27:1–5.
CrossRef - Scheltinga M.R, van Hoek F, Bruijninckx C.M.A. Time of onset in haemodialysis access-induced distal ischaemia (HAIDI) is related to the access type. Nephrol Dial Transplant, 2009 ; 24: 3198–3204.
CrossRef - Loh T. M, Bennett M.E, Peden E. K. Plication of Arteriovenous Access for Ischemic Steal Syndrome and Pathologic High Flow, Durable and Effective. Journal of Vascular Surgery (Supplement), 2015 : 144S.
CrossRef - Leon C and Asif A. Arteriovenous Access and Hand Pain: The Distal Hypoperfusion Ischemic Syndrome. Clin J Am Soc Nephrol. 2007 ; 2: 175–183.
CrossRef - Ho J. P. Prevention, Diagnosis and Management of Steal Syndrome. In : Ho J.P, Cho K. J, Ko P. J, Chu S.Y, Gopinathan A., editors. Practical Guide to Surgical and Endovascular Hemodialysis Access Management. Singapore : World Scientific Publishing Co. Pte. Ltd. 2016 : 179 – 204.
CrossRef - Inston N, Schanzer H, Widmer M, Deane C, Wilkins J, Davidson I, Gibbs P, Zanouw J, Bourquelot P, Valenti D. Arteriovenous access ischemic steal (AVAIS) in haemodialysis: a consensus from the Charing Cross Vascular Access Masterclass 2016. The Journal of Vascular Access, 2016 ; 18 (1) : 3-12. https://doi.org/10.5301/jva.5000621
CrossRef - Berman S.S. Understanding Steal Syndrome: Causes and Prevention Strategies to prevent the development of significant VASS. ENDOVASCULAR TODAY, 2009 : 70-72
- Gupta N, You T.H, Konig IV G, Dillayou E, Leers S. A, Chaer R.A, Cho J.S, Makaroun M.S. Treatment strategies of arterial steal after arteriovenous access. J Vasc Surg,, 2011 ; 54 : 162-7.
CrossRef - Zamani P, Kaufman J, Kinlay S. Ischemic steal syndrome following arm arteriovenous fistula for hemodialysis. Vascular Medicine, 2009 ; 14: 371–376.
CrossRef - Bavare C.S, Bismuth J, El-Sayed H.F, Huynh T.T, Peden E.K, Davies M.G, Lumsden A.B, Naoum J.J. Volume Flow Measurements in Arteriovenous Dialysis Access in Patients with and without Steal Syndrome. International Journal of Vascular Medicine, 2013.
CrossRef - Leake A.E, Winger D.G, Leers S.A, Gupta N, Dillavou E.D. Management and outcomes of dialysis access-associated steal syndrome. J Vasc Surg, 2015 ; 61:754-61.
CrossRef - Stolic R.V, Mijailovic M.Z, Cvetcovic A.M, Stanojevic M.S, Stolic D.Z, Cvetcovic D.M. Distal ischemia induced by vascular access for hemodialysis – a case report. HIPPOKRATIA, 2012 ; 16 (4) : 375-377.








