Manuscript accepted on :31-Jan-2020
Published online on: 11-02-2020
Plagiarism Check: Yes
Reviewed by: Hendry Irawan
Second Review by: Vikrant Rai
Final Approval by: Dr. Mohamed Abdel-Daim
Naveen Chandran1 , Nitin V Muralidhar1, Suma S1, Prathibha Shashikumar2 and Raghunath N1
, Nitin V Muralidhar1, Suma S1, Prathibha Shashikumar2 and Raghunath N1
1Department of Orthodontics, JSS Dental College and Hospital, Jssaher, Mysuru
2Department of Periodontics, JSS Dental College and Hospital, JSSAHER, Mysuru
Corresponding Author E-mail : 5247.naveen@gmail.com
DOI : https://dx.doi.org/10.13005/bpj/1872
Abstract
Long treatment duration is the main drawback of orthodontic treatment. Biostimulation with low-intensity laser therapy (LILT) is a non invase method of accelerating tooth movement. This study aims to test the efficacy of LILT in decrowding lower anteriors in self-ligating and conventional MBT bracket systems.The study group comprised of 32 subjects between age 14 to 25 and Littles index 4 to 6 allotted to two groups, Group I consist of subjects with conventional MBT brackets and Group II consists of patients with self-ligating brackets. Group I and II are further subdivided into subgroups; Group Ia, Group Ib, Group IIa and Group IIb. Groups Ia and IIa served as test groups undergoing photobiomodulation and groups Ib and IIb served as control. Biostimulation was done using diode laser till lower anterior decrowding is achieved. There is an increase in the rate of decrowding in self-ligating brackets by 20% and conventional brackets by 15.6%. Photobiomodulation with LILT is an effective means of decrowding lower anteriors.
Keywords
Bennett and Trevisi; Low Level Laser Therapy; Low Intensity Laser Therapy; Maclaughlin
Download this article as:| Copy the following to cite this article: Chandran N, Muralidhar N. V, Suma S2, Shashikumar P, Raghunath N. Comparing the Effect of Low-Intensity Laser Therapy (LILT) In Decrowding Lower Anteriors Using Conventional and Self-Ligating MBT Bracket Systems - An In Vivo Study. Biomed Pharmacol J 2020;13(1). |
| Copy the following to cite this URL: Chandran N, Muralidhar N. V, Suma S2, Shashikumar P, Raghunath N. Comparing the Effect of Low-Intensity Laser Therapy (LILT) In Decrowding Lower Anteriors Using Conventional and Self-Ligating MBT Bracket Systems - An In Vivo Study. Biomed Pharmacol J 2020;13(1). Available from: https://bit.ly/31KE0ij |
Introduction
Orthodontic treatment is a type of care which often involves pre-adolescents, adolescents and adult who requires higher compliance due to long treatment duration1. Reduction in active treatment time can result in a reduction in patient discomfort and fatigue and improve patient compliance. In long term treatment, there is an increased risk of root resorption, gingival inflammation and dental caries. Reducing orthodontic treatment time requires increasing the rate of tooth movement2.
Leveling and aligning is done in the first phase of orthodontic treatment where crowding of the anterior segment is addressed and can take up to 8 months. Reduction decrowding time can be achieved by acceleration procedures like wilkodontics, piezocision, periodontal distraction, microosteo perforations, injection of an active form of vitamin D3, prostaglandins, PRP etc3. But these procedures are relatively invasive and produce collateral effects like pain and discomfort.
Photobiomodulation involving low-intensity laser therapy (LILT) does not involve invasive methods but rather depends upon exposure of tissues to therapeutic wavelengths of laser irradiation2. LILT in dentistry is an effective method to promote nerve regeneration, wound healing, bone repair, and modeling after surgery4,5. These effects are attributed to the biostimulatory effects of LILT on collagen synthesis, and also osteoblast and fibroblast proliferation and differentiation6, 7, 8.
Studies have proved the biomechanical advantages of self-ligating brackets in the initial leveling and aligning phase of treatment. Self-ligating brackets have several advantages over conventional brackets including greater patient comfort during treatment, fewer visits, overall shorter treatment time, improved anchorage stability, less need of extraction, reduced risk of enamel decalcification9 etc.
The results that have been reported in studies regarding the response of orthodontic tooth movement to self-ligating brackets are inconsistent. A study done by Abdul Wahab concluded that self-ligating brackets are not superior to conventional brackets in the initial leveling and alignment phase of orthodontic treatment10. On the contrary, study done by Vijaybhaskar Reddy had shown the effectiveness of self-ligating brackets in initial phase of orthodontic treatment11.
The purpose of this study was to examine whether biostimulation, with a low-intensity laser, could decrease the treatment duration of the leveling and aligning phase of orthodontic therapy using self-ligating and conventional bracket systems.
The objectives are
To compare the time taken for decrowding of lower anteriors with and without low-intensity Laser therapy in conventional MBT technique
To compare the time taken for decrowding of lower anteriors with and without low-intensity laser therapy in self-ligating MBT technique.
To compare the time taken for decrowding of lower anteriors between conventional MBT technique and self-ligating MBT technique.
Materials and Methods
In this study, subjects of the age group 12-25 years, irrespective of gender, were selected from the outpatients who required fixed orthodontic treatment in the Department of Orthodontics and Dentofacial Orthopaedics, JSS Dental College and Hospital, Mysore. A total number of 70 patients were screened for eligibility (Figure 1). 32 patients who were found eligible were included in the study. Signed informed consent was obtained, from the patients selected for the study ethical clearance, was obtained from the ethical committee of JSS dental college and hospital. The inclusion criteria were, Patients who required fixed orthodontic treatment with the age group of 14 to 25 years, Patients with Little’s irregularity index score ≥ 4 mm and ≤ 6 mm, Healthy periodontal tissues, no systemic diseases, no history of previous orthodontic treatment.
 |
Figure 1: Flow Chart of Study Design |
Patients who were under medical treatment that could interfere with bone metabolism, long term use of systemic corticosteroids, antibiotics, calcium channel blockers, periodontally compromised patient, gingivitis and untreated caries, evidence of bone loss were excluded from the study. Group I consist of 16 subjects with conventional MBT brackets and Group II consist of 16 subjects with self-ligating brackets. Group I and II are further subdivided into subgroups Group Ia, Group Ib, Group IIa and Group IIb, with 8 subjects in each subgroup. Groups Ia and IIa served as test groups undergoing photobiomodulation and Groups Ib and IIb served as control. MBT brackets were placed on Group I subjects and self-ligating brackets were placed on Group II subjects. At the beginning of the treatment (T0), the impression of the lower arch was taken, and casts poured. Littles Irregularity index12 score was noted, and the initial casts were coded and pooled (Figure 2a). Groups Ia and IIa were subjected to Low-intensity laser therapy (LILT).
 |
Figure 2a: Study Model and Intra Oral Photograph at T0 |
 |
Figure 2b: Study Model and Intra Oral Photograph at T1 |
For the laser irradiation, Gallium Aluminum Arsenide (GaAlAs) diode laser of 808 nm wavelength in a continuous wave of 8 J/cm2, and energy of 2 J per point was used. Laser irradiation was done on 0, 3rd, 7th, 14th day in the first month and in intervals of 15 days from the second month until the complete alignment was achieved. Each root was divided into two halves, cervical and apical. The laser device was used to irradiate each halves perpendicular to the root, from both buccal and lingual sides (Figure 3). So, there were four applications for each tooth with an exposure time of 1 minute per tooth.
 |
Figure 3: Points of Laser Application |
Groups Ia and IIa were subjected to photobiomodulation by LILT. Groups Ib and IIb served as controls. The patients were recalled every two weeks until the anterior decrowding was achieved. After the decrowding was achieved (T1), another impression was taken, coded and pooled (Figure 2b). The correction of crowding was considered complete when Little’s irregularity index12 score was down to ≤ 1. For irregularity indices >1 mm, the treatment was continued until complete resolution of crowding is achieved. The time elapsed from T0 to T1 was calculated in days in all the subgroups and analyzed.
Results
The mean age of the patients included in the study was 19.15 ± 2.26 yrs with mean little’s index of 4.90 ± 0.57. Independent sample t-test was performed for statistical analysis.
The mean number of days taken for decrowding lower anteriors in the conventional MBT control group is 99.7 ± 9.7 and in the laser group is 84 ± 11.22 which was significant (Table 1)(Graph 1).
Table 1: Comparison of mean between Group 1a and 1b
| Group Statistics | ||||||
| Groups | N | Mean | Std. Deviation | Std. Error
Mean |
Sig. (2-tailed) | |
| Days | Group I a | 8 | 84.0000 | 11.22497 | 3. 96863 | .010 |
| Group I b | 8 | 99.7500 | 9.72111 | 3. 43693 | ||
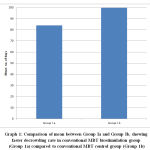 |
Graph 1: Comparison of mean between Group Ia and Group Ib |
The mean number of days taken for decrowding lower anteriors in the self-ligating control group is 91.87 ± 10.86 and in the self-ligating laser group is 73.5 ± 11.22 which was significant (Table 2)(Graph 2).
Table 2: Comparison of means between Group II a and Group II b
| Group Statistics | ||||||
| Groups | N | Mean | Std. Deviation | Std. Error Mean | Sig. (2-tailed) | |
| Days | Group II a | 8 | 73.5000 | 11.22497 | 3.96863 | .005 |
| Group II b | 8 | 91.8750 | 10.86853 | 3.84261 | ||
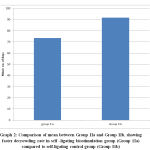 |
Graph 2: Comparison of mean between Group IIa and Group IIb |
The mean number of days taken for decrowding lower anteriors in the conventional MBT laser group is 84 ± 11.22 and in the self-ligating laser group is 73.5 ± 11.22 (Table 3)(Graph 3).
Table 3: Comparison of means between Group Ia and IIa
| Group Statistics | ||||||
| Groups | N | Mean | Std. Deviation | Std. Error Mean | Sig. (2-tailed) | |
| Days | Group I a | 8 | 84.0000 | 11.22497 | 3.96863 | .082 |
| Group II a | 8 | 73.5000 | 11.22497 | 3.96863 | ||
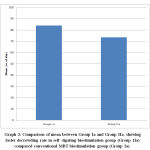 |
Graph 3: Comparison of mean between Group Ia and Group IIa |
Discussion
The Low-level laser beams in red and near-infrared regions correspond with the energy and absorption levels of the respiratory chain in mitochondria. The beams stimulate the antenna pigments, which are the photo acceptors of the respiratory chain, increasing the ATP production in mitochondria. This, in turn, increases the cellular metabolism and hence increases DNA synthesis and cell proliferation13. Setting up the optimal laser dosage level is important, as an excessive dose may inhibit tooth movement and an insufficient amount will produce no effect at all. Considering all the previous studies, irradiation by GaAlAs diode laser of 780-810 nm wavelength was found to accelerate the orthodontic tooth movement in a continuous wave of 5-20 J/cm2, 2-8 J was delivered to the tissue by contacting laser the tip to the gingival surface14.
In a study done by Limpanichkul, he tested the efficacy of GaAlAs laser on patients for maxillary canine retractions using coil springs on fixed edgewise appliance. He found no significant difference in the distal movement of canine between the test side and the control side at any time of the movement. The energy density of the irradiation that was used in this study (25 J/cm2) was probably not in the right quantity to express its stimulatory effect on the canine retraction rate15. Another study on canine retraction was done by Gauri Doshi-Metha using GaAlAs laser of 810 nm wavelength in continuous mode with power output of.25mW to determine the effect of laser biostimulation in canine retraction rate showed an increase in the rate of tooth movement by 30%16. Said A Samara and colleagues used an LED device with self-ligating brackets to decrowd lower anteriors on self-ligating brackets. The subjects used the device every day for 20 minutes till decrowding was achieved. They came out with the result that photobiomodulation decreased the decrowding time by 22%2. Our study was in agreement with these findings as we have attained acceleration of 20%, ie 1.25 times faster than the control group when self-ligation was used.
We are also in agreement with the study of Vijaybhaskar Reddy who had compared the efficiency of five different ligation systems over the duration of mandibular crowding alleviation and concluded that during initial levelling and alignment, self-ligating brackets were more efficient than conventional ligation brackets11.
The study consisted of two groups the first of which (Group I) included subjects with conventional 3M Gemini MBT brackets and second (Group II) included subjects with Damon Q self-ligating passive MBT brackets. Each group were further divided into two subgroups, in which one subgroup is irradiated with LILT (Groups Ia and IIa) and the other served as control. A total of 32 participants with a mean age of 19.15±2.26 yrs and mean Littles index of 4.90±0.57 were included in the study, with 8 participants each in all subgroups. The wire sequencing used for the treatment was .012 HANT, 0.014 HANT, 0.016 HANT, 0.017x.025 HANT, 0.018 SS , 0.019 x.025 HANT, 0.019 x.025 SS, 0.021X.025 TMA wires. The laser unit used for biostimulation was GaAlAs diode laser of 808 nm wavelength in continuous wave mode.
The mean number of days taken to decrowd lower anteriors in conventional MBT group with and without photobiomodulation with LILT was 84 days (SD 11 days) and 99.75 days (SD 9.7 days). This difference indicates that photobiomodulation by LILT increased the rate of decrowding by 15.6% in conventional brackets.
The mean number of days taken to decrowd lower anteriors in self-ligating MBT group with and without photobiomodulation with LILT was 73.5 days (SD 11.2 days) and 91.87 days (SD 10.8 days). This difference indicates that photobiomodulation by LILT increased the rate of decrowding by 20 % in self-ligating brackets.
On comparing conventional and self-ligating MBT groups which have undergone photobiomodulation with LILT, the self-ligating group with LILT has shown to decrowd lower anteriors 12.5% faster compared to conventional brackets with LILT. The mean number of days taken for decrowding was 73.5 days (SD 11.2 days) and 84 days (SD 11 days) respectively. The increase in the rate of decrowding of self-ligating brackets when compared with conventional brackets can be attributed to the self-ligation properties including light continuous force and reduced friction. This implies that self-ligating brackets are more efficient in the leveling and aligning phase of orthodontic therapy.
Conclusion
The use of LILT for photobiomodulation increases the rate of decrowding significantly and is an effective means of tooth movement acceleration. Self-ligating brackets are more efficient than conventional MBT brackets in initial leveling and aligning stage.
References
- Yao J, Li D-D, Yang Y-Q, McGrath CPJ, Mattheos N. What are patients Expectations of orthodontic treatment: a systematic review. BMC Oral Health.2016; 16(1):19.
CrossRef - Amer Z Nahas, Said A Samara, Tannaz A Rastegar ; Decrowding of lower anterior segments with and without photobiomodulation :a single centre randomized clinical trial. Laser and medical sciences January 2017, volume 32,129-135
CrossRef - Hassan AH, Al-Fraidi AA, Al-Saeed SH. Corticotomy-assisted orthodontic Treatment: review. Open Dent J. 2010; 4:159-64.
CrossRef - Hamblin M N, Demidova T. Mechanisms of Low Level Light Therapy. of SPIE 2006: 6140: 614001-1.
CrossRef - Pinheiro ALB, Soares LGP, Aciole GTS, et al. Light microscopic descriptionof the effects of laser phototherapy on bone defects grafted with mineral trioxide aggregate, bone morphogenetic proteins, and guided bone regeneration in a rodent model. J Biomed Mater Res A. 2011;98(2):212-221.
CrossRef - Basso FG, Pansani TN, Turrioni APS, Bagnato VS, Hebling J, de Souza Costaca. In vitro wound healing improvement by low-level laser therapy application in cultured gingival fibroblasts. Int J Dent. 2012;2012:719452.
CrossRef - Bicakci AA, Kocoglu-Altan B, Toker H, Mutaf I, Sumer Z. Efficiency of low-level laser therapy in reducing pain induced by orthodontic forces. Photomed Laser Surg. 2012;30(8):460-465.
CrossRef - Cepera F, Torres FC, Scanavini MA, et al. Effect of a low-level laser on boneregeneration after rapid maxillary expansion. Am J Orthod Dentofacial Orthop. 2012;141(4):444-450.
CrossRef - Prettyman, C.,Best, A. M., Lindauer, S. J., & Tufekci, E. (2012).Self-ligating vs conventional brackets as perceived by orthodontists. The Angle Orthodontist, 82(6), 1060–1066. doi:10.2319/101311-640.1
CrossRef - MegatAbdul Wahab, R., Idris, H., Yacob, H. & Zainal Ariffin, S. H. Comparison of self- and conventional-ligating brackets in the alignment stage. J. Orthod. 34, 176–181 (2012).
CrossRef - Vijaya bhaskara reddy, ashok kumar, mandava prasad, shivakumar nuvvula. a comparitive in -vivo evaluation of the alignment efficiency og 5 ligation methods : a prospective randomized clinical trial. J. Orthod. 8, 23–31 (2014).
- The Irregularity Index: A quantitative score of mandibular anterior alignment Robert M. little, D.D.S., M.S.D., Ph.D.Seattle, Wash. Am J Orthod 1975; 68:50-54.
CrossRef - Walsh LJ. The current status of laser applications in dentistry. Aust Dent J. 2003; 48(3):146-55; quiz 198.
CrossRef - Kim SJ, Chou MY, Park YG. Effect of low-level laser on the rate of tooth movement. Semin Orthod. 2015;21(3):210-218.
CrossRef - W Limpanichkul, K Gorey, N Srisuk, C Rattanayatikul. Effects of low-level laser therapy on the rate of orthodontic tooth movement. Orthod Craniofacial Res 9, 2006; 38–43.
CrossRef - Doshi-Mehta G, Bhad-Patil WA (2012) Efficacy of low-intensity laser therapy in reducing treatment time and orthodontic pain: a clinical investigation. Am J Orthod Dentofac Orthop 141:289–297.
CrossRef
List of Abbreviations
LLLT- low level laser therapy
LILT- low intensity laser therapy
MBT- Maclaughlin, Bennett and Trevisi
GaAlAs – Gallium Aluminum Arsenide
PRP-Platelet rich plasma







